Rotavirus remains one of the most common causes of severe diarrhea in infants and young children worldwide. While vaccines have significantly reduced its prevalence, outbreaks still occur—especially in daycare centers, hospitals, and regions with limited access to healthcare. Early diagnosis is crucial to prevent dehydration, reduce transmission, and ensure appropriate care. This guide details the symptoms, diagnostic tools, and clinical insights necessary to identify rotavirus quickly and effectively.
Understanding Rotavirus: Who Is at Risk?
Rotavirus primarily affects children between 6 months and 2 years of age, though older children and adults can also contract it—usually with milder symptoms. The virus spreads through the fecal-oral route, often via contaminated hands, surfaces, or objects. It’s highly contagious and can survive on surfaces for hours, making containment difficult in group settings.
Infants who are not vaccinated are at the highest risk. Those with weakened immune systems, malnutrition, or limited access to clean water face greater complications. In developing countries, rotavirus leads to hundreds of thousands of hospitalizations annually. Even in developed nations, seasonal spikes occur during winter and early spring.
Recognizing the Key Symptoms of Rotavirus
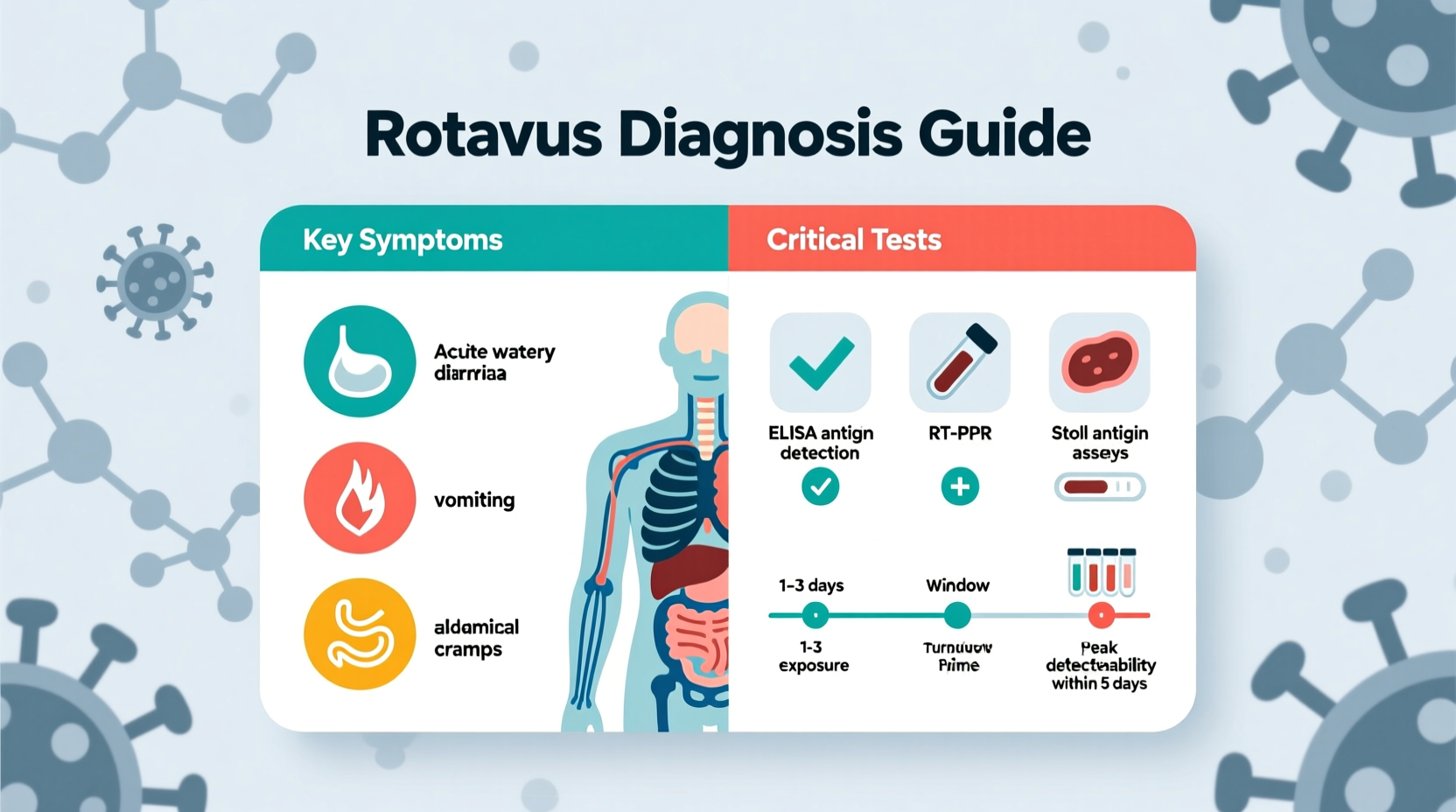
Symptoms typically appear 1–3 days after exposure and begin suddenly. The illness often starts with fever and vomiting, followed by watery diarrhea that can last 3 to 8 days. Unlike bacterial infections, rotavirus does not usually cause blood in the stool.
Common signs include:
- High fever (often above 102°F / 39°C)
- Frequent vomiting lasting 1–2 days
- Profuse, watery diarrhea (up to 20 episodes per day)
- Loss of appetite and fatigue
- Abdominal pain and cramping
- Signs of dehydration: dry mouth, reduced urination, sunken eyes, lethargy
In severe cases, especially in infants, dehydration can develop rapidly. Parents should monitor for decreased tear production, lack of wet diapers for more than six hours, and unusual drowsiness.
“Rotavirus infection can escalate from mild discomfort to life-threatening dehydration within hours in a small child. Recognizing early warning signs is half the battle.” — Dr. Lena Patel, Pediatric Infectious Disease Specialist
Essential Diagnostic Tests for Confirming Rotavirus
Clinical symptoms alone are not enough to confirm rotavirus, as many gastrointestinal illnesses present similarly. Laboratory testing is required for definitive diagnosis, particularly in outbreak investigations or hospitalized patients.
The most widely used method is the **enzyme immunoassay (EIA)**, which detects rotavirus antigens in stool samples. It’s fast, cost-effective, and highly sensitive, providing results within hours. Most hospital labs and clinics use this test routinely during peak season.
Other diagnostic options include:
- Reverse transcription-polymerase chain reaction (RT-PCR): Offers high sensitivity and can identify specific rotavirus strains—used mainly in research and surveillance.
- Latex agglutination: A rapid screening tool, though less sensitive than EIA.
- Electron microscopy: Rarely used due to complexity and cost, but historically important in virus identification.
Stool samples should be collected early in the illness, ideally within the first 48 hours of diarrhea onset, when viral shedding is highest. No special preparation is needed, but samples must be stored properly and transported promptly to avoid false negatives.
When Testing Is Recommended
Testing is not always necessary for otherwise healthy children with mild symptoms managed at home. However, it should be pursued in the following situations:
- Hospitalized patients with acute gastroenteritis
- Outbreaks in childcare facilities or long-term care centers
- Immunocompromised individuals with prolonged diarrhea
- Monitoring vaccine effectiveness in public health programs
Step-by-Step: How to Respond to Suspected Rotavirus Infection
If you suspect rotavirus in a child or vulnerable adult, taking timely action improves outcomes. Follow this sequence:
- Observe symptoms closely: Note frequency of diarrhea and vomiting, fluid intake, and any signs of dehydration.
- Begin oral rehydration: Use an oral rehydration solution (ORS) like Pedialyte. Avoid sugary drinks, fruit juices, or sports beverages.
- Contact a healthcare provider: Especially if symptoms persist beyond 24 hours, or if dehydration signs appear.
- Collect a stool sample if advised: Follow clinic instructions for proper collection and delivery.
- Isolate the patient: Prevent spread by limiting contact with others, especially in schools or group homes.
- Disinfect surfaces: Use bleach-based cleaners on toilets, changing tables, and toys.
Do’s and Don’ts When Managing Rotavirus
| Do | Don't |
|---|---|
| Offer small, frequent sips of ORS | Give plain water as the sole rehydration source |
| Continue breastfeeding or formula feeding | Stop feeding out of fear of vomiting |
| Use acetaminophen for fever control | Use anti-diarrheal medications in children under 2 |
| Wash hands with soap and water after contact | Rely solely on hand sanitizers (less effective against rotavirus) |
| Disinfect high-touch surfaces daily | Allow sick children to attend school or daycare |
Real-World Example: Outbreak in a Daycare Center
In early February, a daycare in the Midwest reported multiple cases of severe diarrhea among toddlers. Within three days, seven children were affected, and two required hospitalization for dehydration. Staff initially assumed it was a common stomach bug, but the speed and severity raised concerns.
Public health officials collected stool samples and confirmed rotavirus using EIA testing. Investigation revealed that one unvaccinated infant had recently returned from travel abroad. Poor hand hygiene among staff during diaper changes contributed to rapid spread.
The center implemented immediate isolation protocols, deep cleaning with bleach solutions, and parent education on symptoms and hydration. Vaccination status was reviewed for all children, and catch-up doses were recommended. No new cases emerged after one week, highlighting how prompt diagnosis and action can halt transmission.
Frequently Asked Questions
Can adults get rotavirus?
Yes, though it’s less common and usually milder. Adults may experience nausea, low-grade fever, and diarrhea, but severe dehydration is rare. Caregivers of infected children are at higher risk due to close contact.
Is the rotavirus vaccine effective?
Yes. The current vaccines (RotaTeq and Rotarix) prevent severe rotavirus illness in over 90% of recipients and have reduced hospitalizations by up to 80% in countries with routine immunization programs.
How long is a person contagious?
Individuals can shed the virus in their stool from two days before symptoms start to up to 10 days after recovery. In immunocompromised people, shedding may continue for weeks, even without symptoms.
Prevention: Vaccination and Hygiene
Vaccination is the most effective way to prevent severe rotavirus disease. The CDC recommends two or three doses of rotavirus vaccine, depending on the brand, administered at 2, 4, and sometimes 6 months of age. The vaccine is given orally and is safe for most infants.
While vaccination doesn’t guarantee complete immunity, it dramatically reduces the severity of illness. Alongside immunization, consistent hygiene practices are essential:
- Wash hands with soap and water after diaper changes and before eating
- Disinfect toys, surfaces, and changing areas regularly
- Keep sick children home until symptoms resolve
- Avoid sharing utensils, bottles, or pacifiers
Conclusion: Stay Informed, Act Early
Rotavirus is a preventable and manageable illness when diagnosed early and treated appropriately. Knowing the symptoms—especially sudden watery diarrhea and vomiting—and understanding when to seek testing can make a critical difference in outcomes. With vaccination, good hygiene, and prompt rehydration, families can navigate this common childhood illness safely.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?