Celiac disease affects approximately 1 in 100 people worldwide, yet many remain undiagnosed. This autoimmune disorder triggers intestinal damage when gluten—a protein found in wheat, barley, and rye—is consumed. Left untreated, it can lead to serious complications including malnutrition, osteoporosis, infertility, and even certain cancers. Recognizing the signs early, understanding diagnostic pathways, and knowing what to do after a diagnosis are critical for long-term health. This guide breaks down the key symptoms, explains how testing works, and outlines actionable steps to take control of your well-being.
Understanding Celiac Disease: More Than Just a Gluten Sensitivity
Celiac disease is not a food allergy or simple intolerance—it’s an autoimmune condition where the immune system attacks the small intestine in response to gluten. This damages the villi, tiny finger-like projections that absorb nutrients, leading to malabsorption and systemic issues. Unlike non-celiac gluten sensitivity (NCGS), which may cause discomfort without intestinal damage, celiac disease involves measurable physiological harm confirmed through blood tests and biopsy.
The condition has a strong genetic component, often linked to HLA-DQ2 and HLA-DQ8 genes. However, having these genes doesn’t guarantee disease development—environmental factors like infections, stress, or surgery can act as triggers.
“Celiac disease is one of the most common chronic gastrointestinal disorders, yet underdiagnosed due to its variable presentation.” — Dr. Alessio Fasano, Director, Center for Celiac Research and Treatment
Recognizing the Symptoms: Digestive and Beyond
Symptoms of celiac disease vary widely between individuals and age groups. While some experience classic digestive complaints, others present with seemingly unrelated issues. This variability contributes to delayed diagnosis, which averages 6–10 years from symptom onset.
Digestive Symptoms (More Common in Children)
- Chronic diarrhea or constipation
- Bloating and abdominal pain
- Nausea and vomiting
- Fatty, foul-smelling stools (steatorrhea)
- Weight loss or failure to thrive in children
Non-Digestive and Systemic Symptoms (Frequent in Adults)
- Fatigue and brain fog
- Anemia (especially iron-deficiency)
- Osteoporosis or recurrent fractures
- Mouth ulcers or dental enamel defects
- Skin rash known as dermatitis herpetiformis
- Joint pain and headaches
- Infertility or recurrent miscarriages
- Neurological symptoms like numbness or balance issues
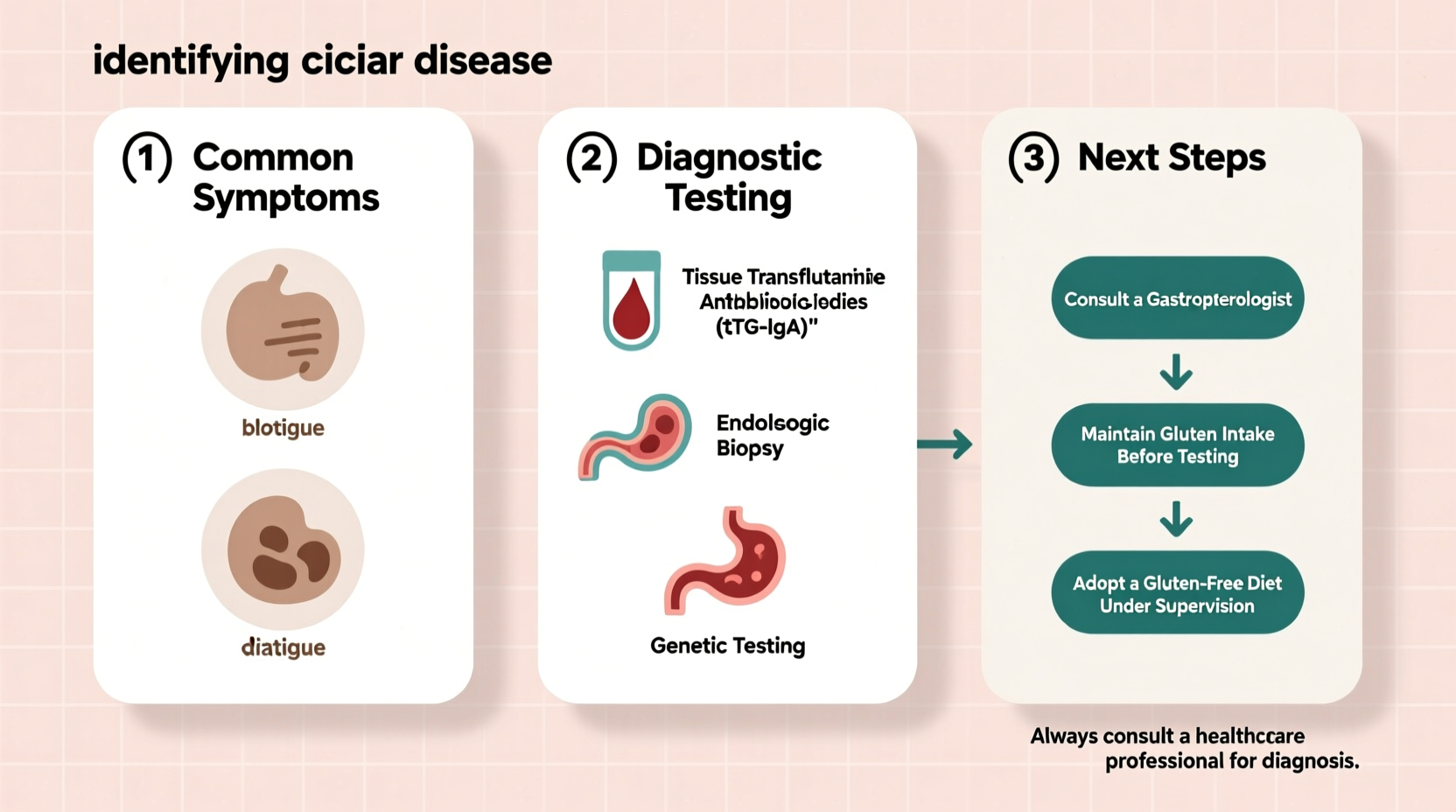
Testing for Celiac Disease: The Right Way to Diagnose
Accurate diagnosis requires specific blood tests and confirmation via endoscopy with biopsy. It’s crucial not to start a gluten-free diet before testing, as this can yield false-negative results.
Step-by-Step Diagnostic Process
- Continue consuming gluten: At least 2 slices of bread daily for 6–8 weeks prior to testing.
- Serology blood panel: Tests for antibodies indicating an immune reaction to gluten.
- Genetic testing (if needed): Rules out celiac if HLA-DQ2/DQ8 genes are absent.
- Endoscopic biopsy: Gold standard for confirming intestinal damage.
Common Blood Tests for Celiac Screening
| Test Name | What It Measures | Interpretation |
|---|---|---|
| tTG-IgA (Tissue Transglutaminase Antibody) | Primary antibody marker | High levels strongly suggest celiac; most sensitive test |
| EMA-IgA (Endomysial Antibody) | Highly specific for celiac | Positive result nearly confirms diagnosis |
| Total Serum IgA | Checks for IgA deficiency | Necessary because low IgA can cause false negatives on tTG-IgA |
| Deamidated Gliadin Peptide (DGP) IgA/IgG | Alternative marker | Useful in young children or IgA-deficient patients |
If blood work suggests celiac, an upper endoscopy is scheduled. During this procedure, a gastroenterologist takes multiple biopsies from the small intestine. The presence of villous atrophy—flattened or damaged villi—is definitive proof of celiac disease.
After Diagnosis: What Happens Next?
Receiving a celiac diagnosis can be overwhelming. The good news? A strict lifelong gluten-free diet allows the gut to heal and symptoms to resolve in most people. But success depends on adherence and support.
Action Plan After Confirmation
- Consult a registered dietitian: Work with someone specializing in celiac disease to learn label reading, avoid cross-contamination, and ensure nutritional adequacy.
- Review medications and supplements: Some contain hidden gluten; verify ingredients with your pharmacist.
- Monitor nutrient levels: Check for deficiencies in iron, B12, folate, vitamin D, calcium, and zinc.
- Educate family members: Encourage first-degree relatives to get tested, as risk is higher.
- Join a support group: Emotional and practical support helps long-term compliance.
Real-Life Example: Sarah’s Journey to Diagnosis
Sarah, a 34-year-old teacher, had struggled with fatigue, bloating, and iron-deficiency anemia for over five years. Doctors treated her symptoms individually—iron supplements, probiotics, antidepressants—but never connected the dots. After noticing her sister improved dramatically on a gluten-free diet post-celiac diagnosis, Sarah requested testing. Her tTG-IgA was elevated, and a biopsy confirmed stage 3b villous atrophy. Within three months of starting a strict gluten-free diet, her energy returned, anemia resolved, and she reported feeling “like herself again.” Sarah now advocates for broader awareness among primary care providers about celiac’s diverse presentations.
Frequently Asked Questions
Can I be tested for celiac disease if I’m already on a gluten-free diet?
Testing while avoiding gluten can produce false negatives. If you’ve already eliminated gluten, your doctor may recommend a gluten challenge—consuming gluten daily for several weeks before testing. Genetic testing can help determine if celiac is still possible.
Is a gluten-free diet healthy for everyone?
For those with celiac disease, it’s essential. But for others, unnecessary restriction can lead to lower fiber intake, reduced whole grains, and potential nutrient gaps. Gluten-free processed foods are often higher in sugar and fat. Unless medically necessary, focus on balanced eating rather than eliminating gluten.
How long does it take to feel better after going gluten-free?
Many people report improvement within days to weeks. However, full intestinal healing can take months to years, especially in adults. Children typically heal faster—within 6 to 12 months.
Conclusion: Take Charge of Your Health
Identifying celiac disease begins with recognizing subtle or persistent symptoms and seeking appropriate testing while still consuming gluten. Once diagnosed, a structured approach involving medical follow-up, dietary changes, and ongoing monitoring can restore health and prevent complications. Don’t dismiss recurring digestive issues, unexplained fatigue, or nutrient deficiencies—they may be signals worth investigating. With accurate diagnosis and proper management, people with celiac disease can live full, vibrant lives.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?