Back teeth—your molars and premolars—are workhorses. They grind food, endure pressure, and are more prone to decay due to their location and grooved surfaces. When they ache, the pain can be sharp, throbbing, or constant, interfering with eating, speaking, and sleep. Unlike front teeth, back teeth issues often go unnoticed until symptoms escalate. Understanding the root causes and knowing how to respond can prevent complications and preserve oral health.
Common Causes of Aching Back Teeth
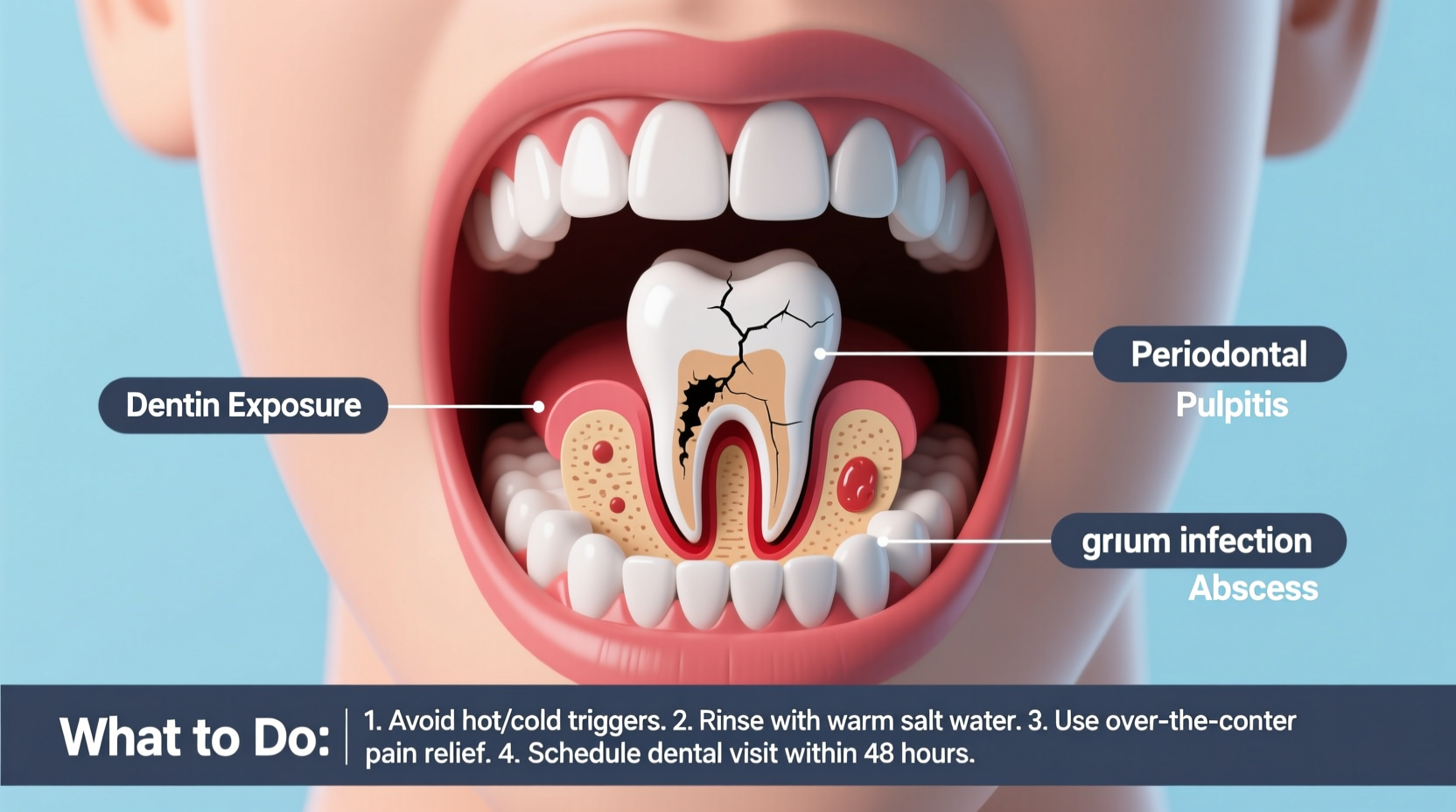
Pain in the back teeth isn't always due to a cavity. Multiple dental and non-dental factors may be responsible, some requiring immediate professional care.
- Tooth Decay (Cavities): Molars are especially vulnerable because food particles easily get trapped in their deep fissures. Untreated decay reaches the inner pulp, causing inflammation and pain.
- Dental Abscess: A bacterial infection at the tooth root or between the gum and tooth leads to pus buildup, swelling, and severe, pulsating pain that may radiate to the jaw or ear.
- Cracked or Fractured Tooth: Biting hard foods or grinding teeth can cause cracks. Pain may spike when chewing or exposed to temperature changes.
- Gum Disease (Periodontitis): Advanced gum infection erodes bone support around molars, leading to sensitivity, mobility, and dull, persistent aches.
- Impacted Wisdom Teeth: Third molars often don’t erupt properly, pressing against adjacent teeth and causing deep, radiating pain, swelling, and infection risk.
- Teeth Grinding (Bruxism): Chronic clenching or grinding wears down enamel and strains jaw muscles, resulting in soreness in the molars and surrounding areas.
- Sinus Pressure: The maxillary sinuses sit just above the upper molars. During sinus infections, pressure can mimic toothache, especially in multiple upper back teeth.
What You Can Do at Home (Temporary Relief)
While home remedies won’t fix underlying problems, they can reduce discomfort until you see a dentist.
- Rinse with Warm Salt Water: Mix ½ teaspoon of salt in 8 oz of warm water. Swish for 30 seconds twice daily to reduce inflammation and flush debris.
- Use a Cold Compress: Apply ice wrapped in a cloth to the outside of your cheek for 15 minutes to numb pain and reduce swelling.
- Over-the-Counter Pain Relievers: Ibuprofen or acetaminophen can temporarily ease pain. Follow dosage instructions and avoid placing aspirin directly on the gum (it can burn tissue).
- Clove Oil Application: Dab a cotton swab with clove oil (diluted with carrier oil like coconut) on the affected area. Eugenol in cloves acts as a natural anesthetic and antiseptic.
- Avoid Triggers: Stay away from extreme temperatures, sugary foods, and chewing on the painful side.
“Home remedies are stopgaps, not solutions. Delaying professional care risks irreversible damage like nerve death or tooth loss.” — Dr. Lena Torres, Endodontist
When to See a Dentist Immediately
Some symptoms require prompt evaluation. Ignoring them can lead to serious complications such as systemic infection or tooth extraction.
| Symptom | Urgency Level | Recommended Action |
|---|---|---|
| Severe, unrelenting pain lasting over 24 hours | High | See dentist within 24–48 hours |
| Swelling in face, jaw, or gums | Emergency | Seek immediate care—possible abscess |
| Fever accompanying tooth pain | High | Indicates spreading infection |
| Tooth feels loose or shifted | Moderate | Schedule appointment within a week |
| Pain when biting or chewing | Moderate | Could indicate crack or decay |
Mini Case Study: Delayed Care Leads to Complication
Mark, 34, experienced mild sensitivity in his lower left molar for two weeks. He used OTC painkillers and avoided chewing on that side. After three weeks, the pain intensified into a constant throb, and his jaw began to swell. He visited an emergency dental clinic and was diagnosed with a periapical abscess. The infection had spread to the jawbone, requiring root canal therapy and antibiotics. With earlier intervention, a simple filling might have sufficed. His delay turned a minor issue into a complex treatment.
Step-by-Step Guide: Responding to Back Tooth Pain
If you’re experiencing molar pain, follow this sequence to manage it effectively:
- Assess Symptoms: Note the type of pain (sharp, dull, throbbing), duration, triggers (heat, cold, pressure), and any swelling or fever.
- Practice Immediate Relief: Rinse with salt water, apply cold compress, take appropriate pain medication.
- Avoid Aggravating Habits: Stop chewing on the side, limit sugar, and refrain from smoking or drinking alcohol, which can worsen inflammation.
- Contact Your Dentist: Call for an appointment. Describe your symptoms clearly so they can prioritize urgency.
- Prepare for the Visit: Write down when the pain started, what makes it better or worse, and any medications you’re taking.
- Follow Through Treatment: Whether it’s a filling, crown, root canal, or extraction, complete the recommended plan to prevent recurrence.
Prevention Checklist
Protect your back teeth before problems arise. Use this checklist to maintain long-term molar health:
- Brush twice daily with fluoride toothpaste using a soft-bristled brush.
- Floss daily, especially behind the last molars where plaque accumulates.
- Use an antibacterial mouthwash to reduce gum disease risk.
- Schedule dental cleanings and checkups every six months.
- Ask your dentist about dental sealants for deep molar grooves (especially in children and teens).
- Wear a night guard if you grind your teeth.
- Avoid chewing ice, hard candy, or non-food items like pens.
- Limit sugary snacks and acidic drinks that promote decay.
Frequently Asked Questions
Can wisdom teeth cause pain in other molars?
Yes. Impacted or partially erupted wisdom teeth can push against adjacent molars, creating pressure, misalignment, and pain. They also trap bacteria, increasing decay and gum disease risk in neighboring teeth.
Is it possible to have a toothache without a cavity?
Absolutely. Cracks, gum recession, bruxism, sinus issues, and even referred pain from jaw joint disorders (TMJ) can mimic tooth pain. A dentist can perform tests to pinpoint the true source.
How long can I wait before seeing a dentist for molar pain?
If pain persists beyond 1–2 days despite home care, schedule an appointment. Lingering discomfort often indicates underlying damage that won’t resolve on its own. Early treatment saves time, money, and discomfort.
Final Thoughts: Take Action Before It Gets Worse
Back tooth pain is rarely trivial. While occasional sensitivity might fade, consistent or worsening ache signals a condition needing attention. From cavities to abscesses, the causes vary in severity—but the solution starts the same way: a visit to your dentist. Preventive habits, timely care, and awareness of warning signs empower you to protect your smile and overall health. Don’t wait for the pain to become unbearable.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?