Many people experience persistently cold hands and feet, especially in cooler environments. While occasional chilliness is normal, consistently cold extremities may signal underlying health issues or lifestyle factors affecting circulation. Understanding the root causes and knowing when to take action can help restore warmth, improve comfort, and even prevent complications. This guide explores the science behind cold extremities, identifies key contributors, and provides actionable solutions.
Why Do Hands and Feet Get Cold?
The human body prioritizes core temperature over extremities. When exposed to cold, blood vessels in the hands and feet constrict—a process called vasoconstriction—to reduce heat loss and maintain internal organ function. However, some individuals experience exaggerated or prolonged vasoconstriction, leading to chronically cold limbs even in mild conditions.
Blood flow regulation involves a complex interplay between the nervous system, hormones, and vascular health. Conditions that impair circulation or alter autonomic responses can disrupt this balance, making hands and feet feel cold without apparent cause.
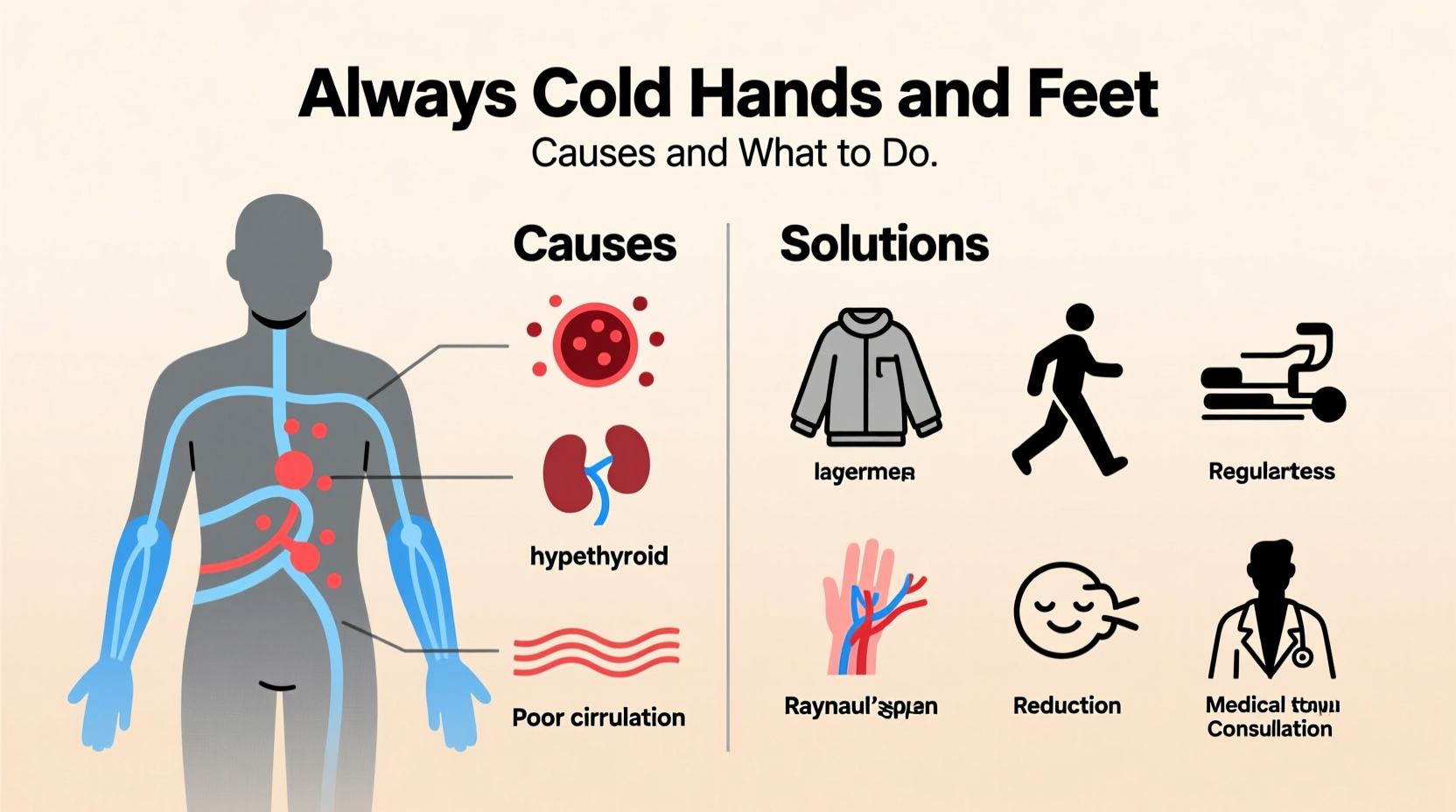
Common Medical Causes of Cold Extremities
Persistent cold hands and feet are not always due to low room temperature. Several medical conditions can contribute:
- Anemia: Low red blood cell count reduces oxygen delivery and impairs heat production.
- Hypothyroidism: Underactive thyroid slows metabolism, reducing body heat generation.
- Raynaud’s Phenomenon: A condition where small arteries spasm excessively in response to cold or stress, drastically reducing blood flow to fingers and toes.
- Peripheral Artery Disease (PAD): Narrowed arteries limit blood flow to limbs, often accompanied by pain during activity.
- Diabetes: Nerve damage (neuropathy) and poor circulation from high blood sugar can affect temperature sensation and regulation.
- Autonomic Dysfunction: Disorders like POTS or Parkinson’s can disrupt the nervous system’s control over blood vessel tone.
“Cold hands and feet aren’t just uncomfortable—they can be an early warning sign of circulatory or metabolic issues.” — Dr. Lena Torres, Vascular Neurologist
Lifestyle and Environmental Triggers
Even without diagnosed illness, daily habits can contribute to cold extremities:
| Factor | Impact on Circulation | Solution |
|---|---|---|
| Sedentary lifestyle | Reduces blood flow to extremities | Take movement breaks every hour |
| Caffeine and nicotine | Constrict blood vessels | Limit intake, especially in cold weather |
| Tight clothing or footwear | Restricts blood flow | Wear looser-fitting socks and shoes |
| Poor diet | Deficiencies in iron, B12, or folate impair circulation | Eat iron-rich foods and balanced meals |
| Dehydration | Reduces blood volume and flow efficiency | Drink adequate water daily |
Step-by-Step Guide to Warmer Hands and Feet
If you’re frequently reaching for gloves indoors or wearing multiple pairs of socks, follow this practical timeline to address the issue systematically:
- Week 1: Assess Your Habits
Track daily routines—note caffeine intake, physical activity, clothing choices, and when coldness occurs. Identify patterns. - Week 2: Improve Daily Circulation
Incorporate short walks, hand and foot exercises (like finger spreads and ankle circles), and elevate your legs periodically to encourage blood return. - Week 3: Optimize Diet and Hydration
Add iron-rich foods (spinach, lentils, red meat), vitamin B12 (eggs, dairy, fortified cereals), and omega-3s (salmon, flaxseeds). Drink at least 2 liters of water daily. - Week 4: Evaluate and Adjust Environment
Use space heaters if needed, wear layered clothing, and avoid sitting near drafts. Consider heated blankets or slippers during prolonged sitting. - Week 5: Consult a Healthcare Provider
If no improvement, request blood tests (CBC, TSH, iron panel) and discuss symptoms with your doctor to rule out anemia, thyroid issues, or Raynaud’s.
Real-Life Example: Managing Raynaud’s at Work
Sarah, a 34-year-old office worker, noticed her fingers turned white and numb every winter, especially in her air-conditioned workplace. After researching her symptoms, she realized she might have Raynaud’s phenomenon. She began keeping hand warmers in her desk, wore fingerless gloves lined with thermal fabric, and avoided icy drinks. She also spoke with her doctor, who confirmed mild Raynaud’s and recommended lifestyle adjustments. Within two months, her episodes decreased by 70%, and she no longer dreaded morning commutes.
This case highlights how identifying triggers and making small changes can yield significant improvements—even without medication.
When to Seek Medical Help
While cold extremities are often benign, certain warning signs warrant prompt evaluation:
- Fingers or toes turn blue or white and then red upon warming
- Pain, numbness, or tingling that interferes with daily tasks
- Sores or ulcers on fingertips or toes that heal slowly
- Symptoms occurring only on one side of the body
- History of autoimmune diseases like lupus or scleroderma
These could indicate secondary Raynaud’s or vascular disease requiring targeted treatment.
Prevention Checklist
Use this checklist to minimize cold hands and feet proactively:
- ✅ Dress in layers with thermal base layers in cold weather
- ✅ Wear insulated gloves and moisture-wicking socks
- ✅ Avoid smoking and limit caffeine
- ✅ Exercise regularly to boost circulation
- ✅ Manage stress through breathing techniques or meditation
- ✅ Maintain a balanced diet rich in iron and B vitamins
- ✅ Stay hydrated throughout the day
- ✅ Warm up hands and feet gradually after cold exposure
“Never ignore persistent coldness in extremities—especially if it’s new or worsening. Early intervention can prevent long-term vascular damage.” — Dr. Marcus Reed, Cardiologist
Frequently Asked Questions
Can anxiety cause cold hands and feet?
Yes. Anxiety activates the sympathetic nervous system, triggering vasoconstriction and redirecting blood away from extremities to vital organs. This “fight-or-flight” response can make hands and feet feel cold even in warm rooms.
Is it normal for young women to have cold hands and feet?
It’s common but not necessarily normal. Women, especially younger ones, are more prone due to lower muscle mass, hormonal fluctuations, and higher rates of anemia or Raynaud’s. However, chronic coldness should still be evaluated if disruptive.
Can medications cause cold extremities?
Yes. Beta-blockers, certain migraine medications (like ergotamines), and decongestants can constrict blood vessels as a side effect. If you suspect a medication is contributing, consult your doctor—do not stop taking it abruptly.
Take Action for Lasting Comfort
Always cold hands and feet may seem like a minor annoyance, but they can reflect deeper imbalances in circulation, metabolism, or nervous system function. By understanding the causes—from lifestyle choices to medical conditions—you gain the power to make informed changes. Start with simple adjustments: move more, dress appropriately, and monitor your symptoms. If problems persist, seek professional guidance. Small steps today can lead to warmer, healthier extremities tomorrow.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?