At first glance, compression socks and knee-high socks may look nearly identical—both extend from the foot to just below the knee, often come in neutral or athletic colors, and are worn during physical activity or long periods of sitting. But appearances can be deceiving. While they share a similar silhouette, their purpose, construction, and physiological impact are fundamentally different. Understanding these distinctions isn’t just about semantics; it’s about health, performance, and avoiding misconceptions that could lead to poor choices for circulation, recovery, or comfort.
How Compression Socks Work: More Than Just Tight Fabric
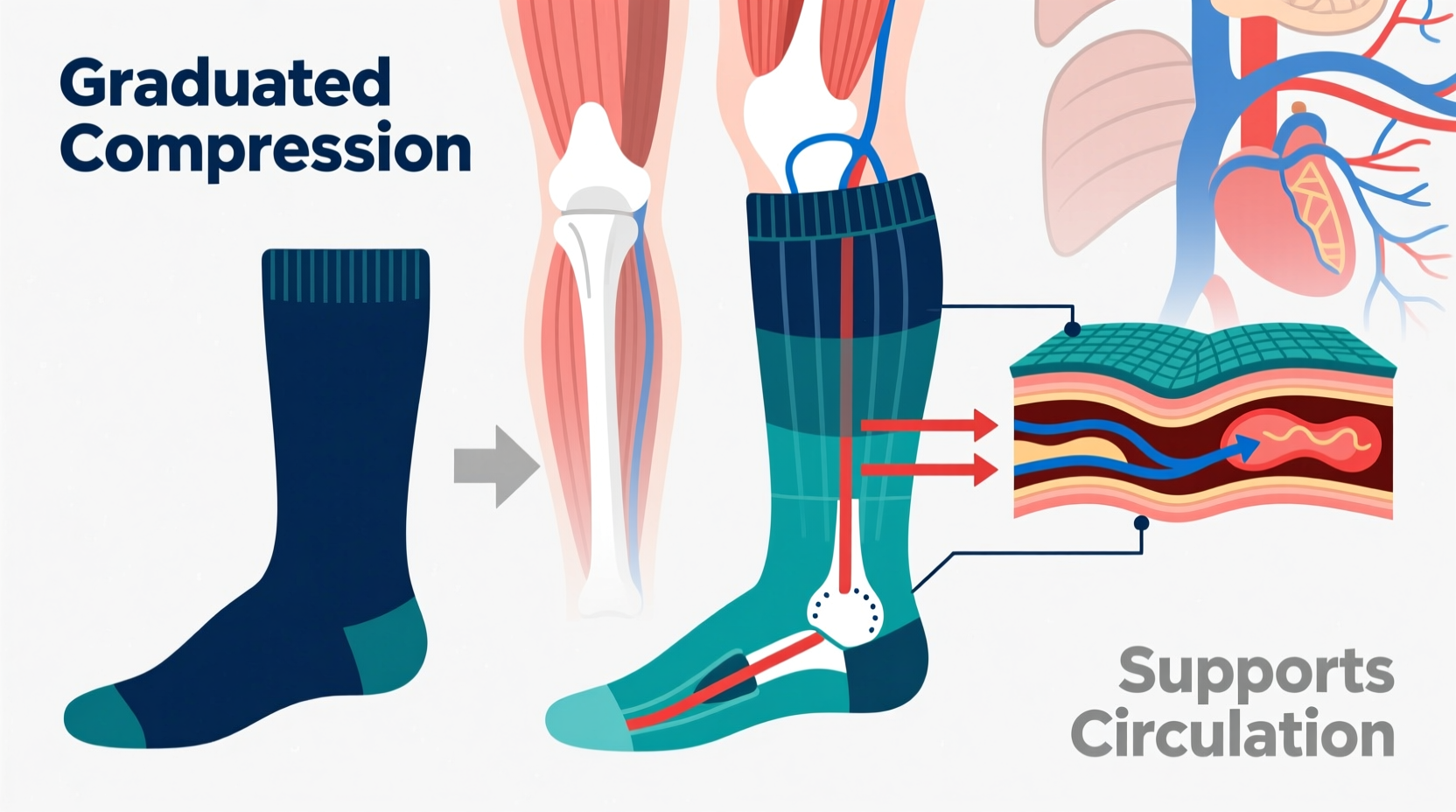
The core difference lies in how compression socks interact with your body. Unlike regular knee-high socks, which are designed primarily for warmth, fashion, or modesty, compression socks apply graduated pressure to the legs. This means they are tightest at the ankle and gradually loosen as they move up the calf. This gradient helps push blood upward toward the heart, counteracting the effects of gravity and improving venous return.
This mechanism is critical for people who spend long hours on their feet, sit during extended travel, or suffer from conditions like varicose veins, edema, or deep vein thrombosis (DVT). The pressure is measured in millimeters of mercury (mmHg) and categorized into levels:
- 15–20 mmHg: Mild compression, suitable for daily wear, travel, or mild swelling.
- 20–30 mmHg: Moderate compression, often recommended for post-surgery recovery or moderate venous insufficiency.
- 30–40 mmHg: Firm compression, typically prescribed for serious circulatory issues.
Regular knee-high socks do not offer this calibrated pressure. Their elasticity may provide a snug fit, but it’s uniform and not medically engineered.
Material and Construction: Engineered for Function
Compression socks are made from specialized blends of nylon, spandex, and microfiber, designed to maintain consistent pressure without losing shape. They often feature reinforced heels and toes, moisture-wicking properties, and anti-odor treatments—important for users wearing them for 8–12 hours a day.
In contrast, standard knee-high socks are usually made from cotton, wool, or basic synthetic fibers. These materials stretch and sag over time, especially after washing. They’re not built to sustain tension throughout the day, nor do they support muscle stabilization.
The weave and stitching in compression socks are also precision-engineered. Seams are flat to prevent chafing, and the fabric is denser around the ankle. Some brands incorporate targeted zones of support for the arch or Achilles tendon—features absent in traditional hosiery.
Medical Backing and Clinical Use
One of the most significant distinctions is the role of compression therapy in medicine. Compression socks aren't lifestyle accessories—they're clinically validated tools. According to the American Venous Forum, graduated compression therapy is a first-line treatment for chronic venous disorders, reducing symptoms like leg heaviness, cramping, and swelling by up to 60%.
“Compression therapy is one of the oldest and most effective forms of vascular care. It’s not a trend—it’s a treatment.” — Dr. Rebecca Tran, Vascular Medicine Specialist
Hospitals routinely prescribe compression socks after surgery to prevent blood clots. Airlines recommend them for long-haul flights due to the increased risk of DVT. Athletes use them to enhance recovery by reducing lactic acid buildup and minimizing muscle oscillation during runs.
Knee-high socks, while comfortable, have no such clinical endorsement. Wearing them instead of proper compression gear in high-risk situations could lead to avoidable complications.
Real-World Example: Travel and Swelling
Consider Sarah, a 42-year-old marketing executive who flies frequently. On a recent 14-hour flight, she wore her favorite black wool knee-highs for warmth. By landing, her ankles were visibly swollen, and she experienced throbbing discomfort—a common sign of fluid pooling due to inactivity.
Her doctor recommended trying 20–30 mmHg compression socks on her next trip. Skeptical but willing, she switched brands. This time, despite a similar flight duration, she reported minimal swelling and no leg fatigue. The difference wasn’t just comfort—it was measurable: her ankle circumference increased by only 0.3 cm versus 1.8 cm previously.
This case illustrates that while both sock types cover the same area, only compression wear actively supports circulatory function under stress.
Compression Socks vs. Regular Knee-Highs: A Comparison
| Feature | Compression Socks | Regular Knee-High Socks |
|---|---|---|
| Pressure Type | Graduated (tightest at ankle) | Uniform or loose fit |
| Medical Use | Yes – treats & prevents conditions | No – purely functional/fashion |
| Material | Nylon, spandex, microfiber blend | Cotton, wool, acrylic |
| Durability | Retains elasticity for months | Sags or stretches quickly |
| Price Range | $15–$50+ per pair | $5–$15 per pair |
| Washing Care | Hand wash or gentle cycle recommended | Machine washable, low maintenance |
Common Misconceptions Debunked
Misconception 1: “If it feels tight, it’s compressing.”
Not true. Uniform tightness can restrict blood flow rather than assist it. True compression is graduated and medically tested.
Misconception 2: “Athletic socks are the same as compression.”
Some performance socks claim “compression-like” benefits, but unless they specify mmHg and gradient design, they’re unlikely to deliver therapeutic effects.
Misconception 3: “Only older people need compression.”
Young athletes, pregnant women, frequent travelers, and desk workers all benefit. Circulation issues aren’t age-limited.
How to Choose the Right Compression Socks
Selecting the right pair involves more than picking a color or size. Follow this checklist to ensure effectiveness:
- Determine your need: Travel, recovery, medical condition, or athletic performance?
- Check the compression level: 15–20 mmHg for prevention, higher levels require medical advice.
- Measure your leg: Use ankle and calf circumference to match sizing charts—ill-fitting socks lose effectiveness.
- Look for certification: FDA-cleared or CE-marked products meet quality standards.
- Try reputable brands: Sigvaris, Jobst, CEP, and Physix Gear Sport are known for consistency.
- Replace every 3–6 months: Elasticity degrades over time, reducing therapeutic benefit.
Frequently Asked Questions
Can I wear compression socks every day?
Yes, if you're using mild (15–20 mmHg) compression and have no contraindications like severe peripheral artery disease. Many people wear them daily for comfort and prevention. However, if using firm compression (30–40 mmHg), follow your doctor’s guidance.
Do compression socks help with varicose veins?
They won’t cure varicose veins, but they can significantly reduce symptoms like aching, swelling, and fatigue. They also slow progression by improving blood flow. For best results, combine with exercise, leg elevation, and weight management.
Are compression socks safe during pregnancy?
Yes—and highly recommended. Pregnancy increases the risk of swelling and blood clots due to hormonal changes and pressure on pelvic veins. Most obstetricians suggest 15–20 mmHg compression stockings starting in the second trimester.
Final Thoughts: Function Over Fashion
Calling compression socks “fancy knee-highs” is like calling a stethoscope a “fancy necklace.” The comparison misses the point entirely. While both garments cover the lower leg, only compression socks are engineered to improve blood flow, reduce swelling, and support vascular health. They’re backed by decades of medical research, prescribed by doctors, and used by millions for legitimate physiological benefits.
That said, modern compression socks have evolved to be stylish, breathable, and comfortable—bridging the gap between healthcare and everyday wear. But their value isn’t in appearance; it’s in what they do beneath the surface.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?