Sleep is foundational to health—impacting everything from cognitive function to immune resilience. As more people turn to wearable technology to monitor their rest, questions arise: Can a wristband or ring truly detect whether you're sleeping well—or poorly? And more critically, are these consumer-grade sleep trackers reliable enough to identify clinical sleep issues like insomnia, sleep apnea, or circadian disruption?
The short answer: while modern sleep trackers offer valuable insights into sleep trends, they are not yet accurate or regulated enough to replace clinical diagnostics. However, their role in identifying potential red flags and guiding conversations with healthcare providers is growing. This article examines the scientific evidence behind tracker accuracy, compares leading devices, and outlines how consumers can use this data wisely.
How Sleep Trackers Work: The Science Behind the Sensors
Sleep tracking devices—such as Fitbit, Apple Watch, Oura Ring, and Garmin wearables—rely on a combination of sensors and algorithms to estimate sleep stages and duration. Unlike polysomnography (PSG), the gold standard in sleep labs, wearables use indirect metrics:
- Accelerometry: Measures movement to infer sleep versus wake states.
- Heart rate variability (HRV): Used to estimate light, deep, and REM sleep phases based on autonomic nervous system fluctuations.
- Body temperature: Some advanced trackers (e.g., Oura Ring) include thermal sensors to detect subtle shifts associated with sleep cycles.
- Blood oxygen saturation (SpO2): Monitors for potential breathing disruptions, though often only intermittently.
These inputs feed proprietary algorithms that classify sleep stages. But because they don’t measure brainwave activity (via EEG), eye movements (EOG), or muscle tone (EMG), their ability to distinguish between true REM and light sleep remains limited.
“Consumer sleep trackers are excellent for trend analysis but should not be used to rule in or out sleep disorders.” — Dr. Cathy Goldstein, Neurologist and Sleep Specialist, University of Michigan
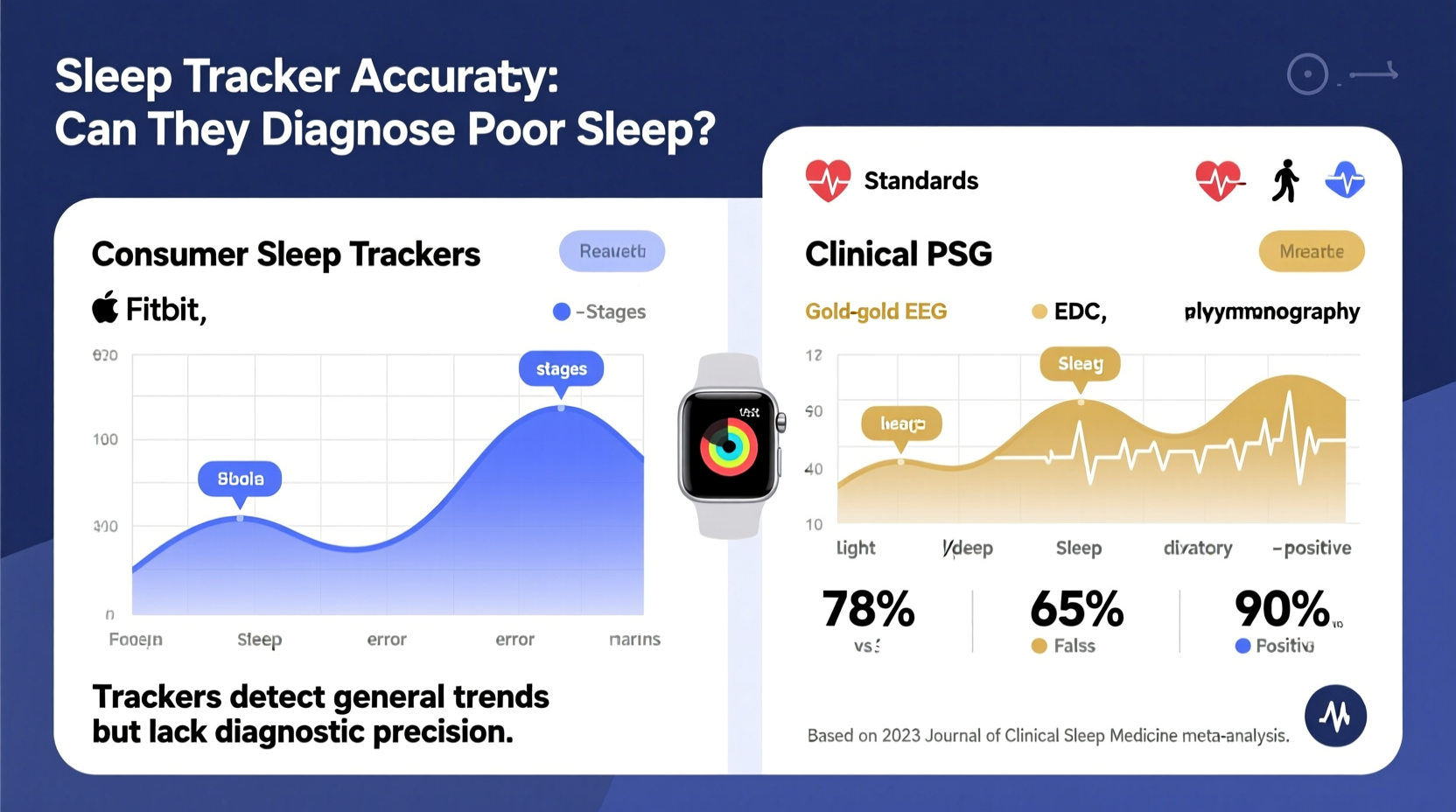
Accuracy Compared to Polysomnography: What Studies Reveal
To assess reliability, researchers have repeatedly compared wearable devices against PSG in controlled settings. A 2021 meta-analysis published in *Sleep Medicine Reviews* evaluated 33 studies involving over 2,000 participants. Key findings included:
- Most trackers accurately detect total sleep time within 10–15 minutes of PSG readings.
- They perform reasonably well at distinguishing sleep from wakefulness, especially in individuals with regular sleep patterns.
- However, accuracy drops significantly when estimating specific sleep stages—particularly REM and deep sleep.
- Devices tend to overestimate total sleep time and underestimate sleep latency (time to fall asleep).
For example, one study found that Fitbit Charge 3 overestimated REM sleep by an average of 72 minutes per night compared to PSG. Another showed that while the Oura Ring closely tracked sleep onset and wake time, it misclassified up to 40% of actual REM periods.
Can Wearables Diagnose Poor Sleep Patterns? Limitations and Risks
While some users report discovering undiagnosed sleep apnea after noticing repeated oxygen desaturation alerts, relying solely on tracker data for diagnosis carries significant risks:
- Lack of medical validation: Most devices are FDA-cleared only for general wellness, not diagnostic use.
- Algorithm opacity: Manufacturers rarely disclose how data is processed, making independent verification difficult.
- Individual variability: Skin tone, arm dominance, device fit, and even hydration levels can affect sensor accuracy.
- Noisy data interpretation: Alerts about “poor sleep” may cause anxiety (orthosomnia), where users become overly fixated on improving scores at the expense of actual rest.
A real-world case illustrates this risk: Sarah, a 38-year-old teacher, began wearing a smartwatch after experiencing fatigue. For weeks, her device reported low deep sleep and frequent awakenings. Despite feeling rested most mornings, she restricted her schedule, avoided social events, and eventually consulted a sleep clinic. A PSG revealed normal sleep architecture—her symptoms were unrelated to sleep quality. The tracker had amplified subjective concerns into unnecessary distress.
“We’re seeing patients who come in convinced they have severe insomnia based on their tracker data—only to find they’re actually sleeping fine.” — Dr. Raj Dasgupta, Sleep Physician, Keck School of Medicine
Comparing Top Sleep Trackers: Features vs. Reliability
Not all trackers are created equal. Below is a comparison of leading devices based on research-backed performance and user-reported utility:
| Device | Key Sensors | Reported Sleep Stage Accuracy (vs. PSG) | Best For | Limitations |
|---|---|---|---|---|
| Fitbit Sense 2 | HRV, SpO2, skin temperature, accelerometer | Moderate (good for TST, fair for REM/deep) | Trend monitoring, wellness integration | Overestimates REM; algorithm changes without notice |
| Oura Ring Gen3 | HRV, body temp, movement, SpO2 | High (best-in-class for sleep staging) | Detailed recovery insights, circadian rhythm tracking | Expensive; less accurate in very active users |
| Apple Watch Series 8 | HRV, accelerometer, optional third-party apps | Low-Moderate (limited native sleep stage detail) | Integration with iOS health ecosystem | Limited built-in analysis; relies on third-party tools |
| Garmin Venu 3 | HRV, pulse ox, accelerometer, respiration | Moderate (strong on consistency tracking) | Athletes, stress and recovery balance | Less precise in detecting sleep onset |
| Whoop 4.0 | HRV, skin temp, strain, recovery | Moderate (focuses on recovery, not staging) | Performance optimization, sleep coaching | No screen; subscription model required |
The table shows that while devices like the Oura Ring lead in sleep stage estimation, none match clinical standards. Their value lies not in pinpoint accuracy, but in longitudinal tracking—spotting deviations from personal baselines that may warrant further investigation.
When Sleep Tracker Data Can Be Useful: A Practical Guide
Despite limitations, sleep trackers can serve as early-warning systems when used thoughtfully. Follow this step-by-step approach to maximize benefit while minimizing misinformation:
- Establish a baseline (Weeks 1–2): Wear the device consistently without altering habits. Record average bedtime, wake time, total sleep, and HRV.
- Identify outliers (Ongoing): Note nights with major deviations—e.g., unusually low HRV, frequent awakenings, or oxygen dips.
- Correlate with symptoms: Ask: Did I feel unrested? Was I irritable or fatigued the next day? Is there snoring or gasping reported by a partner?
- Look for patterns (After 4+ weeks): Are disruptions clustered? Do they follow lifestyle changes (alcohol, stress, travel)?
- Consult a professional: Bring summarized data (screenshots, trend graphs) to a primary care provider or sleep specialist.
This method transforms raw data into actionable insight. For instance, if your tracker consistently shows low SpO2 levels during sleep—and you experience daytime drowsiness—it may prompt a referral for a home sleep apnea test (HSAT), which uses validated medical equipment.
Action Checklist: Using Your Sleep Tracker Wisely
- ✅ Use the same device and wear it consistently (same wrist/finger).
- ✅ Focus on weekly averages, not single-night scores.
- ✅ Pair tracker data with a simple journal (mood, caffeine, bedtime routine).
- ✅ Avoid obsessing over \"perfect\" sleep metrics.
- ✅ Share long-term trends—not screenshots—with your doctor.
- ✅ Turn off notifications if they increase bedtime anxiety.
Frequently Asked Questions
Can a sleep tracker detect sleep apnea?
Some devices flag potential signs—like repeated blood oxygen drops or irregular breathing patterns—but cannot confirm sleep apnea. These alerts may prompt further testing, but only a formal sleep study (PSG or HSAT) can diagnose the condition.
Should I trust my watch’s sleep score?
Sleep scores are algorithmic summaries designed for engagement, not medical insight. They can highlight inconsistencies, but shouldn't dictate behavior. A low score doesn't always mean poor-quality sleep, especially if you feel refreshed.
Are prescription sleep trackers more accurate?
Yes. Medically prescribed devices such as the WatchPAT or Nox T3 use more rigorous sensors and are validated for diagnostic use. However, they are typically used for short-term assessments, not daily monitoring.
Conclusion: From Data to Diagnosis—A Balanced Approach
Sleep trackers are powerful tools for self-awareness, offering a window into rest patterns that were once invisible. They can help identify lifestyle-related disruptions, support behavioral changes, and even accelerate diagnosis when red flags emerge. But they are not substitutes for clinical evaluation.
Their true value lies in partnership—with users who interpret data contextually, and with healthcare providers who integrate it into broader assessments. As sensor technology improves and AI models evolve, we may see greater diagnostic confidence in future wearables. For now, treat your tracker as a conversation starter, not a verdict.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?