Stool color is a reliable indicator of digestive health. While brown is typical, variations occur—and black stool often raises concern. Known medically as melena when caused by bleeding, black poop can stem from harmless sources like food or medication, or signal serious gastrointestinal issues. Understanding the difference between benign and dangerous causes helps determine when to act.
Not all black stools are alarming. Some result from eating blueberries or taking iron supplements. Others, however, point to upper gastrointestinal bleeding—a potentially life-threatening condition. Recognizing key symptoms, timing, and associated factors is essential for timely intervention.
Common Causes of Black Stool
Black stool arises from multiple sources, broadly categorized into non-medical and medical causes. Most cases fall into the former, but distinguishing them matters for health safety.
- Dietary factors: Foods like black licorice, blueberries, beets, and dark chocolate can darken stool.
- Medications and supplements: Iron supplements, bismuth subsalicylate (Pepto-Bismol), and certain antacids frequently turn stool black.
- Gastrointestinal bleeding: Bleeding in the stomach or upper small intestine leads to melena—tarry, foul-smelling black stool due to digested blood.
- Ulcers and gastritis: Peptic ulcers or inflammation of the stomach lining may erode blood vessels, causing slow or acute bleeding.
- Tumors or esophageal varices: Less common but serious causes, especially in individuals with liver disease or cancer history.
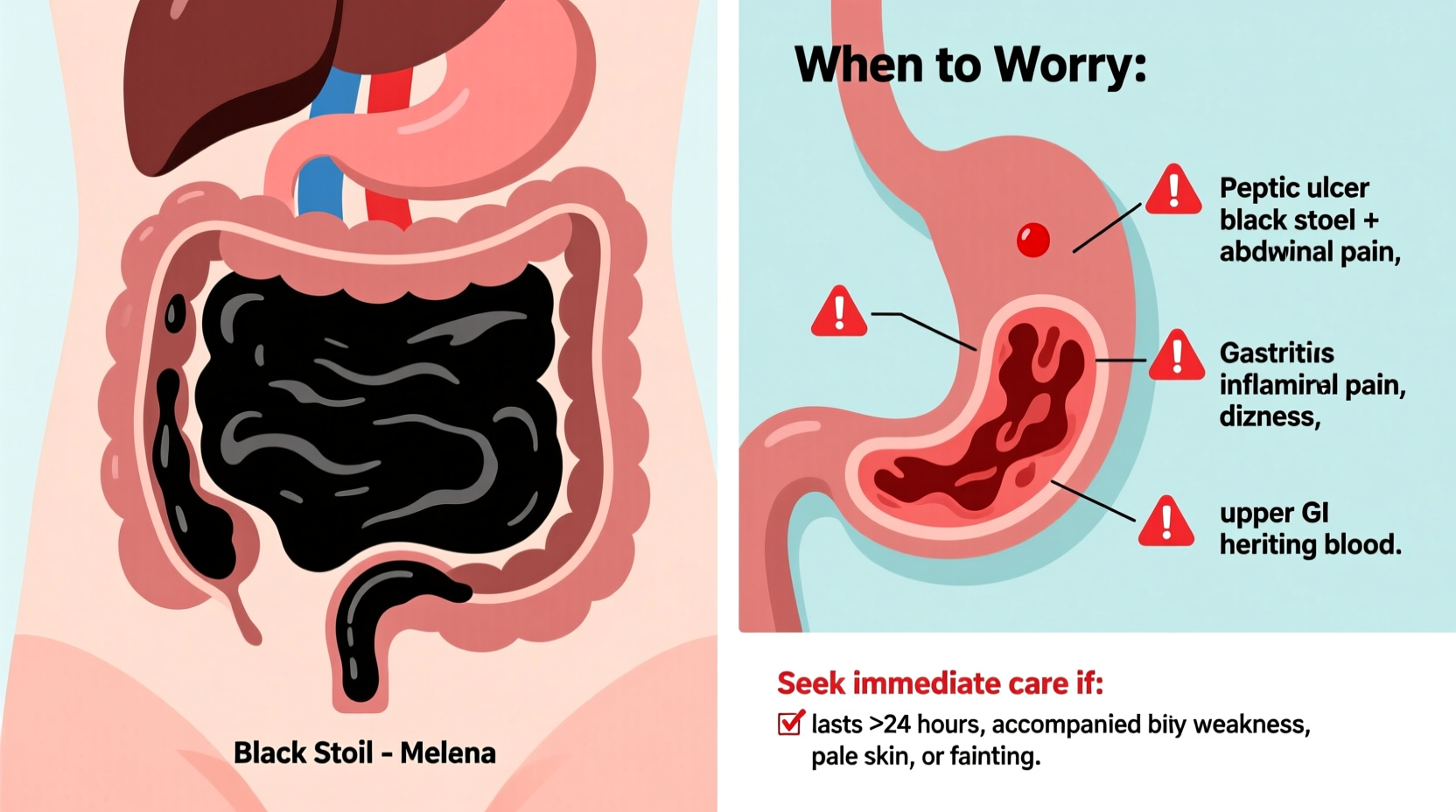
When to Worry: Red Flags to Watch For
Not every instance of black stool requires emergency care, but certain signs suggest urgent evaluation. The presence of additional symptoms increases the likelihood of internal bleeding.
“Tarry, sticky black stool with a strong odor is rarely dietary—it’s usually a sign of upper GI bleeding.” — Dr. Lena Torres, Gastroenterologist
Seek immediate medical attention if black stool is accompanied by any of the following:
- Dizziness or lightheadedness
- Vomiting blood or material resembling coffee grounds
- Abdominal pain or cramping
- Unexplained fatigue or shortness of breath
- Pale skin or rapid heartbeat
- Recent use of NSAIDs (e.g., ibuprofen, aspirin) over several weeks
The consistency and smell matter. Melena typically appears shiny, sticky, and has a distinct foul odor due to hemoglobin breakdown in the gut. In contrast, diet-induced black stool tends to be uniform and less pungent.
Diagnostic Process: What to Expect at the Doctor
If black stool persists beyond a couple of days or occurs with warning signs, a physician will likely initiate a diagnostic workup. This begins with a thorough patient history and physical exam, followed by targeted testing.
- Medical history review: Doctors ask about medications, recent diet, alcohol use, and prior ulcers or liver conditions.
- Fecal occult blood test (FOBT): A simple test to detect hidden blood in stool.
- Complete blood count (CBC): Checks for anemia, which may indicate chronic blood loss.
- Endoscopy: An upper endoscopy allows direct visualization of the esophagus, stomach, and duodenum to locate bleeding sites.
- Imaging: In some cases, CT scans or capsule endoscopy help identify obscure sources of bleeding.
Early diagnosis improves outcomes significantly, especially for conditions like gastric ulcers or malignancies. Delaying evaluation risks complications such as severe anemia or hemorrhagic shock.
Do’s and Don’ts When You Notice Black Stool
| Action | Do | Don’t |
|---|---|---|
| Evaluating cause | Review recent diet, supplements, and medications | Ignore persistent changes lasting more than 3 days |
| Symptom monitoring | Track associated symptoms like fatigue or nausea | Assume it's “just iron” without verification |
| Seeking care | See a doctor promptly if red flags appear | Self-treat with acid reducers without diagnosis |
| Medication use | Inform your doctor about NSAID or anticoagulant use | Stop prescribed meds without consulting a professional |
Real-Life Example: A Case of Misinterpreted Symptoms
Mark, a 52-year-old accountant, noticed his stool had turned black over three consecutive mornings. Assuming it was due to the iron tablets he’d started for mild anemia, he dismissed it. Over the next week, he developed increasing fatigue and occasional stomach discomfort. He attributed this to stress at work.
After two weeks, Mark fainted at home and was rushed to the ER. Blood tests revealed severe anemia (hemoglobin of 7.2 g/dL). An emergency endoscopy found a bleeding gastric ulcer, likely exacerbated by long-term ibuprofen use for back pain. With prompt treatment—including clotting therapy and proton pump inhibitors—Mark recovered. His doctors emphasized that earlier intervention could have prevented hospitalization.
This case illustrates how easily concerning symptoms can be misattributed to benign causes. Self-diagnosis without clinical confirmation carries real risks.
Prevention and Management Tips
While not all causes of black stool are preventable, managing risk factors reduces the likelihood of serious underlying conditions.
- Limits on alcohol and tobacco reduce irritation of the stomach lining.
- Avoid combining NSAIDs with corticosteroids or anticoagulants unless medically supervised.
- Monitor iron supplement intake; excessive doses increase constipation and stool discoloration.
- Maintain regular check-ups if you have chronic conditions like H. pylori infection or liver cirrhosis.
Frequently Asked Questions
Can dehydration cause black stool?
No, dehydration alone does not cause black stool. However, concentrated waste from low fluid intake may appear darker than usual. True black, tarry stool is more likely linked to bleeding or substances like iron.
Is black stool always a sign of cancer?
No. While gastrointestinal cancers can cause melena, they are far less common than ulcers or medication effects. Persistent black stool warrants investigation, but it should not be assumed to be cancerous without diagnostic testing.
How long does Pepto-Bismol stay in your system affecting stool color?
Bismuth subsalicylate can darken stool for up to 3–5 days after stopping use. The effect is harmless and resolves on its own.
Step-by-Step Guide: What to Do If You Notice Black Stool
- Pause potential triggers: Stop iron supplements or Pepto-Bismol for 48 hours if recently started.
- Review your diet: Identify consumption of dark-colored foods or beverages.
- Check for symptoms: Note dizziness, abdominal pain, vomiting, or fatigue.
- Observe stool characteristics: Is it tarry and smelly? Does it leave a smear when flushed?
- Contact your doctor: Report findings, especially if stool remains black or symptoms develop.
- Follow through with testing: Complete recommended exams like blood work or endoscopy if advised.
Conclusion: Take Charge of Your Digestive Health
Black poop isn't automatically dangerous, but it demands thoughtful attention. Whether it's a side effect of a daily vitamin or a signal of internal bleeding, the right response starts with awareness and ends with action. Ignoring persistent changes in bowel habits can lead to delayed diagnoses and avoidable complications.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?