Noticing a change in stool color can be unsettling, especially when it turns black. While occasional discoloration may result from harmless dietary factors, black stool—medically referred to as melena—can also signal internal bleeding or other serious gastrointestinal issues. Understanding the difference between benign causes and warning signs is crucial for timely intervention. This article breaks down the most common reasons behind black stools, highlights red flags, and guides you on when to seek medical help.
What Causes Black Stool?
Black, tarry stools often stem from changes in diet, medication, or underlying health conditions. The key is determining whether the dark color results from something ingested or from blood in the digestive tract.
Dietary Causes
Certain foods are known to darken stool without indicating any health problem:
- Iron-rich foods: Red meat, spinach, lentils, and fortified cereals can contribute to darker stools, especially when consumed in large amounts.
- Blueberries and black licorice: These deeply pigmented foods may temporarily alter stool color.
- Beets (in some cases): Though more commonly associated with red urine or stool, they occasionally cause darkening.
Medications and Supplements
Several over-the-counter and prescription medications are frequent culprits behind black stool:
- Iron supplements: One of the most common non-medical causes. Ferrous sulfate and similar formulations often turn stool dark green or black.
- Bismuth subsalicylate: Found in medications like Pepto-Bismol and Kaopectate, this compound reacts with sulfur in the gut to form bismuth sulfide—a black substance that colors the stool.
- Activated charcoal: Used in detox products or overdose treatments, it passes through the digestive system and turns stool jet black.
“Patients often panic when they see black stool, but in many cases, it's just their multivitamin or a recent dose of Pepto-Bismol.” — Dr. Lena Patel, Gastroenterologist at Cleveland Clinic
When Black Stool Signals a Medical Problem
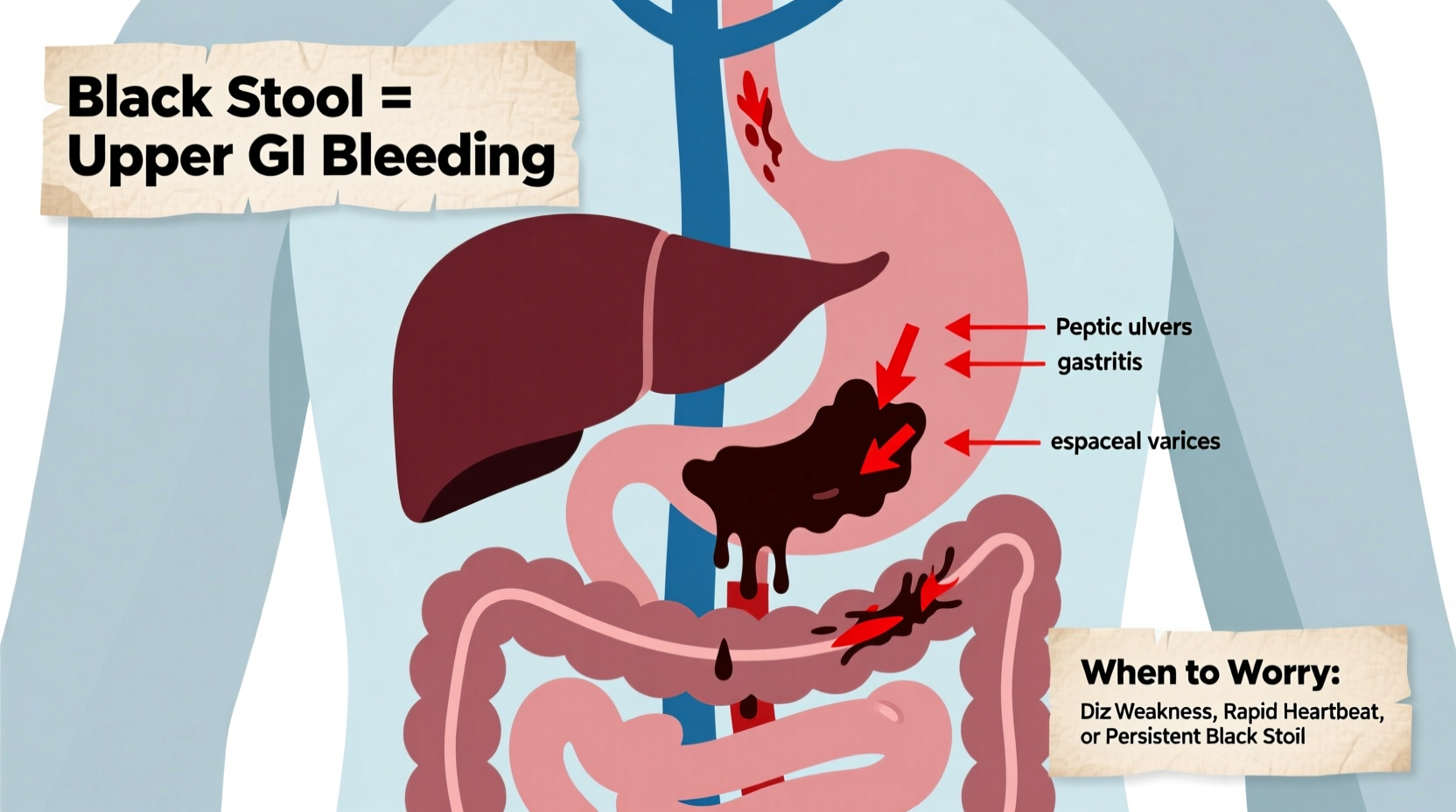
Melena—black, sticky, foul-smelling stool—is a clinical sign of upper gastrointestinal (GI) bleeding. Blood from the stomach or small intestine undergoes digestion, turning it black and giving it a tar-like consistency.
Common Medical Causes
- Peptic ulcers: Sores in the lining of the stomach or duodenum can bleed slowly, leading to melena. Often caused by H. pylori infection or long-term NSAID use.
- Gastritis or esophagitis: Inflammation of the stomach or esophagus lining can erode blood vessels and cause bleeding.
- Mallory-Weiss tears: These are lacerations in the esophagus, typically from violent vomiting, which may lead to minor bleeding.
- Esophageal varices: Swollen veins in the esophagus, usually due to liver cirrhosis, that can rupture and bleed heavily.
- Tumors or malignancies: Cancers in the stomach or upper GI tract may ulcerate and bleed over time.
The presence of melena suggests bleeding proximal to the ligament of Treitz—the anatomical boundary between the upper and lower GI tract. This differentiates it from bright red blood in stool, which typically indicates lower GI bleeding (e.g., hemorrhoids, diverticulosis).
Red Flags: When to Worry About Black Stool
While not all black stools are dangerous, certain accompanying symptoms demand urgent evaluation.
| Symptom | Interpretation | Action Required |
|---|---|---|
| Black, tarry, and foul-smelling stool | Classic melena—likely upper GI bleed | Seek emergency care |
| Dizziness, weakness, or fainting | Possible anemia from blood loss | Immediate medical assessment |
| Abdominal pain or cramping | May indicate ulcer or perforation | Consult doctor promptly |
| Vomiting blood (red or coffee-ground appearance) | Active upper GI bleeding | Call emergency services |
| Persistent black stool beyond 48 hours after stopping supplements | Unexplained source of bleeding | Schedule gastroenterology visit |
Mini Case Study: Recognizing a Silent Bleed
John, a 54-year-old office worker, noticed his stool had turned black over three days. He initially dismissed it as a side effect of his new iron supplement. However, he began feeling unusually fatigued and lightheaded while climbing stairs. His wife urged him to see a doctor. Blood tests revealed severe iron-deficiency anemia. An endoscopy uncovered a bleeding gastric ulcer caused by years of occasional ibuprofen use. With treatment, including antibiotics for H. pylori and acid-suppressing medication, John recovered fully. His case underscores how subtle symptoms can mask serious internal bleeding.
Diagnosis and What to Expect at the Doctor
If your doctor suspects an upper GI bleed, they will likely perform one or more diagnostic procedures:
- Fecal occult blood test: Checks for hidden blood in stool.
- Complete blood count (CBC): Assesses for anemia or low hemoglobin.
- Endoscopy (EGD): A camera-equipped tube examines the esophagus, stomach, and duodenum. It’s the gold standard for identifying and treating upper GI bleeds.
- Imaging studies: CT scans or capsule endoscopy may be used if the source isn’t clear.
Prevention and Management Checklist
To reduce the risk of developing conditions that cause black stool, follow this actionable checklist:
- ✔ Avoid prolonged use of NSAIDs like ibuprofen or naproxen unless prescribed with a protective agent (e.g., proton pump inhibitor).
- ✔ Limit alcohol consumption to protect liver and stomach lining.
- ✔ Treat heartburn or GERD early to prevent esophagitis.
- ✔ Get tested for H. pylori if you have recurrent stomach pain or ulcers.
- ✔ Monitor iron intake—only take supplements if medically indicated.
- ✔ Report persistent changes in bowel habits to your healthcare provider.
Frequently Asked Questions
Can dehydration cause black stool?
No, dehydration does not directly cause black stool. However, concentrated waste due to low fluid intake might appear darker than usual. True melena is unrelated to hydration status and more likely tied to blood or substances like iron.
Is black stool always a sign of cancer?
No, black stool is not always cancer-related. While tumors can cause GI bleeding, far more common causes include ulcers, gastritis, or medication effects. However, unexplained melena should always be evaluated to rule out malignancy.
How long does Pepto-Bismol stay in your system and affect stool color?
Bismuth subsalicylate can darken stool for 24 to 72 hours after the last dose. The effect is temporary and resolves once the medication clears the digestive tract.
Conclusion: Know Your Body, Act Early
Black stool isn't always a crisis, but it shouldn't be ignored—especially when accompanied by fatigue, pain, or dizziness. Distinguishing between harmless triggers like supplements and life-threatening GI bleeds can be difficult without medical insight. Pay attention to patterns, track your symptoms, and don’t hesitate to seek professional evaluation when in doubt. Early detection of gastrointestinal issues significantly improves outcomes. Your digestive health matters; advocate for it with awareness and timely action.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?