Noticing black stool can be alarming. While it’s often due to something you’ve eaten or a medication you’re taking, it can also signal a more serious condition—especially if the darkness is caused by digested blood. Understanding the difference between benign causes and warning signs is essential for knowing when to act.
Black, tarry stools—medically known as melena—are typically sticky and have a strong, unpleasant odor. This appearance usually results from bleeding in the upper gastrointestinal (GI) tract, where blood is broken down by digestive enzymes. However, not all black stools indicate internal bleeding. The key lies in context: what you’ve eaten, what medications you’re on, and whether you're experiencing other symptoms.
Dietary and Medicinal Causes of Black Stool
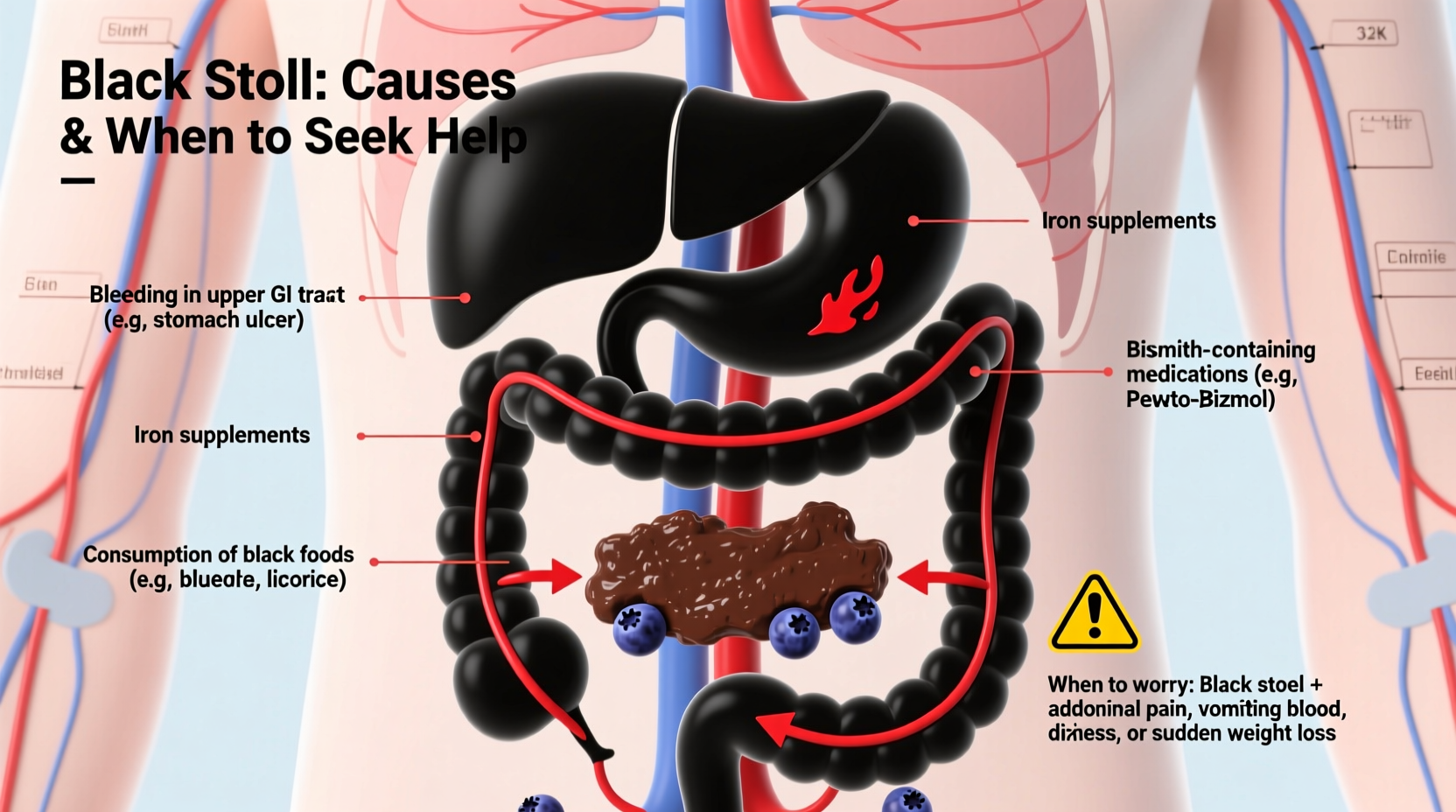
Many cases of black stool are entirely harmless and linked to food or supplements. Iron-rich foods, certain medications, and even some natural substances can darken your bowel movements without posing any health risk.
- Iron supplements: One of the most common causes of black stool. Iron reacts with sulfur compounds in the gut, forming black iron sulfide.
- Bismuth-containing medications: Products like Pepto-Bismol or Kaopectate contain bismuth subsalicylate, which can turn stool gray-black. This is temporary and harmless.
- Dark-colored foods: Consuming large amounts of blueberries, black licorice, or dark beets may temporarily darken stool.
- Activated charcoal: Often used in detox products or after overdoses, this substance turns stool jet black.
When Black Stool Signals a Medical Problem
Melena—black, tarry, foul-smelling stool—is a clinical sign of upper GI bleeding. Blood from the esophagus, stomach, or duodenum is partially digested as it moves through the intestines, turning stool black. Unlike dietary causes, this type of black stool persists and is often accompanied by other symptoms.
Potential sources of bleeding include:
- Gastric or duodenal ulcers
- Esophageal varices (swollen veins in the esophagus)
- Gastritis or erosive esophagitis
- Mallory-Weiss tears (tears in the esophagus from vomiting)
- Tumors or malignancies in the upper GI tract
“Melena is a red flag symptom. If a patient presents with black, tarry stools and signs of anemia or dizziness, we initiate urgent evaluation for upper GI bleeding.” — Dr. Lena Torres, Gastroenterologist
Symptoms That Warrant Immediate Medical Attention
While isolated black stool without other symptoms may not be concerning, certain accompanying signs suggest a serious underlying issue. Seek immediate medical care if you experience:
- Dizziness or lightheadedness
- Weakness or fatigue
- Rapid heart rate
- Vomiting blood (which may look like coffee grounds)
- Abdominal pain or cramping
- Unintentional weight loss
- Fever or chills
If you're over 50, have a history of GI issues, or take blood thinners (like warfarin or aspirin), black stool should be evaluated promptly—even without other symptoms.
Diagnostic Process: What to Expect at the Doctor
If your doctor suspects upper GI bleeding, they will likely perform a series of tests to confirm the diagnosis and locate the source of bleeding.
- Medical history review: You’ll be asked about medications, diet, alcohol use, and recent symptoms.
- Physical exam: Checking for pallor, abdominal tenderness, and signs of anemia.
- Fecal occult blood test: Detects hidden blood in stool, though it won’t distinguish between upper and lower GI sources.
- Endoscopy (EGD): A camera-equipped tube is inserted through the mouth to examine the esophagus, stomach, and duodenum. This is the gold standard for diagnosing upper GI bleeding.
- Blood tests: To check hemoglobin levels and assess for anemia or infection.
In some cases, imaging studies like a CT scan or capsule endoscopy may be used if the source isn’t found during initial testing.
Do’s and Don’ts When You Notice Black Stool
| Do’s | Don’ts |
|---|---|
| Track your diet and medications for possible causes | Ignore persistent black stool lasting more than 2–3 days |
| Stay hydrated, especially if you feel weak | Take NSAIDs (like ibuprofen) which can worsen stomach irritation |
| Contact your doctor if you have additional symptoms | Assume it’s “just iron” without verifying the cause |
| Follow up on recommended tests | Delay evaluation if you’re over 50 or have risk factors |
Real-Life Example: A Case of Misdiagnosed Melena
James, a 58-year-old man, noticed his stool had turned black over several days. He assumed it was due to his new multivitamin with iron. When he began feeling unusually fatigued and lightheaded, he visited his primary care physician. Blood tests revealed severe anemia. An emergency endoscopy uncovered a bleeding gastric ulcer. After treatment with acid-suppressing medication and a blood transfusion, James recovered fully.
This case highlights how easily a serious condition can be mistaken for a benign cause. Had James waited longer, the outcome could have been life-threatening.
Prevention and Long-Term Management
For those prone to GI issues, prevention is key. Chronic use of NSAIDs, heavy alcohol consumption, and untreated H. pylori infections increase the risk of ulcers and bleeding.
Lifestyle changes that support GI health include:
- Limiting alcohol and quitting smoking
- Avoiding excessive NSAID use
- Eating a balanced diet rich in fiber
- Managing stress, which can exacerbate acid production
Frequently Asked Questions
Is black stool always a sign of bleeding?
No. Black stool can result from iron supplements, bismuth medications (like Pepto-Bismol), or dark foods. However, if the stool is tarry, foul-smelling, and persistent, it may indicate upper GI bleeding and should be evaluated.
How long does black stool last after taking iron?
Typically, stool returns to normal within 2–3 days after stopping iron supplements. If it remains black beyond that, especially with other symptoms, consult a doctor.
Can dehydration cause black stool?
Dehydration doesn’t directly cause black stool, but it can concentrate stool and make existing discoloration more noticeable. It may also worsen symptoms if there’s underlying bleeding.
Final Thoughts: When to Act
Black stool isn’t always dangerous, but it shouldn’t be ignored—especially when it appears without a clear dietary or medicinal explanation. Your digestive system communicates through changes in bowel habits, and black stool is one of its loudest signals.
If you’re ever in doubt, err on the side of caution. Early detection of GI bleeding or ulcers can prevent complications like severe anemia or perforation. Keep track of your symptoms, know your medications, and don’t hesitate to seek medical advice.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?