Vaginal bleeding outside of your regular menstrual cycle can be unsettling. While occasional spotting may be harmless, unexpected bleeding can also signal an underlying health issue that requires medical attention. Understanding the possible causes—and knowing when to seek help—is essential for maintaining reproductive health. This article explores the most common reasons for non-menstrual bleeding, highlights warning signs, and provides practical guidance for evaluating your symptoms.
Common Causes of Bleeding Outside Your Period
Bleeding between periods, known as intermenstrual or breakthrough bleeding, can stem from a range of factors—some benign, others more serious. Hormonal fluctuations are among the most frequent culprits. The body’s delicate balance of estrogen and progesterone can be disrupted by stress, weight changes, or certain medications, leading to irregular spotting.
Other common causes include:
- Ovulation spotting: Some women experience light bleeding mid-cycle due to a temporary drop in estrogen during ovulation.
- Hormonal contraceptives: Birth control pills, IUDs (especially copper and hormonal types), implants, or patches can cause irregular bleeding, particularly during the first few months of use.
- Pregnancy-related changes: Implantation bleeding occurs when a fertilized egg attaches to the uterine lining, usually around the time of a missed period. It’s typically lighter and shorter than a normal period.
- Infections: Sexually transmitted infections (STIs) like chlamydia or gonorrhea can inflame the cervix (cervicitis), leading to post-coital or intermenstrual bleeding.
- Uterine or cervical polyps: These noncancerous growths can bleed easily, especially after intercourse.
When to Worry: Red Flags That Require Medical Attention
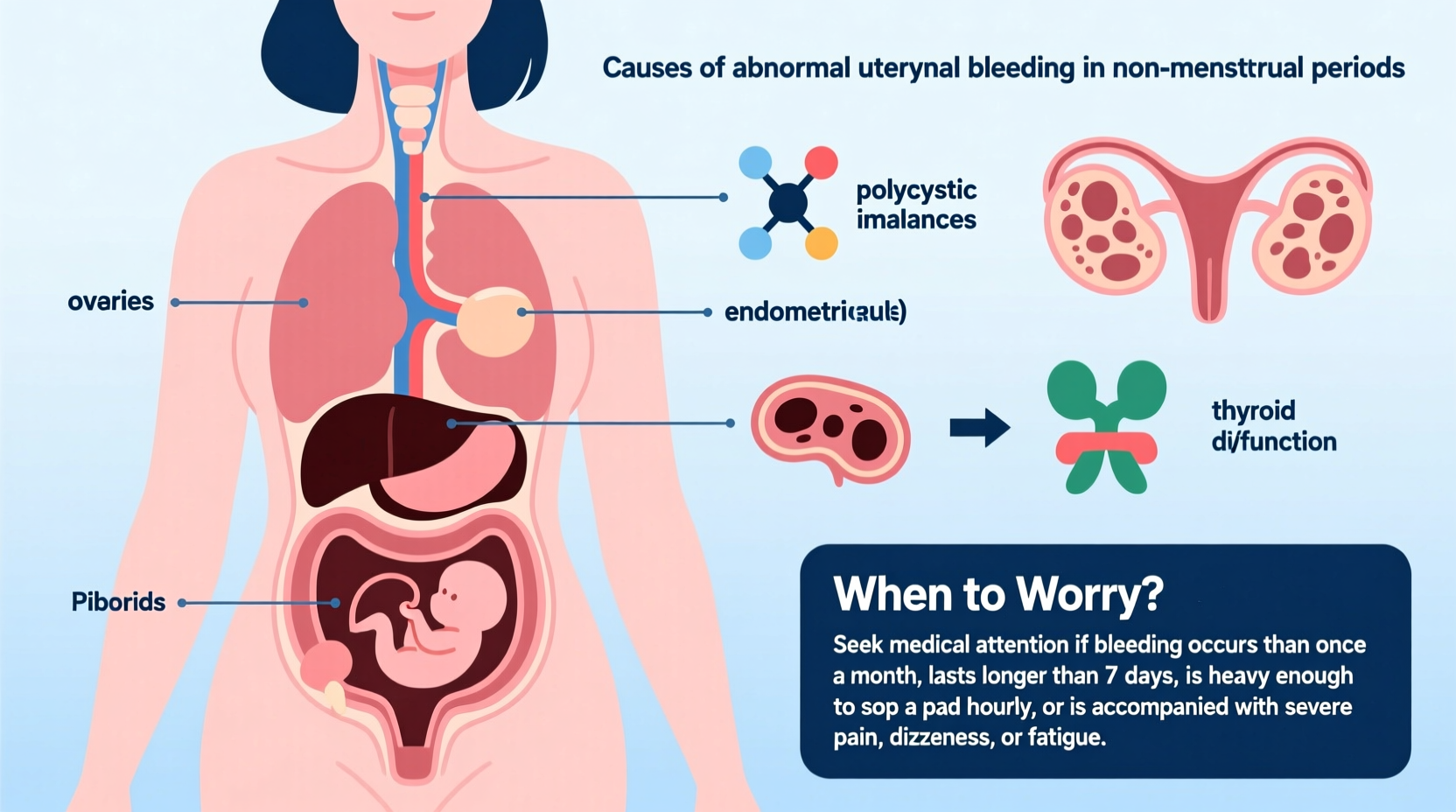
Not all irregular bleeding demands urgent care, but certain patterns should prompt immediate evaluation. Heavy bleeding that soaks through pads or tampons every hour, bleeding lasting longer than seven days, or recurrent spotting over several cycles are not normal and warrant investigation.
Seek prompt medical advice if you experience:
- Bleeding after menopause
- Severe pelvic pain accompanying bleeding
- Foul-smelling vaginal discharge
- Fever with abnormal bleeding
- Bleeding after sexual intercourse (post-coital bleeding)
- Symptoms of anemia such as fatigue, dizziness, or shortness of breath
“Any postmenopausal bleeding is considered abnormal and must be evaluated immediately. It can be an early sign of endometrial cancer.” — Dr. Lena Patel, Gynecologic Oncologist
Medical Conditions Linked to Irregular Bleeding
Several gynecological conditions can lead to bleeding outside your period. Identifying these helps clarify when intervention is necessary.
| Condition | Description | Associated Symptoms |
|---|---|---|
| Endometriosis | Tissue similar to the uterine lining grows outside the uterus | Painful periods, painful sex, infertility |
| Polycystic Ovary Syndrome (PCOS) | Hormonal imbalance causing irregular ovulation | Infrequent periods, acne, weight gain, excess hair growth |
| Uterine Fibroids | Noncancerous tumors in the uterine muscle wall | Heavy periods, pelvic pressure, frequent urination |
| Cervical or Endometrial Cancer | Abnormal cell growth in the cervix or uterine lining | Postmenopausal bleeding, pain during intercourse, unexplained weight loss |
| Thyroid Disorders | Overactive or underactive thyroid affecting hormone regulation | Fatigue, weight changes, mood swings |
Diagnosis often involves a pelvic exam, ultrasound, Pap smear, STI testing, or endometrial biopsy. Early detection significantly improves outcomes, especially in cases involving precancerous or cancerous changes.
Step-by-Step: What to Do If You’re Experiencing Unexplained Bleeding
If you notice bleeding outside your expected cycle, follow this structured approach to assess and respond appropriately.
- Document the details: Note the date, amount (spotting vs. heavy flow), color, and any triggers (e.g., after sex, exercise).
- Review recent changes: Consider new medications, birth control, stress levels, travel, or lifestyle shifts.
- Take a pregnancy test: Even if you're using contraception, rule out pregnancy—especially if your period is late or irregular.
- Avoid self-diagnosis: Don’t assume it’s “just stress” or a side effect without professional input.
- Schedule a doctor’s visit: See a gynecologist within one to two weeks, or sooner if symptoms are severe.
- Prepare for your appointment: Bring your symptom log, list of medications, and questions.
Mini Case Study: Recognizing a Hidden Condition
Sophia, a 34-year-old teacher, noticed light spotting about a week after her period ended. Initially dismissing it as stress-related, she began experiencing heavier mid-cycle bleeding over three consecutive months. After tracking her symptoms and visiting her OB-GYN, an ultrasound revealed multiple uterine fibroids. With treatment, including medication and eventually minimally invasive surgery, Sophia regained regular cycles and relief from fatigue caused by blood loss. Her case underscores how persistent but seemingly minor bleeding can point to treatable structural issues.
Prevention and Management Tips
While not all causes of irregular bleeding can be prevented, certain lifestyle choices support hormonal balance and reproductive health.
- Practice safe sex to reduce the risk of STIs that can cause cervical inflammation.
- Attend regular gynecological checkups, including Pap smears and HPV screenings.
- Manage stress through mindfulness, exercise, or therapy—chronic stress impacts cortisol and reproductive hormones.
- Limit alcohol and avoid smoking, both of which can influence hormonal regulation.
FAQ
Can stress really cause vaginal bleeding?
Yes. Chronic stress affects the hypothalamus, which regulates hormones controlling the menstrual cycle. This disruption can lead to spotting or missed periods. While occasional stress-related changes are common, persistent irregularities should be evaluated.
I’m on birth control and still bleeding—should I be concerned?
Breakthrough bleeding is common in the first 3–6 months of starting hormonal contraception. However, if it continues beyond that, worsens, or starts suddenly after stable use, consult your provider. It could indicate improper fit (e.g., IUD displacement), missed pills, or other issues.
Is spotting during pregnancy normal?
Light spotting, especially early in pregnancy, can be normal (e.g., implantation bleeding). However, any bleeding during pregnancy should be reported to your healthcare provider to rule out complications like ectopic pregnancy or miscarriage.
Conclusion: Take Charge of Your Health
Experiencing bleeding but not on your period doesn’t always mean something is seriously wrong—but it shouldn’t be ignored. From hormonal shifts to more complex conditions, the causes vary widely in severity. The key is awareness, documentation, and timely medical consultation. By paying attention to your body and seeking answers early, you protect not only your reproductive health but your overall well-being.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?