Noticing blood in your urine—especially if it only happens during urination—can be alarming. This symptom, known medically as hematuria, may range from harmless to serious depending on the underlying cause. While occasional spotting might not always signal danger, persistent or painful bleeding when peeing should never be ignored. Understanding the potential reasons behind this symptom empowers you to take timely action and seek appropriate medical care.
Common Causes of Bleeding During Urination
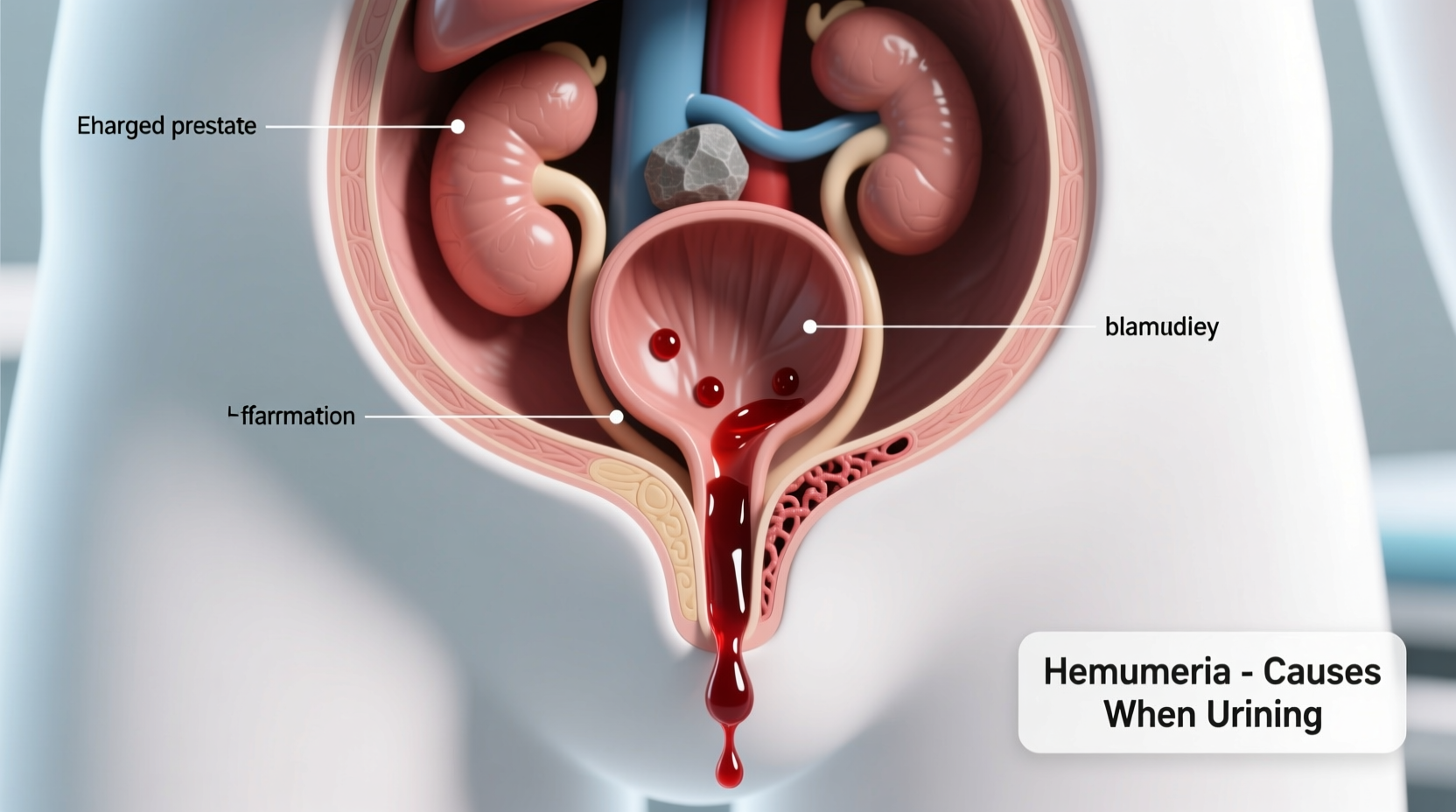
Blood appearing specifically when you urinate often indicates an issue within the lower urinary tract—the bladder, urethra, or ureters. The timing and pattern of bleeding can offer clues about its origin. Below are some of the most frequent causes:
- Urinary Tract Infections (UTIs): One of the leading causes, especially in women. Bacteria entering the urethra can inflame the bladder lining, causing irritation and microscopic or visible blood in urine.
- Bladder or Kidney Stones: As stones move through the urinary tract, they can scratch tissues, resulting in sharp pain and intermittent bleeding that occurs with urination.
- Urethritis: Inflammation of the urethra, often due to infection (including sexually transmitted infections like chlamydia or gonorrhea), can lead to bleeding during or after peeing.
- Enlarged Prostate (in men): Benign prostatic hyperplasia (BPH) can compress the urethra and irritate surrounding tissue, sometimes causing hematuria.
- Bladder or Kidney Cancer: Though less common, persistent painless hematuria is a hallmark sign of urinary tract cancers and warrants immediate evaluation.
When Is the Bleeding Serious?
Not all cases of bloody urine indicate a severe condition, but certain warning signs suggest the need for urgent medical attention:
- Painful urination accompanied by fever or chills
- Inability to urinate despite feeling the urge
- Severe flank or abdominal pain
- Recurrent episodes of bleeding without clear cause
- Weight loss, fatigue, or bone pain alongside hematuria (possible cancer indicators)
“Even asymptomatic hematuria—blood in the urine without pain—should be evaluated. It can be the first and only sign of bladder cancer.” — Dr. Lena Patel, Urologist at Boston Medical Center
Diagnosis: What to Expect at the Doctor
If you're experiencing bleeding only when urinating, your doctor will likely follow a structured diagnostic path to identify the root cause. This typically includes:
- Medical History Review: Questions about frequency, pain, recent infections, medications, and family history of kidney or bladder disease.
- Urinalysis: A lab test to confirm the presence of red blood cells, white blood cells, bacteria, or proteins.
- Urine Culture: To detect bacterial growth and identify specific pathogens causing infection.
- Imaging Tests: Ultrasound, CT scan, or MRI to visualize the kidneys, bladder, and ureters for stones, tumors, or structural abnormalities.
- Cystoscopy: A thin scope inserted into the urethra to examine the bladder lining directly—often used if cancer is suspected.
Diagnostic Timeline Example
| Step | Purpose | Time to Results |
|---|---|---|
| Initial Consultation | Assess symptoms and risk factors | Same day |
| Urinalysis | Detect blood, infection, protein | 1–2 days |
| Urine Culture | Identify bacterial strain | 3–7 days |
| CT Scan / Ultrasound | Check for stones, tumors, blockages | 1–3 days |
| Cystoscopy | Direct visualization of bladder | Immediate findings |
Real-Life Scenario: When Ignoring Symptoms Led to Complications
Sarah, a 34-year-old teacher, noticed her urine turned pink after a long weekend hike. She assumed it was due to dehydration and muscle strain. Over the next two weeks, she experienced mild burning when peeing but no fever or back pain. She dismissed it as a minor UTI and avoided seeing a doctor. Three months later, recurring episodes prompted a visit. A CT scan revealed a 6mm kidney stone stuck in her left ureter, along with signs of early kidney swelling (hydronephrosis). With prompt treatment, including lithotripsy, Sarah recovered—but her delay had increased the risk of permanent kidney damage.
This case highlights how seemingly minor symptoms can mask progressive conditions. Early diagnosis prevents complications and reduces treatment complexity.
Action Plan: What You Should Do Now
If you're noticing blood only when you pee, don’t panic—but do act. Follow this checklist to ensure proper evaluation and care:
- Document symptoms: Note color of urine, frequency, pain, and associated signs (fever, nausea).
- Stay hydrated: Drink water to help flush the urinary tract.
- Avoid irritants: Skip caffeine, alcohol, spicy foods, and harsh soaps near the genital area.
- Schedule a doctor’s appointment: Even if bleeding stops, get tested.
- Provide a clean-catch urine sample: Follow instructions carefully to avoid contamination.
Do’s and Don’ts for Managing Urinary Bleeding
| Do’s | Don’ts |
|---|---|
| Drink plenty of water daily | Ignore a single episode of visible blood |
| Wipe front to back (especially women) | Use scented feminine hygiene products |
| Urinate after sexual intercourse | Delay testing due to embarrassment |
| Take prescribed antibiotics fully | Self-diagnose using online tools alone |
| Follow up on abnormal test results | Assume it's normal because there's no pain |
Frequently Asked Questions
Can dehydration cause blood in urine?
Dehydration itself doesn’t directly cause hematuria, but concentrated urine can irritate the bladder lining and make existing issues—like stones or infections—more noticeable. Severe dehydration combined with intense physical activity (e.g., marathon running) may lead to exercise-induced hematuria, which usually resolves with rest and hydration.
Is it normal to bleed after sex?
Some women may experience light spotting after intercourse due to vaginal or urethral trauma, especially if lubrication is insufficient or there’s an infection. However, recurrent post-sex bleeding should be evaluated to rule out urethritis, cystitis, or cervical conditions.
Can medications cause bloody urine?
Yes. Certain drugs—including blood thinners (warfarin, aspirin), anti-inflammatory medicines (NSAIDs), and cyclophosphamide (a chemotherapy drug)—can increase the risk of urinary bleeding. Always inform your doctor about all medications you’re taking.
Conclusion: Take Charge of Your Urinary Health
Seeing blood only when you pee isn’t something to brush off. Whether it’s a passing infection or a sign of something more serious, your body is sending a message. Timely medical evaluation can distinguish between treatable conditions and those requiring urgent intervention. Most causes of hematuria are manageable when caught early—from simple UTIs to complex stone disease. The key is awareness, prompt action, and honest communication with your healthcare provider.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?