Menstrual cycles are often seen as a reliable barometer of overall health, but irregularities like bleeding twice in one menstrual cycle can be unsettling. While occasional changes in flow or timing are common and usually harmless, frequent or unexpected bleeding may signal an underlying condition that warrants medical attention. Understanding the potential causes—and knowing when to seek help—is essential for maintaining reproductive health and peace of mind.
Understanding Normal vs. Abnormal Uterine Bleeding
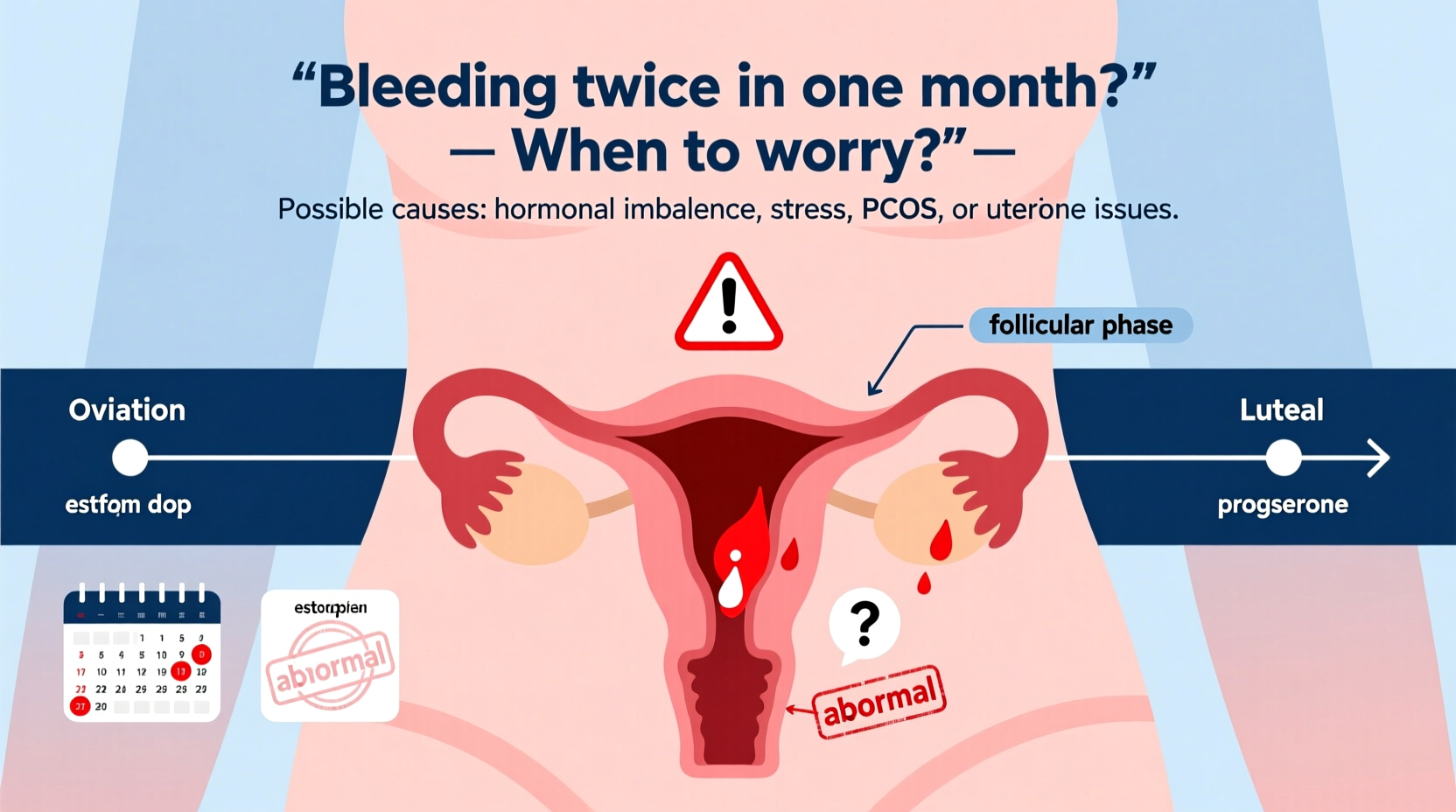
A typical menstrual cycle lasts 21 to 35 days, with bleeding lasting 3 to 7 days. When bleeding occurs outside this window—especially a second episode within the same month—it’s classified as abnormal uterine bleeding (AUB). This doesn’t always indicate a serious problem, but it should never be dismissed without evaluation.
Abnormal bleeding can present as:
- Bleeding between periods (intermenstrual bleeding)
- Spotting after sex
- Heavier-than-usual flow
- Cycles shorter than 21 days
- Bleeding after menopause
The key is consistency. If this is a one-time occurrence during a period of high stress or travel, it may resolve on its own. But recurring or persistent episodes require investigation.
Common Causes of Bleeding Twice in One Month
Several factors—ranging from hormonal shifts to structural issues—can lead to mid-cycle or recurrent bleeding. The most frequent causes include:
Hormonal Imbalances
Fluctuations in estrogen and progesterone levels are among the top reasons for irregular bleeding. These imbalances can stem from:
- Polycystic ovary syndrome (PCOS)
- Thyroid disorders
- Perimenopause (the transition to menopause)
- Sudden weight changes or intense exercise
Ovulation Spotting
Some women experience light spotting around ovulation due to a temporary drop in estrogen. This typically lasts 1–2 days and is not a cause for concern if it’s consistent, minimal, and not accompanied by pain or heavy flow.
Birth Control Use
Hormonal contraceptives—especially when starting, stopping, or switching methods—can cause breakthrough bleeding. This is particularly common with:
- Progestin-only pills
- Implants (e.g., Nexplanon)
- Intrauterine devices (IUDs), especially hormonal ones
This type of bleeding often resolves within 3–6 months as the body adjusts.
Uterine Fibroids and Polyps
Noncancerous growths in the uterus can disrupt normal menstrual patterns. Fibroids (muscle tissue tumors) and polyps (endometrial tissue overgrowths) may cause:
- Heavy or prolonged bleeding
- Painful periods
- Bleeding between cycles
Infections and STIs
Pelvic inflammatory disease (PID), often caused by untreated chlamydia or gonorrhea, can lead to irregular bleeding, pelvic pain, and discharge. Cervical inflammation from infections may also result in spotting after intercourse.
Pregnancy-Related Causes
Early pregnancy complications such as miscarriage or ectopic pregnancy can mimic menstrual bleeding. Any unexplained bleeding in women of reproductive age should prompt a pregnancy test—even if menstruation was recently expected.
When to Worry: Red Flags That Require Medical Attention
While some irregular bleeding is benign, certain signs suggest a need for prompt evaluation. Seek medical care if you experience:
| Symptom | Potential Concern |
|---|---|
| Soaking through a pad or tampon every hour for 2+ hours | Heavy blood loss leading to anemia or hemorrhage |
| Bleeding after menopause | Possible endometrial hyperplasia or cancer |
| Severe pelvic pain or cramping | Fibroids, PID, or ectopic pregnancy |
| Fever with foul-smelling discharge | Infection or retained tissue |
| Dizziness, fatigue, or shortness of breath | Anemia from chronic blood loss |
“Recurrent intermenstrual bleeding isn't something to ignore. It can be a sign of treatable conditions—but early diagnosis improves outcomes.” — Dr. Lena Patel, OB-GYN Specialist
Diagnostic Process and What to Expect at the Doctor
If you're experiencing repeated bleeding, your doctor will likely begin with a detailed history and physical exam. They may ask about:
- Your menstrual pattern over the past 6–12 months
- Use of contraception or hormone therapy
- Recent stress, illness, or lifestyle changes
- Family history of fibroids, endometriosis, or cancer
Next, diagnostic tools may include:
- Pregnancy test: To rule out pregnancy-related causes.
- Blood tests: Checking for anemia, thyroid function, and hormone levels.
- Ultrasound: Transvaginal imaging to assess the uterus, ovaries, and endometrial thickness.
- Endometrial biopsy: Sampling uterine lining tissue, especially in women over 45 or those with risk factors for cancer.
- Hysteroscopy: A minimally invasive procedure to view the inside of the uterus directly.
Based on findings, treatment may involve medication, lifestyle adjustments, or surgical intervention.
Mini Case Study: Sarah’s Experience with Recurrent Bleeding
Sarah, a 38-year-old teacher, began noticing light spotting two weeks after her last period. At first, she dismissed it as stress-related. But when it happened again the following month—this time with heavier flow and fatigue—she scheduled a visit with her gynecologist.
After a transvaginal ultrasound, she was diagnosed with multiple small uterine fibroids. Her hemoglobin level was low, indicating iron-deficiency anemia from chronic blood loss. She started on iron supplements and a low-dose hormonal IUD to reduce bleeding. Within three months, her cycles normalized, and her energy improved significantly.
Sarah’s case highlights how timely evaluation can identify manageable causes and prevent long-term complications like severe anemia.
Action Plan: What You Can Do Now
If you’ve had two bleedings in one month, take these practical steps:
- Take a home pregnancy test, even if unlikely.
- Record the dates, duration, and characteristics of each bleed.
- Note any additional symptoms: pain, fatigue, fever, etc.
- Review recent changes in birth control, medications, or lifestyle.
- Schedule an appointment with your OB-GYN or primary care provider.
Frequently Asked Questions
Can stress really cause me to bleed twice in a month?
Yes. Chronic stress affects the hypothalamus, which regulates hormones that control your cycle. Elevated cortisol can delay ovulation or cause anovulatory cycles, leading to irregular or unexpected bleeding.
Is bleeding between periods a sign of cancer?
Not usually, but it can be. In premenopausal women, cancer is a rare cause of irregular bleeding. However, postmenopausal bleeding is considered a warning sign and must be evaluated promptly to rule out endometrial cancer.
I just got an IUD—why am I bleeding more?
Hormonal IUDs often cause irregular bleeding in the first 3–6 months. Copper IUDs may increase menstrual flow and cramping. Both effects usually improve over time. If bleeding remains heavy or disruptive, consult your provider about alternatives.
Conclusion: Listen to Your Body and Act Early
Bleeding twice in one month isn’t automatically dangerous, but it’s a signal worth investigating. Whether due to hormonal shifts, structural issues, or lifestyle factors, identifying the root cause empowers you to make informed decisions about your health. Ignoring persistent irregularities can lead to complications like anemia, infertility, or delayed diagnosis of serious conditions.
You know your body best. If something feels off, don’t wait for symptoms to worsen. Early consultation leads to faster relief and better outcomes. Take charge of your reproductive health today—your future self will thank you.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?