Finding blood in your stool can be alarming. It’s a symptom that ranges from harmless and temporary to a sign of serious underlying conditions. While occasional minor bleeding may stem from something as simple as hemorrhoids or anal fissures, persistent or heavy bleeding warrants medical attention. Understanding the difference between what’s likely benign and what requires urgent evaluation is essential for timely care.
Blood in the stool—also known as rectal bleeding—can appear in various forms: bright red on toilet paper, mixed in with bowel movements, or even make stools look black and tarry. The color and consistency often provide clues about where the bleeding originates in the digestive tract. This article breaks down the most common causes, highlights red flags, and guides you on when to seek help.
Common Causes of Blood in Stool
Not all rectal bleeding signals a severe problem. Many causes are treatable and relatively common. The location of the bleed within the gastrointestinal (GI) tract determines how the blood appears.
- Hemorrhoids: Swollen veins in the rectum or anus, often caused by straining during bowel movements. They typically cause bright red blood on toilet paper or dripping into the bowl.
- Anal fissures: Small tears in the lining of the anus, usually from passing hard stools. Pain during bowel movements and visible red blood are typical.
- Diverticulosis: Small pouches in the colon wall that can bleed, especially in older adults. Bleeding is often sudden and painless, with maroon or bright red blood.
- Colitis: Inflammation of the colon due to infections, inflammatory bowel disease (IBD), or ischemia. May present with bloody diarrhea, cramping, and urgency.
- Polyps or colorectal cancer: Growths in the colon that can erode and bleed over time. Blood may be hidden (occult) or visible, sometimes mixed with mucus.
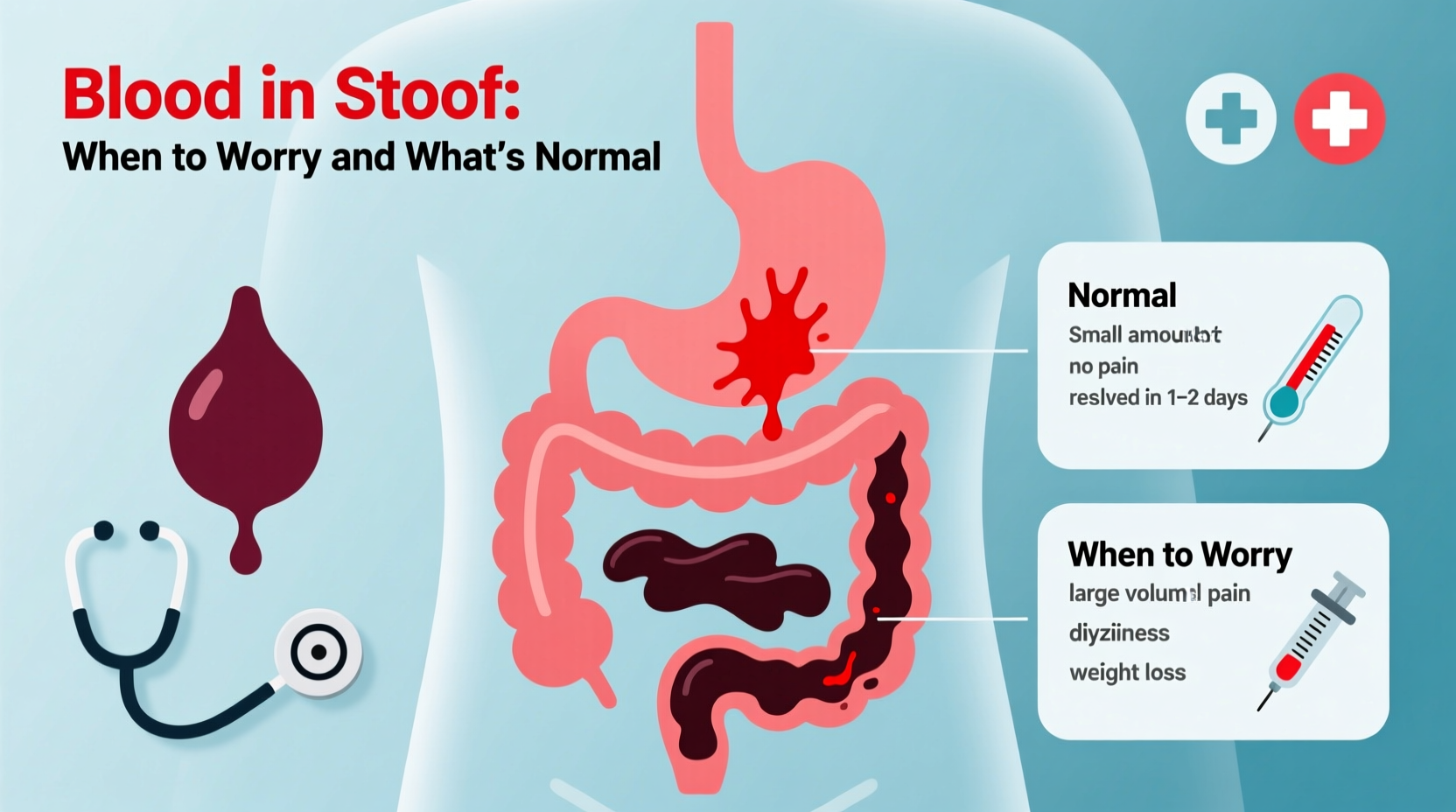
When to Worry: Red Flags That Require Medical Attention
While some instances of blood in stool resolve on their own, certain signs should prompt immediate medical evaluation. These indicate possible serious GI conditions, including cancer, ulcers, or significant inflammation.
“Any new or unexplained rectal bleeding in someone over 40 should be investigated. Colorectal cancer is highly treatable when caught early.” — Dr. Alan Reyes, Gastroenterologist
Symptoms that warrant prompt consultation with a healthcare provider include:
- Persistent bleeding lasting more than a few days
- Black, tarry stools (melena), which suggest upper GI bleeding
- Dizziness, fatigue, or shortness of breath—signs of anemia from chronic blood loss
- Unintentional weight loss
- Abdominal pain or changes in bowel habits (diarrhea, constipation)
- A family history of colorectal cancer
- Age over 45, especially if screening hasn’t begun
Understanding Stool Color and Its Meaning
The appearance of blood in stool helps doctors narrow down its source. Use this guide to interpret what different colors might mean:
| Stool Appearance | Possible Source | Common Causes |
|---|---|---|
| Bright red blood on toilet paper or surface | Lower colon, rectum, or anus | Hemorrhoids, anal fissures |
| Maroon or dark red stool | Colon or small intestine | Diverticulosis, polyps, IBD |
| Black, tarry, foul-smelling stool | Upper GI tract (stomach, duodenum) | Peptic ulcers, gastritis, esophageal varices |
| Streaks of red mixed with mucus | Colon inflammation | Ulcerative colitis, infection |
| No visible blood, but positive fecal test | Microscopic bleeding anywhere in GI tract | Early cancer, polyps, slow bleed |
Step-by-Step: What to Do If You Notice Blood
Discovering blood doesn’t mean panic—but it does call for thoughtful action. Follow this timeline to determine your next steps:
- Assess the situation: Note the color, amount, frequency, and any associated symptoms (pain, fever, change in bowel habits).
- Recall recent diet or medications: Did you eat beets, blueberries, or take iron supplements? These can mimic blood. Stop aspirin or NSAIDs if not medically essential.
- Monitor for 1–3 days: Minor bleeding from straining may resolve with increased fiber and hydration.
- Contact your doctor if: Bleeding persists, worsens, or is accompanied by red flag symptoms.
- Prepare for evaluation: Your doctor may order a fecal occult blood test, sigmoidoscopy, or colonoscopy depending on risk factors.
Real Example: A Wake-Up Call at Age 48
Mark, a 48-year-old teacher, noticed streaks of bright red blood on his stool for two weeks. He initially dismissed it as hemorrhoids, especially since he’d been constipated. But when he began feeling unusually tired and lost 7 pounds without trying, he scheduled a visit. His primary care physician ordered a colonoscopy, which revealed a 3 cm polyp in the ascending colon—some cells were precancerous. After removal, Mark recovered fully. “I almost didn’t go,” he said. “But catching it early made all the difference.”
Prevention and Screening Checklist
Many causes of rectal bleeding are preventable or detectable early through lifestyle choices and routine screening. Use this checklist to stay proactive:
- ✅ Eat a high-fiber diet rich in fruits, vegetables, and whole grains
- ✅ Drink plenty of water daily (at least 6–8 glasses)
- ✅ Avoid prolonged straining during bowel movements
- ✅ Exercise regularly to support healthy digestion
- ✅ Begin colorectal cancer screening at age 45 (or earlier if high-risk)
- ✅ Report any persistent changes in bowel habits to your doctor
- ✅ Don’t ignore blood—even if it seems minor or goes away
Frequently Asked Questions
Is a little blood in stool normal?
Occasional small amounts of bright red blood, especially after a hard bowel movement, can be due to hemorrhoids or fissures and may not be serious. However, even minor bleeding should not be ignored long-term. Recurrent bleeding needs evaluation.
Can food make my stool look bloody?
Yes. Foods like beets, cranberries, blueberries, and red gelatin can tint stool red. Iron supplements and bismuth (found in Pepto-Bismol) can turn stools black. If in doubt, avoid these foods for a few days and recheck. When uncertain, consult a doctor.
Do I need a colonoscopy if I see blood?
Not always immediately, but your doctor will assess your age, symptoms, and risk factors. For individuals over 45 or those with persistent bleeding, a colonoscopy is often recommended to rule out polyps or cancer.
Conclusion: Listen to Your Body
Blood in stool is never something to assume is “normal” without consideration. While many causes are benign and easily treated, the symptom can also be an early warning of conditions like colorectal cancer—especially in adults over 45. The key is awareness, timely response, and not brushing off changes in your body. Whether it’s adjusting your diet, managing hemorrhoids, or scheduling a screening, taking action today can protect your long-term health.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?