Finding blood in your stool can be alarming. Whether it’s streaks on the toilet paper, mixed in with bowel movements, or turning the water pink, rectal bleeding raises immediate concern. While some causes are minor and easily treatable—like hemorrhoids or anal fissures—others may signal serious conditions such as colorectal cancer. Understanding the difference between normal and dangerous signs is essential for timely care.
Blood in the stool, medically known as hematochezia, varies in color depending on where the bleeding originates in the digestive tract. Bright red blood usually indicates a source closer to the anus, while darker, tarry stools suggest bleeding higher up in the colon or stomach. Not all bleeding is life-threatening, but ignoring persistent or severe symptoms can lead to complications.
Common Causes of Blood in Stool
Many gastrointestinal issues can result in rectal bleeding. Most are benign, especially when occasional and mild, but they still warrant attention if they persist.
- Hemorrhoids: Swollen veins in the rectum or anus, often caused by straining during bowel movements, pregnancy, or chronic constipation. They may bleed during defecation, producing bright red blood.
- Anal fissures: Small tears in the lining of the anus, typically from passing hard stools. These cause sharp pain during bowel movements and leave streaks of blood.
- Diverticulosis: Small pouches that form in the colon wall. When inflamed (diverticulitis), they can bleed, sometimes significantly, though often without pain.
- Colitis: Inflammation of the colon due to infections, inflammatory bowel disease (IBD) like ulcerative colitis or Crohn’s disease, or reduced blood flow (ischemic colitis).
- Polyps or colorectal cancer: Growths in the colon that may bleed slowly over time. Cancer-related bleeding is often not visible to the naked eye and detected through screening tests.
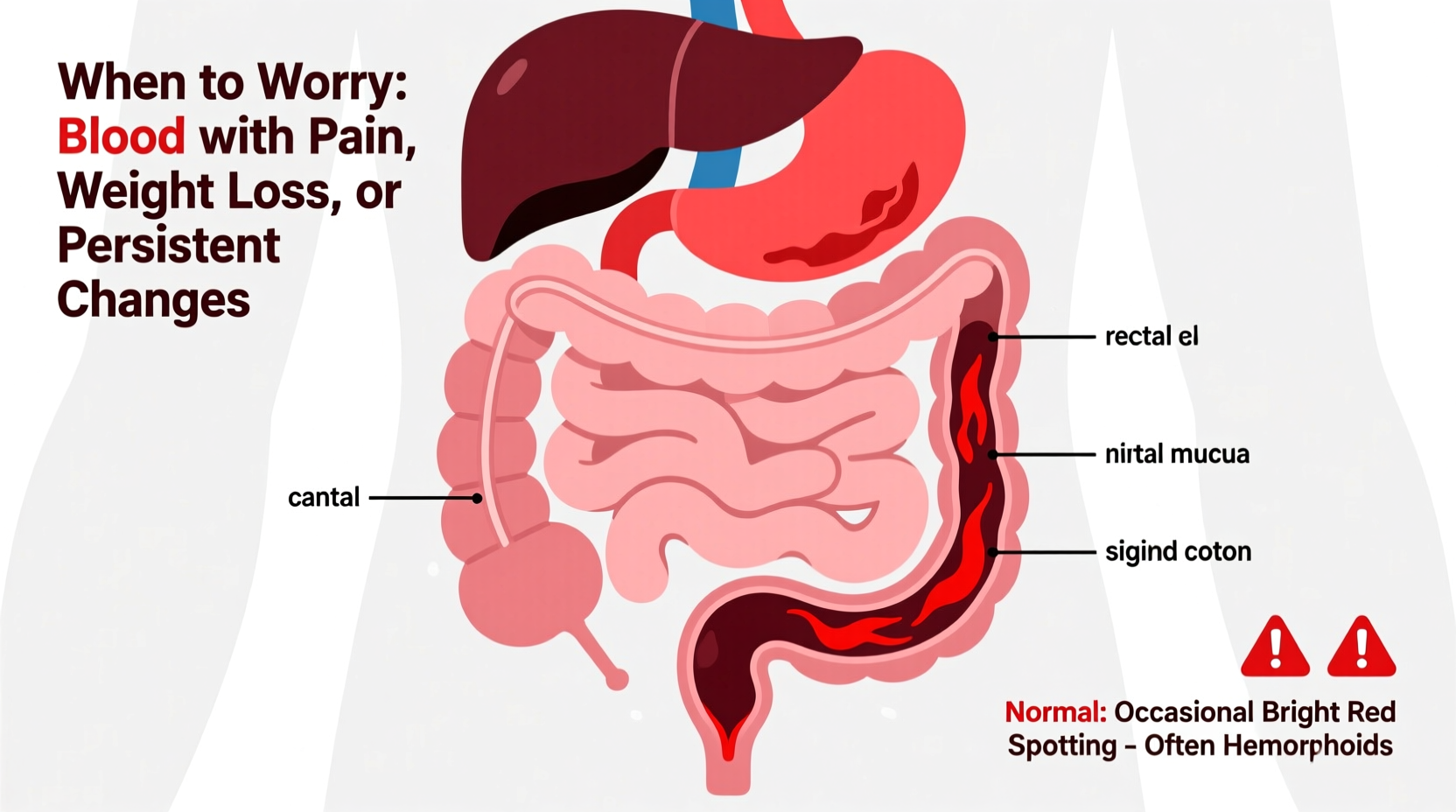
When to Worry: Red Flags That Require Immediate Attention
While occasional, small amounts of bright red blood may not be urgent, certain symptoms should prompt immediate medical evaluation. The presence of these warning signs increases the likelihood of a serious underlying condition.
“Any new onset of rectal bleeding in someone over 40 should be investigated. We can’t assume it’s just hemorrhoids without ruling out malignancy.” — Dr. Lena Torres, Gastroenterologist
Symptoms That Demand Medical Evaluation
- Heavy or continuous bleeding
- Dark maroon or black, tarry stools (melena)
- Dizziness, lightheadedness, or fatigue (signs of anemia)
- Unexplained weight loss
- Persistent abdominal pain or cramping
- Change in bowel habits lasting more than a few days
- Family history of colorectal cancer
- Age over 45, especially if never screened
Even if symptoms seem mild, persistent bleeding—even if minimal—should not be ignored. Colorectal cancer often begins asymptomatically, making early detection through screening crucial.
What’s Normal vs. What’s Not: A Practical Guide
Distinguishing between harmless and concerning bleeding starts with observation. Use this table to assess your situation.
| Feature | Normal / Likely Benign | Concerning / Needs Evaluation |
|---|---|---|
| Blood Color | Bright red, on surface or toilet paper | Dark red, maroon, or black/tarry |
| Amount | Small streaks or drops | Copious blood, filling toilet bowl |
| Pain | Mild discomfort or burning (fissures) | Severe abdominal or rectal pain |
| Frequency | One-time or occasional | Recurrent over days or weeks |
| Other Symptoms | None | Weight loss, fatigue, diarrhea, nausea |
If your experience aligns with the \"Concerning\" column, schedule an appointment with your doctor promptly. Diagnostic tools like colonoscopy, sigmoidoscopy, or fecal immunochemical tests (FIT) can identify the source.
Real-Life Example: Recognizing a Silent Threat
James, a 52-year-old teacher, noticed occasional bright red blood on the toilet paper for about three months. He assumed it was hemorrhoids, especially since he had a family history. He increased his fiber intake and used over-the-counter creams, which reduced the bleeding temporarily. But he also began feeling unusually tired and lost 10 pounds without trying. After encouragement from his wife, he visited his primary care physician.
A FIT test came back positive, leading to a colonoscopy. Doctors discovered a large polyp in the ascending colon, which turned out to be early-stage adenocarcinoma. Because it was caught early, James underwent surgery and avoided chemotherapy. His case highlights how even seemingly minor symptoms, when combined with subtle changes like fatigue or weight loss, can indicate something serious.
Step-by-Step: What to Do If You See Blood
Don’t panic—but do act. Follow this timeline to ensure proper assessment.
- Observe the details: Note the color, amount, frequency, and whether it’s associated with pain or changes in bowel habits.
- Adjust lifestyle factors: Increase water, fiber, and physical activity to ease bowel movements and reduce strain.
- Monitor for 3–5 days: If bleeding stops and no other symptoms arise, it may have been minor. Continue healthy habits.
- Contact your doctor if: Bleeding persists, worsens, or is accompanied by red flag symptoms.
- Get recommended screenings: Adults over 45 should undergo regular colorectal cancer screening, even without symptoms.
Prevention and Long-Term Care Checklist
Reducing your risk of rectal bleeding involves consistent digestive health practices. Use this checklist to stay proactive.
- ✅ Eat a high-fiber diet (fruits, vegetables, whole grains)
- ✅ Drink at least 8 glasses of water daily
- ✅ Avoid prolonged straining during bowel movements
- ✅ Exercise regularly to support gut motility
- ✅ Don’t ignore the urge to go—delaying can harden stool
- ✅ Get a colonoscopy starting at age 45 (or earlier if high-risk)
- ✅ Report any rectal bleeding to your healthcare provider, no matter how minor
Frequently Asked Questions
Is bright red blood always less serious?
Not necessarily. While bright red blood often comes from the lower rectum (like hemorrhoids or fissures), it can also originate from polyps or tumors in the left colon. Persistent bleeding requires evaluation regardless of color.
Can medications cause bloody stool?
Yes. NSAIDs (like ibuprofen or aspirin) can irritate the stomach lining and cause ulcers, leading to dark, tarry stools. Anticoagulants increase bleeding risk anywhere in the GI tract. Always inform your doctor about medications you’re taking.
Do I need a colonoscopy if I’m young?
Generally, screening starts at 45. However, if you have a family history of colorectal cancer, inflammatory bowel disease, or genetic syndromes like Lynch syndrome, your doctor may recommend earlier testing—even in your 20s or 30s.
Take Action Before It’s Too Late
Rectal bleeding is not something to normalize or dismiss. While many causes are treatable and non-life-threatening, the consequences of ignoring potential warning signs can be severe. Advances in screening and treatment mean colorectal cancer is highly preventable when caught early. Don’t wait for symptoms to worsen. Pay attention to your body, maintain open communication with your healthcare provider, and prioritize preventive care.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?