Noticing blood on the toilet paper after a bowel movement can be alarming. While it’s often due to minor, treatable conditions, it can also signal something more serious. The good news is that most cases are not life-threatening and can be managed with simple lifestyle changes or medical treatment. Understanding the possible causes, recognizing warning signs, and knowing when to seek help are crucial steps toward proper care.
Common Causes of Blood When Wiping
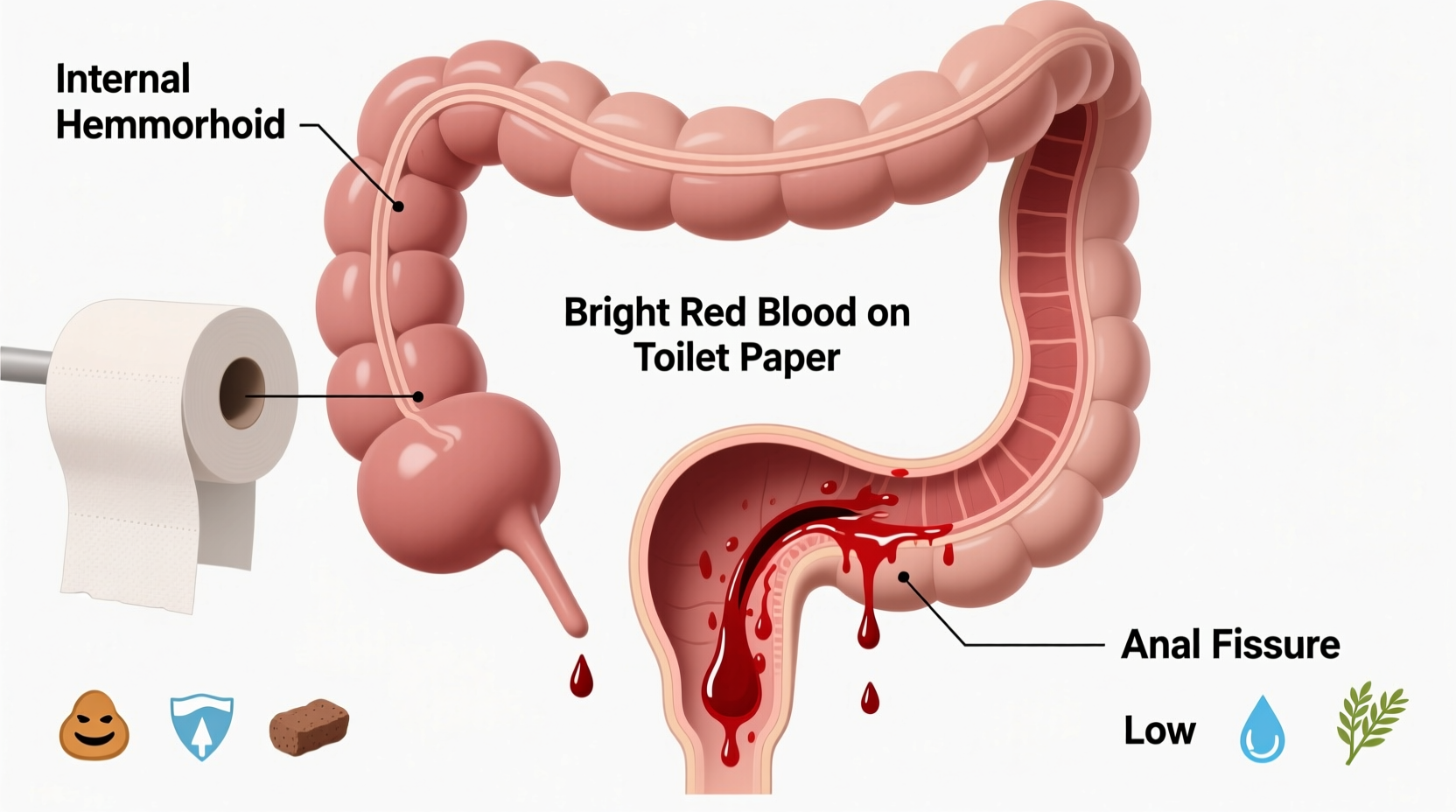
Bright red blood typically indicates bleeding from the lower gastrointestinal tract—most commonly the rectum or anus. Several benign but uncomfortable conditions can lead to this symptom.
- Hemorrhoids: Swollen veins in the rectum or around the anus are the most frequent cause. They can bleed during bowel movements, especially if stools are hard or straining occurs.
- Anal fissures: Small tears in the lining of the anus, often caused by passing large or hard stools. These can cause sharp pain during bowel movements along with bright red blood.
- Anal irritation: Excessive wiping, use of scented wipes, or diarrhea can inflame the delicate skin around the anus, leading to minor bleeding.
- Proctitis: Inflammation of the rectal lining, which may result from infections, inflammatory bowel disease (IBD), or radiation therapy.
- Colorectal polyps: Growths in the colon or rectum that can bleed. While many are harmless, some may become cancerous over time.
When Blood Could Signal Something Serious
While most bleeding is due to non-cancerous causes, certain symptoms should prompt immediate medical evaluation. Blood mixed into the stool, dark or tarry stools, or persistent bleeding may point to conditions like colorectal cancer, inflammatory bowel disease (Crohn’s disease or ulcerative colitis), or diverticulosis.
“Any new onset of rectal bleeding in someone over 45, or those with a family history of colon cancer, warrants a thorough evaluation—even if hemorrhoids are suspected.” — Dr. Lena Patel, Gastroenterologist
Risk factors that increase concern include:
- Age over 45
- Family history of colorectal cancer
- Unexplained weight loss
- Persistent abdominal pain
- Changes in bowel habits lasting more than a few days
- Fatigue or signs of anemia (like dizziness or pale skin)
What You Can Do at Home: Immediate Relief and Prevention
For mild cases linked to hemorrhoids or anal fissures, several self-care strategies can reduce discomfort and promote healing.
Diet and Hydration
Maintaining soft, regular stools is essential. Increase your intake of fiber-rich foods such as fruits, vegetables, legumes, and whole grains. Drink plenty of water—aim for at least 8 glasses daily—to prevent constipation.
Sitz Baths
Soaking the anal area in warm water for 15–20 minutes, two to three times a day, can soothe irritation and improve blood flow to aid healing, especially for fissures or external hemorrhoids.
Over-the-Counter Treatments
Creams, ointments, or suppositories containing hydrocortisone or witch hazel may reduce swelling and discomfort. Use them as directed and avoid prolonged use without medical advice.
| Do | Don’t |
|---|---|
| Eat high-fiber foods (oats, apples, broccoli) | Ignore persistent bleeding beyond a week |
| Stay hydrated | Strain during bowel movements |
| Use gentle, unscented toilet paper | Use harsh wipes or alcohol-based cleaners |
| Exercise regularly to support digestion | Sit for long periods, especially on the toilet |
Step-by-Step Guide: What to Do If You Notice Blood
- Assess the appearance: Note the color (bright red vs. dark), amount, and whether it's on the paper, coating the stool, or mixed in.
- Review recent changes: Consider diet, bowel habits, medications, or activities that might contribute (e.g., heavy lifting).
- Start conservative care: Increase fiber, hydrate, take sitz baths, and avoid straining.
- Monitor symptoms: Track frequency of bleeding, pain levels, and any additional symptoms like fatigue or weight loss.
- Schedule a doctor’s visit: If bleeding persists beyond 7–10 days, worsens, or is accompanied by other symptoms, see a healthcare provider.
Mini Case Study: Recognizing the Need for Medical Evaluation
Mark, a 52-year-old office worker, noticed occasional streaks of blood on the toilet paper for about two weeks. He assumed it was hemorrhoids, as he’d experienced them before. He increased his fiber intake and used an over-the-counter cream, which helped briefly. But then the bleeding returned, and he began feeling unusually tired. His wife urged him to see a doctor. After a colonoscopy, Mark was diagnosed with early-stage colorectal cancer. Because it was caught early, he underwent successful treatment and made a full recovery. His case highlights how easily serious conditions can be mistaken for minor ones—and why timely evaluation matters.
When to See a Doctor
While minor bleeding may resolve on its own, certain red flags require prompt medical attention:
- Bleeding that lasts longer than 7–10 days despite home care
- Heavy bleeding or blood clots
- Dark red or black, tarry stools (indicating upper GI bleeding)
- Pain, lumps, or discharge from the anus
- Anemia symptoms: fatigue, shortness of breath, pale skin
- Family history of colon cancer or IBD
A physician may perform a digital rectal exam, anoscopy, sigmoidoscopy, or colonoscopy to determine the source of bleeding. Early diagnosis significantly improves outcomes, especially in cases involving polyps or cancer.
FAQ
Is it normal to see a little blood after pooping?
Occasional small amounts of bright red blood, especially with hard stools or known hemorrhoids, can be normal. However, it should never be ignored completely. Recurring or unexplained bleeding warrants medical review.
Can stress cause rectal bleeding?
Stress doesn’t directly cause bleeding, but it can exacerbate conditions like IBS or lead to constipation or diarrhea, which may contribute to anal trauma or hemorrhoid flare-ups.
Do I need a colonoscopy just for minor bleeding?
Not always—but doctors often recommend one for patients over 45 or those with risk factors. It’s the most effective way to rule out polyps, inflammation, or cancer.
Prevention Checklist
- Drink at least 8 glasses of water per day
- Eat 25–30 grams of fiber daily (fruits, vegetables, whole grains)
- Avoid sitting on the toilet for long periods
- Respond promptly to bowel urges—don’t delay
- Exercise regularly to support healthy digestion
- Use soft, unscented toilet paper or moistened wipes
- Practice good anal hygiene without over-wiping
Conclusion
Seeing blood when you wipe after pooping is more common than many realize, and often stems from manageable causes like hemorrhoids or fissures. But because it can also be an early sign of serious conditions, it should never be dismissed outright. With the right dietary habits, hygiene practices, and awareness of warning signs, you can protect your digestive health and act quickly when needed. Don’t hesitate to consult a healthcare provider if bleeding persists or concerns arise. Your long-term well-being could depend on it.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?