Fractures in older adults are far more than just broken bones. While a fall and subsequent injury might seem like a temporary setback, the reality is that for seniors, a fracture can trigger a cascade of health complications—some of which can be fatal. As people age, their bodies change in ways that make recovery from trauma significantly harder. Osteoporosis weakens bones, healing slows, and underlying health conditions amplify risks. Understanding why broken bones can be deadly in the elderly is crucial for caregivers, family members, and healthcare providers aiming to prevent and manage these injuries effectively.
The Hidden Dangers of Fractures in Older Adults
Unlike younger individuals, whose bodies typically heal quickly and resiliently, older adults face multiple physiological challenges when recovering from a fracture. The most common sites of injury—hips, spine, and wrists—are especially dangerous due to their impact on mobility and independence. A hip fracture, for example, often requires surgery and prolonged immobility during recovery. This stillness increases the risk of life-threatening complications such as blood clots, pneumonia, and pressure sores.
According to the Centers for Disease Control and Prevention (CDC), approximately 300,000 Americans aged 65 and older are hospitalized for hip fractures each year. Alarmingly, up to 20% of those individuals die within one year of the injury. Even among survivors, only about 25% fully regain their pre-fracture level of function.
Why Healing Is Slower and Riskier with Age
Aging affects nearly every system involved in bone repair. Bone density naturally declines, especially in postmenopausal women, increasing susceptibility to breaks even from minor falls. Additionally, the body’s regenerative capacity diminishes. Blood flow to bones decreases, immune response slows, and stem cell activity wanes—all critical factors in healing.
Chronic conditions commonly seen in seniors further complicate recovery. Diabetes, cardiovascular disease, and respiratory issues impair circulation and oxygen delivery, both essential for tissue repair. Medications such as corticosteroids or anticoagulants may weaken bones or increase bleeding risk during surgery.
“An elderly patient doesn’t just break a bone—they break their resilience. The fracture itself is often less dangerous than what follows.” — Dr. Alan Reyes, Geriatric Trauma Specialist, Massachusetts General Hospital
Life-Threatening Complications After a Fracture
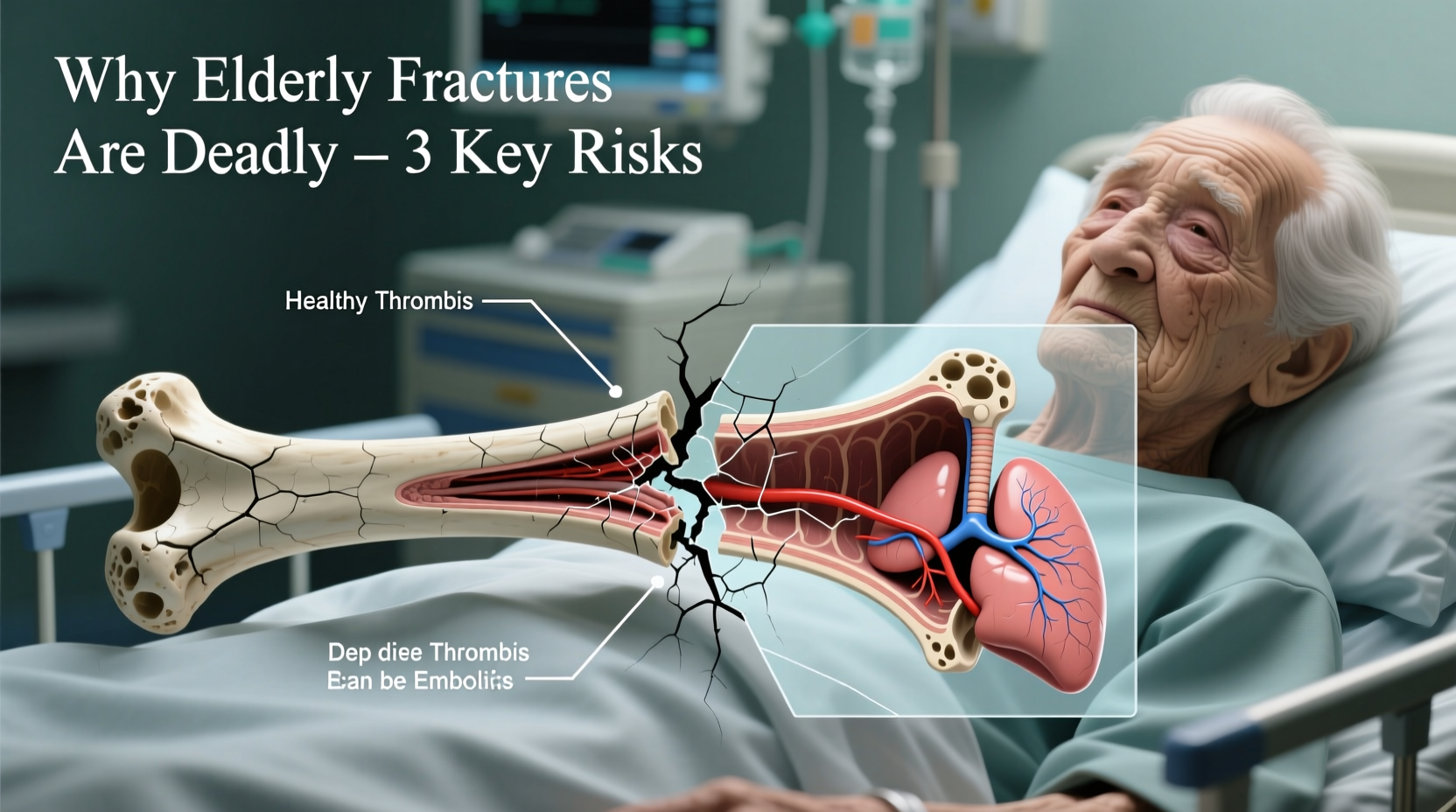
The danger of a broken bone in an older adult isn’t limited to the injury site. Secondary complications arising during recovery pose the greatest threat. These include:
- Pneumonia: Immobility reduces lung expansion, allowing fluid and bacteria to accumulate.
- Deep Vein Thrombosis (DVT) and Pulmonary Embolism: Prolonged sitting or lying down increases clot formation risk, which can travel to the lungs.
- Pressure Ulcers: Constant pressure on skin over bony areas leads to sores that can become infected.
- Urinary Tract Infections (UTIs):strong> Catheter use and reduced mobility contribute to higher infection rates.
- Delirium: Sudden cognitive changes due to pain, medication, infection, or hospital environment.
These conditions often develop rapidly and can spiral into sepsis or organ failure if not caught early. For someone already living with compromised health, even a mild infection can become overwhelming.
Prevention: Reducing Fall and Fracture Risk
Because recovery is so perilous, preventing fractures in the first place is paramount. Most fractures in the elderly result from falls, many of which are preventable. A multifaceted approach involving medical care, home safety, and lifestyle adjustments can dramatically lower risk.
Step-by-Step Guide to Fall Prevention at Home
- Assess balance and strength: Work with a physical therapist to improve stability and muscle support.
- Review medications: Some drugs cause dizziness or drowsiness; consult a doctor about alternatives.
- Improve lighting: Install bright lights in hallways, stairwells, and bathrooms.
- Remove tripping hazards: Secure rugs, clear clutter, and keep cords out of walkways.
- Install grab bars: Place them near toilets, showers, and bathtubs for added support.
- Wear proper footwear: Non-slip, well-fitting shoes should be worn indoors and outdoors.
- Encourage vitamin D and calcium intake: Supports bone density and muscle function.
Medical Interventions That Save Lives
Early diagnosis and treatment of osteoporosis are critical. Bone density scans (DEXA) can identify weakening before a fracture occurs. When indicated, doctors may prescribe medications such as bisphosphonates, denosumab, or teriparatide to strengthen bones.
In the event of a fracture, timely surgical intervention improves outcomes. Hip fracture patients who undergo surgery within 48 hours have lower mortality rates and shorter hospital stays. Post-surgery, coordinated care involving geriatricians, nurses, physical therapists, and nutritionists enhances recovery speed and safety.
| Factor | Risk if Ignored | Recommended Action |
|---|---|---|
| Osteoporosis | 5x higher fracture risk | Bone density test + medication if needed |
| Home hazards | Doubles fall likelihood | Safety audit + modifications |
| Poor nutrition | Slows healing, weakens immunity | Protein-rich diet + vitamin D supplements |
| Medication side effects | Increases dizziness/fall risk | Annual medication review |
Real-Life Example: Maria’s Recovery Journey
Maria, a 78-year-old retired teacher, slipped on a wet kitchen floor and fractured her hip. She underwent surgery within 24 hours and was moved to a rehabilitation center the following week. Her care team included a geriatrician, physical therapist, and dietitian. Within days, she began standing with assistance. By week four, she was walking short distances with a walker.
Crucially, Maria’s family had previously installed grab bars and removed loose rugs—measures that likely prevented earlier falls. Her proactive bone health screening five years prior led to early osteoporosis treatment, which minimized additional fractures. Though recovery was slow, Maria avoided pneumonia, blood clots, and infections thanks to vigilant monitoring and early mobilization.
Her case illustrates how preparation, prompt care, and coordinated support can turn a potentially fatal injury into a manageable one.
Frequently Asked Questions
Can a broken bone really lead to death in older adults?
Yes. While the fracture itself may not be fatal, complications such as pneumonia, blood clots, sepsis, or heart strain due to immobility can be life-threatening. The stress of surgery and recovery also taxes an aging body.
What is the most dangerous type of fracture for seniors?
Hip fractures are among the most serious. They almost always require surgery, lead to long-term immobility, and are associated with high rates of disability and mortality. Spinal compression fractures also carry significant risks, including chronic pain and breathing difficulties.
How long does it take for an elderly person to recover from a broken bone?
Recovery varies widely but generally takes 3 to 6 months for initial healing. Full functional recovery may take a year or longer, and many never return to their previous level of independence. Early rehab and strong social support improve outcomes.
Conclusion: Taking Action Can Save Lives
A broken bone in an elderly person is not a minor injury—it’s a medical emergency with potentially fatal consequences. But with awareness, prevention, and timely intervention, many of these tragedies can be avoided. Families and caregivers play a vital role in creating safe environments, encouraging healthy habits, and ensuring access to medical care.
If you have an aging loved one, start today: schedule a bone density test, conduct a home safety check, and talk to their doctor about fall prevention. Small steps now can prevent devastating outcomes later.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?