Brown discharge in place of a regular menstrual period can be unsettling, especially if it's unexpected or recurring. While it’s often not a sign of serious illness, it can indicate hormonal shifts, early pregnancy, infections, or other underlying conditions. Understanding the root causes and knowing when to seek medical advice is essential for maintaining reproductive health.
Brown discharge is typically old blood that has taken longer to exit the uterus, oxidizing and turning brown before being expelled. Unlike bright red menstrual flow, which suggests fresh bleeding, brownish discharge may appear at the beginning or end of a cycle—or even replace a full period altogether. Though occasional changes are normal, persistent or symptomatic discharge warrants attention.
Common Causes of Brown Discharge Instead of a Period
A variety of physiological and medical factors can lead to brown discharge replacing your expected period. Some are natural and temporary; others may require treatment.
- Hormonal fluctuations: Changes in estrogen and progesterone levels—common during puberty, perimenopause, or after stopping birth control—can delay ovulation and cause spotting or brown discharge.
- Implantation bleeding: One of the earliest signs of pregnancy occurs when a fertilized egg attaches to the uterine lining, causing light spotting 6–12 days after conception. This often appears as brown or pinkish discharge.
- Birth control use: Hormonal contraceptives like pills, IUDs (especially copper and hormonal types), patches, or implants can alter menstrual patterns, leading to irregular bleeding or brown discharge, particularly in the first few months of use.
- Stress and lifestyle factors: High stress, rapid weight loss, excessive exercise, or disrupted sleep can interfere with the hypothalamus, affecting hormone production and delaying or altering periods.
- Pelvic inflammatory disease (PID): Often caused by untreated sexually transmitted infections (STIs) like chlamydia or gonorrhea, PID can result in abnormal discharge, pelvic pain, and irregular cycles.
- Polycystic ovary syndrome (PCOS): Women with PCOS frequently experience irregular or missed periods due to hormonal imbalances, sometimes accompanied by brown discharge when delayed shedding of the uterine lining finally occurs.
- Perimenopause: As women approach menopause (usually in their 40s and early 50s), periods become irregular. Brown spotting between cycles or in place of a full flow is common.
When to Be Concerned: Red Flags to Watch For
While brown discharge alone isn’t always alarming, certain accompanying symptoms suggest the need for prompt medical evaluation.
“Any change in your usual menstrual pattern should be noted. Persistent brown discharge without a clear trigger—especially with pain or odor—deserves clinical assessment.” — Dr. Lena Torres, OB-GYN Specialist
Seek medical advice if you experience any of the following:
- Foul-smelling discharge
- Severe abdominal or pelvic pain
- Fever or chills
- Discharge lasting more than two weeks
- Missed periods for three or more cycles
- Unexplained weight gain or hair growth (possible PCOS)
- Pain during intercourse
Differential Diagnosis Table: Possible Conditions Compared
| Condition | Symptoms | Diagnosis Method | Treatment Approach |
|---|---|---|---|
| Implantation Bleeding | Brief brown/pink spotting, mild cramping | Pregnancy test, ultrasound | Monitoring, prenatal care |
| PCOS | Irregular cycles, acne, weight gain, excess hair | Blood tests, ultrasound | Hormonal therapy, lifestyle changes |
| PID | Foul discharge, fever, pelvic pain | STI testing, pelvic exam | Antibiotics, partner treatment |
| Perimenopause | Hot flashes, mood swings, irregular bleeding | Clinical history, hormone panels | HRT, symptom management |
| Thyroid Disorder | Fatigue, weight changes, hair loss | Blood tests (TSH, T4) | Medication to regulate thyroid function |
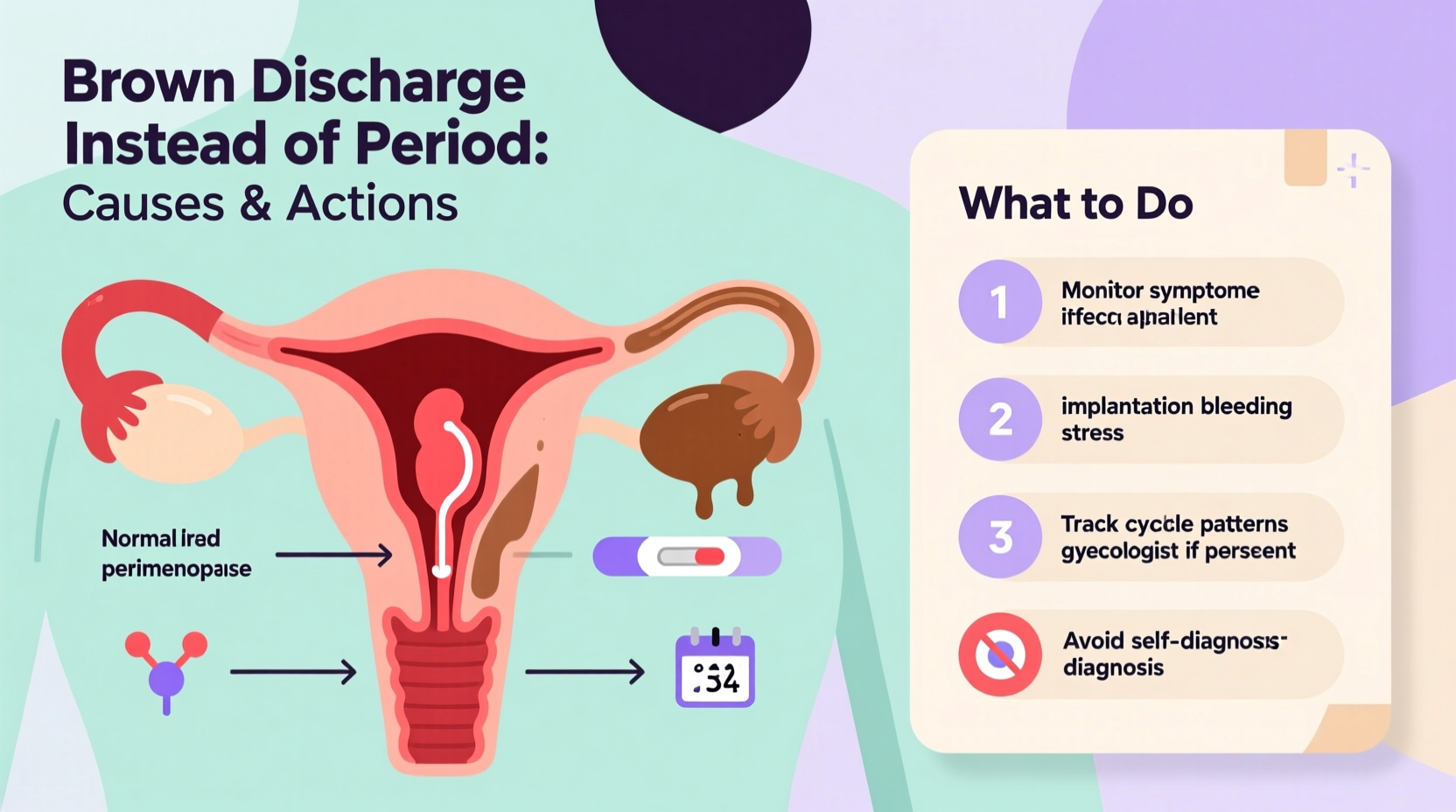
What You Should Do: Step-by-Step Action Plan
If you notice brown discharge instead of your expected period, follow this structured approach to determine next steps:
- Take a pregnancy test: Even if you're on birth control, a home urine test can rule out early pregnancy, including implantation bleeding. Test one week after your missed period for accuracy.
- Review recent lifestyle changes: Consider new medications, stress levels, travel, diet, or exercise routines that might have disrupted your cycle.
- Check for other symptoms: Note any pain, odor, fever, or unusual fatigue that could point to infection or hormonal imbalance.
- Monitor for two weeks: Track the duration, color, and consistency of discharge. Use a journal or app to log observations.
- Schedule a doctor’s visit: If the discharge persists beyond two weeks, recurs monthly, or is accompanied by discomfort, consult a gynecologist for evaluation.
Mini Case Study: Sarah’s Experience with Missed Period and Brown Spotting
Sarah, a 29-year-old graphic designer, noticed her period was five days late. Instead of her usual flow, she experienced light brown discharge for six days. She had recently switched from a combined oral contraceptive to a hormonal IUD three months prior. Initially concerned about pregnancy, she took a home test, which came back negative. After tracking her symptoms and discussing them with her OB-GYN, she learned that her body was still adjusting to the IUD—a common cause of irregular bleeding. Her doctor reassured her and recommended waiting another cycle. By month four, her bleeding normalized.
This case illustrates how medical interventions like IUDs can temporarily disrupt menstrual patterns—and why professional guidance matters in distinguishing between normal adaptation and potential issues.
Prevention and Self-Care Tips
Maintaining menstrual health involves proactive habits that support hormonal balance and overall well-being.
- Maintain a balanced diet rich in iron, omega-3s, and B vitamins to support hormone regulation.
- Exercise moderately—over-exercising can suppress menstruation.
- Avoid smoking and limit alcohol, both of which can affect estrogen levels.
- Stay hydrated and prioritize sleep to support endocrine system function.
Checklist: When to See a Doctor
- ☑ Pregnancy test is positive or inconclusive
- ☑ Discharge lasts longer than 14 days
- ☑ You experience pelvic pain or fever
- ☑ There’s a strong or unpleasant odor
- ☑ You’ve missed three or more periods
- ☑ You’re trying to conceive without success
Frequently Asked Questions
Can brown discharge be a sign of pregnancy?
Yes. Implantation bleeding, which occurs when a fertilized egg attaches to the uterine wall, often presents as light brown or pink spotting around the time of your expected period. A sensitive pregnancy test can confirm this, ideally taken after a missed period.
Is brown discharge normal after stopping birth control?
Yes. After discontinuing hormonal contraception, it can take several months for your natural cycle to regulate. During this time, brown discharge, irregular periods, or anovulatory cycles are common as your body readjusts.
Can thyroid problems cause missed periods and brown discharge?
Absolutely. Both hypothyroidism and hyperthyroidism can disrupt menstrual cycles by affecting hormone production. Blood tests measuring TSH, T3, and T4 levels help diagnose these conditions, which are treatable with medication.
Conclusion: Take Charge of Your Reproductive Health
Brown discharge instead of a period is a common occurrence with diverse causes—from benign hormonal shifts to conditions requiring medical intervention. The key is awareness, observation, and timely action. Don’t dismiss persistent changes in your cycle as “normal” without understanding the context. Whether it’s adjusting to a new IUD, managing stress, or investigating fertility concerns, your body’s signals deserve attention.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?