Burning back pain isn’t just uncomfortable—it can disrupt sleep, limit mobility, and interfere with daily life. Unlike dull or aching pain, a burning sensation often signals nerve involvement or inflammation. Understanding the root cause is essential to effective treatment. This guide breaks down the science behind burning back pain, explores common triggers, and delivers actionable strategies for both immediate comfort and long-term recovery.
What Causes Burning Back Pain?
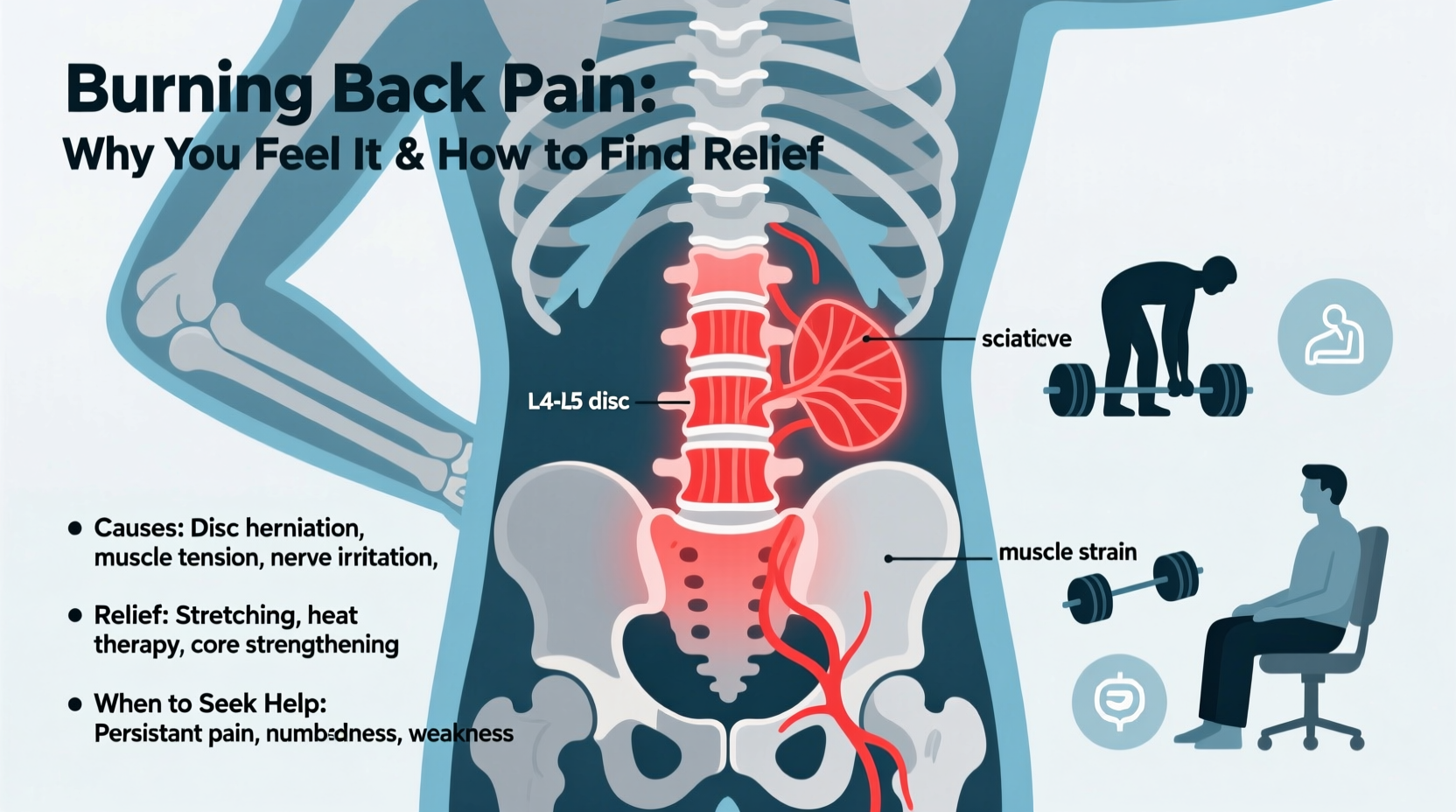
Burning pain in the back typically stems from irritation or damage to nerves along the spine. While muscle strain can cause sharp or throbbing discomfort, a persistent burn suggests neurological activity. The most frequent culprits include:
- Sciatica: Compression of the sciatic nerve leads to a radiating burn from the lower back down the leg.
- Herniated discs: When spinal discs bulge or rupture, they press on nearby nerves, triggering a searing sensation.
- Spinal stenosis: Narrowing of the spinal canal puts pressure on the spinal cord, especially during standing or walking.
- Pinched nerves: Poor posture, injury, or degenerative changes can trap nerves in the lumbar or thoracic spine.
- Diabetic neuropathy: High blood sugar damages peripheral nerves, sometimes manifesting as back burning.
- Infections or tumors: Rare but serious causes that require urgent evaluation.
Secondary factors like prolonged sitting, obesity, and lack of core strength amplify these conditions. Identifying whether your pain originates from mechanical stress or systemic disease determines the right path to relief.
How Nerves Create the Sensation of Burning
Nociceptors are specialized nerve endings that detect tissue damage. When irritated—by compression, inflammation, or chemical changes—they send rapid signals to the brain interpreted as heat or fire. This misfiring is known as neuropathic pain.
In the spine, damaged discs or bone spurs can inflame dorsal root ganglia, clusters of sensory neurons near each vertebra. Once activated, these nerves generate abnormal electrical impulses, leading to chronic burning even without ongoing injury.
“Neuropathic back pain is less about structural damage and more about malfunctioning signaling. That’s why anti-inflammatory drugs alone often fall short.” — Dr. Lena Torres, Neurologist and Pain Specialist
This explains why some patients report intense burning despite clean MRI results. The nervous system becomes hypersensitive, amplifying minor stimuli into severe discomfort—a condition called central sensitization.
Immediate Relief Strategies
While long-term healing requires addressing root causes, managing acute symptoms improves quality of life and supports recovery. Here’s what works:
Cold and Heat Therapy
Apply ice packs for 15–20 minutes during the first 48 hours to reduce inflammation. Afterward, switch to moist heat to relax tight muscles and improve circulation.
Over-the-Counter (OTC) Medications
Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can temporarily ease nerve-related inflammation. Topical creams containing lidocaine or capsaicin may numb localized areas.
Gentle Movement
Contrary to instinct, staying completely still worsens stiffness. Short walks or cat-cow stretches maintain spinal fluidity and prevent nerve adhesions.
| Method | Best For | Caution |
|---|---|---|
| Cold therapy | Acute flare-ups, swelling | Don’t apply directly to skin; limit to 20 min |
| Heat therapy | Chronic stiffness, muscle tension | Avoid with active inflammation |
| NSAIDs | Short-term inflammation control | Limited use due to GI/kidney risks |
| Topical analgesics | Localized burning | Test patch first; avoid broken skin |
Long-Term Healing Approaches
Sustainable relief comes from correcting biomechanical imbalances and reducing nerve irritation over time. Consider integrating the following into your routine:
Physical Therapy
A physical therapist designs targeted exercises to strengthen core stabilizers, improve posture, and decompress affected nerves. Techniques like McKenzie therapy have shown high success rates for disc-related burning pain.
Posture Correction
Slouching while sitting increases disc pressure by up to 300%. Use ergonomic chairs, keep screens at eye level, and take standing breaks every 30 minutes.
Weight Management
Excess body weight, especially around the abdomen, pulls the pelvis forward, straining the lower back. Losing even 10 pounds can significantly reduce spinal load.
Mind-Body Practices
Yoga and tai chi enhance flexibility and body awareness while lowering stress hormones that heighten pain perception. Studies show regular practice reduces chronic back pain intensity by 30–50%.
When to See a Doctor
Most cases of burning back pain respond to conservative care within 6 weeks. However, certain red flags demand prompt medical attention:
- Loss of bladder or bowel control
- Numbness in the saddle area (inner thighs, genitals)
- Progressive leg weakness or foot drop
- Pain worsening at night or unrelated to movement
- History of cancer, infection, or unexplained weight loss
These symptoms could indicate cauda equina syndrome or another serious condition requiring imaging and possibly surgery.
Diagnostic Tools
Doctors may order:
- MRI: Best for visualizing soft tissues, discs, and nerves.
- EMG/Nerve conduction studies: Assess nerve function and pinpoint damage location.
- X-rays: Rule out fractures or alignment issues, though less useful for nerve pain.
Step-by-Step Recovery Plan
Follow this 6-week timeline to regain control over burning back pain:
- Week 1: Begin gentle movement (walking 10–15 min daily), apply ice/heat as needed, and start OTC pain relief if necessary.
- Week 2: Introduce basic stretches (knee-to-chest, pelvic tilts). Evaluate posture habits and adjust workspace setup.
- Week 3: Consult a physical therapist for personalized exercises. Discontinue NSAIDs unless advised otherwise.
- Week 4: Build endurance with low-impact activities like swimming or cycling. Monitor symptom patterns.
- Week 5: Incorporate mind-body practices (yoga, mindfulness) to address pain sensitivity.
- Week 6: Reassess progress. If no improvement, seek further diagnostic evaluation.
Frequently Asked Questions
Can stress cause burning back pain?
Yes. Chronic stress increases muscle tension and alters pain processing in the brain. It can also trigger inflammatory responses that irritate nerves. Managing stress through breathing techniques or counseling often reduces symptom severity.
Is burning back pain a sign of a herniated disc?
It can be. A herniated disc frequently compresses spinal nerves, producing sharp, electric, or burning pain that radiates. However, not all disc issues cause symptoms. Imaging and clinical evaluation are needed for confirmation.
Should I rest or stay active with burning back pain?
Stay moderately active. Complete bed rest beyond 1–2 days slows recovery. Gentle motion keeps joints lubricated and prevents scar tissue formation around nerves. Listen to your body—avoid movements that spike pain.
Real-Life Example: Recovering from Sciatica
James, a 47-year-old office worker, began experiencing a fiery sensation running from his lower back down his left leg after installing new flooring. Initially, he rested and took ibuprofen, but the pain persisted. After two weeks, he consulted a physical therapist who diagnosed sciatica from a mildly herniated L5-S1 disc.
His treatment included nerve gliding exercises, core stabilization work, and ergonomic adjustments at work. Within five weeks, the burning subsided significantly. James now does daily mobility routines and uses a standing desk part-time to prevent recurrence.
Conclusion: Take Control of Your Back Health
Burning back pain doesn’t have to be permanent. Whether caused by nerve compression, poor posture, or systemic factors, relief is possible with informed action. Start with small, consistent changes—improve your sitting posture, add gentle movement, and pay attention to warning signs. Combine self-care with professional guidance when needed, and remember that healing is rarely linear but always achievable.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?