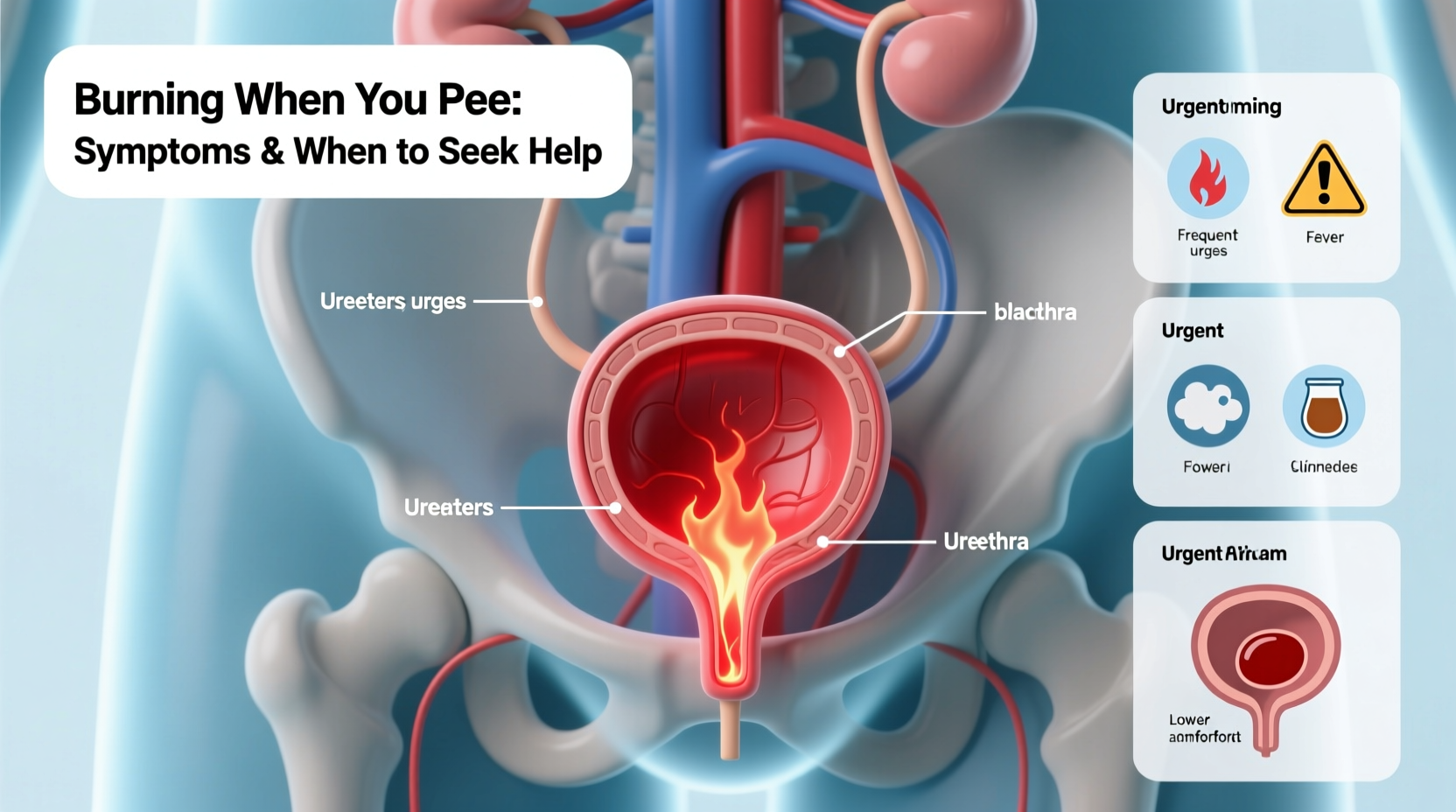
A burning sensation during urination is a symptom many people experience at some point in their lives. While it can be mild and temporary, it may also signal an underlying condition that requires medical attention. Ignoring persistent or worsening discomfort can lead to complications, especially if the cause is an infection or inflammation. Understanding the potential causes, recognizing associated symptoms, and knowing when to consult a healthcare provider are essential steps toward effective treatment and recovery.
Common Causes of Burning During Urination
Burning while urinating—medically known as dysuria—is most often linked to irritation or inflammation in the urinary tract. The causes range from infections to chemical irritants. Some of the most frequent triggers include:
- Urinary Tract Infections (UTIs): Bacteria, most commonly *Escherichia coli*, enter the urethra and multiply in the bladder, causing cystitis. Women are more susceptible due to shorter urethral length.
- Sexually Transmitted Infections (STIs): Chlamydia, gonorrhea, and trichomoniasis can inflame the urethra and lead to painful urination, often accompanied by discharge.
- Vaginal Infections: Yeast infections and bacterial vaginosis alter vaginal pH and may cause external irritation that feels like burning during urination.
- Chemical Irritants: Soaps, douches, spermicides, scented toilet paper, and laundry detergents can trigger localized irritation, especially in sensitive individuals.
- Bladder Inflammation (Interstitial Cystitis): A chronic condition causing bladder pressure, pain, and frequent, urgent urination with a burning sensation.
- Prostatitis: In men, inflammation of the prostate gland can mimic UTI symptoms, including painful urination and pelvic discomfort.
- Kidney Stones: As stones pass through the urinary tract, they can cause sharp pain and a burning sensation during urination.
Symptoms That May Accompany a Burning Sensation
The presence of additional symptoms helps determine the root cause. Not all cases involve infection; however, certain signs indicate a need for prompt evaluation:
| Symptom | Possible Cause |
|---|---|
| Frequent urge to urinate with little output | UTI, interstitial cystitis |
| Cloudy, strong-smelling, or bloody urine | UTI, kidney stones |
| Genital itching or discharge | Yeast infection, STI |
| Pelvic or lower abdominal pain | UTI, prostatitis, interstitial cystitis |
| Fever or chills | Complicated UTI or kidney infection (pyelonephritis) |
In women, symptoms may overlap between vaginal and urinary conditions, making self-diagnosis difficult. Men experiencing dysuria should not assume it’s a minor issue—prostate-related or sexually transmitted causes require professional assessment.
“Patients often delay care because they assume a burning sensation will resolve on its own. But early treatment of infections prevents them from spreading to the kidneys or reproductive organs.” — Dr. Lena Patel, Urologist
When to Seek Medical Help
While occasional, mild burning after sexual activity or dehydration may resolve with hydration and hygiene, certain situations demand immediate medical evaluation:
Seek care immediately if you experience:
- Fever above 101°F (38.3°C), especially with back or side pain
- Nausea or vomiting alongside urinary discomfort
- Blood in the urine (hematuria)
- Inability to urinate despite urgency
- Symptoms lasting more than 24–48 hours without improvement
Pregnant women, older adults, and individuals with diabetes or weakened immune systems should contact a provider at the first sign of dysuria. These groups are at higher risk for rapid progression to kidney infection or sepsis.
For men:
Persistent burning, especially with penile discharge or testicular pain, may indicate an STI or prostatitis. Untreated chlamydia or gonorrhea can lead to infertility. Prostatitis may require antibiotics and anti-inflammatory therapy.
For women:
Recurrent UTIs (three or more per year) warrant further investigation. A pelvic exam, urine culture, or vaginal swab may be needed to differentiate between UTI, yeast, or bacterial vaginosis.
Step-by-Step Guide to Initial Management at Home
If symptoms are mild and you're waiting to see a provider, these steps may offer relief and prevent worsening:
- Stay Hydrated: Drink plenty of water to flush bacteria from the urinary tract. Aim for at least 8 glasses daily.
- Avoid Irritants: Eliminate caffeine, alcohol, spicy foods, and acidic drinks (like citrus juice) that can aggravate the bladder.
- Use a Heating Pad: Apply to the lower abdomen to ease bladder pressure or pelvic discomfort.
- Urinate Frequently: Don’t hold urine. Emptying the bladder regularly reduces bacterial buildup.
- Practice Good Hygiene: Wipe front to back after using the toilet. Urinate after sex to help flush out bacteria.
- Consider OTC Pain Relief: Phenazopyridine (Azo) can temporarily relieve burning but does not treat infection—use only as directed and expect orange-colored urine.
Note: Over-the-counter remedies do not replace antibiotics for bacterial infections. They offer symptomatic relief only.
Real Example: Recognizing When to Act
Sophia, a 28-year-old teacher, noticed a slight burn when urinating after a weekend trip. She assumed it was due to dehydration and increased her water intake. After two days, the discomfort worsened, she began feeling fatigued, and developed a low-grade fever. She also noticed her urine was cloudy and foul-smelling.
She scheduled a same-day clinic visit. A urine test confirmed a UTI with *E. coli*. Her provider prescribed a 5-day course of nitrofurantoin and advised follow-up if symptoms persisted. Within 48 hours of starting antibiotics, her symptoms improved significantly.
Sophia’s case illustrates how a seemingly minor symptom can escalate. Prompt testing prevented the infection from reaching her kidneys—a scenario that could have required hospitalization.
Checklist: What to Do If You Feel a Burn When Urinating
- ✅ Assess severity and duration of symptoms
- ✅ Check for fever, back pain, or blood in urine
- ✅ Increase fluid intake, especially water
- ✅ Avoid irritants like caffeine, alcohol, and scented products
- ✅ Practice proper bathroom hygiene
- ✅ Use OTC pain relief only for temporary comfort
- ✅ Contact a healthcare provider if symptoms last beyond 24–48 hours or worsen
- ✅ Get tested if you’re sexually active—STI screening may be necessary
Frequently Asked Questions
Can dehydration cause a burning sensation when I pee?
Yes. Concentrated urine due to low fluid intake can irritate the lining of the bladder and urethra, causing a temporary burning feeling. This usually resolves with rehydration. However, if the sensation persists after drinking water, another cause should be considered.
Is burning when peeing always a sign of an infection?
No. While infections are a common cause, other factors like chemical irritation, menopause-related vaginal dryness, or chronic conditions such as interstitial cystitis can also produce similar symptoms. Accurate diagnosis requires clinical evaluation.
Can men get UTIs too?
Yes, though less common than in women. Men with UTIs often have an underlying issue such as an enlarged prostate, kidney stones, or a compromised immune system. Symptoms may include burning, frequent urination, and sometimes penile discharge.
Conclusion: Take Action Before It Gets Worse
Burning during urination is your body’s way of signaling that something isn’t right. While it may stem from a minor, self-limiting issue, it can also be the first sign of an infection or condition requiring medical treatment. Self-care measures can help in mild cases, but delaying professional evaluation risks complications like kidney infections or long-term pelvic pain.
Listen to your body. Track your symptoms, stay hydrated, and don’t hesitate to reach out to a healthcare provider when in doubt. Early intervention leads to faster recovery and better outcomes. Your urinary health matters—treat it with the attention it deserves.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?