Calf muscle aches are a common complaint affecting people across all ages and activity levels. Whether you're an athlete, office worker, or weekend hiker, discomfort in the lower leg can disrupt daily life and raise concerns about underlying health issues. While most cases stem from overuse or minor strain, some causes require prompt medical attention. Understanding the root of your calf pain—whether it’s due to dehydration, injury, or circulation problems—can guide appropriate treatment and prevent complications.
Common Causes of Calf Muscle Aches
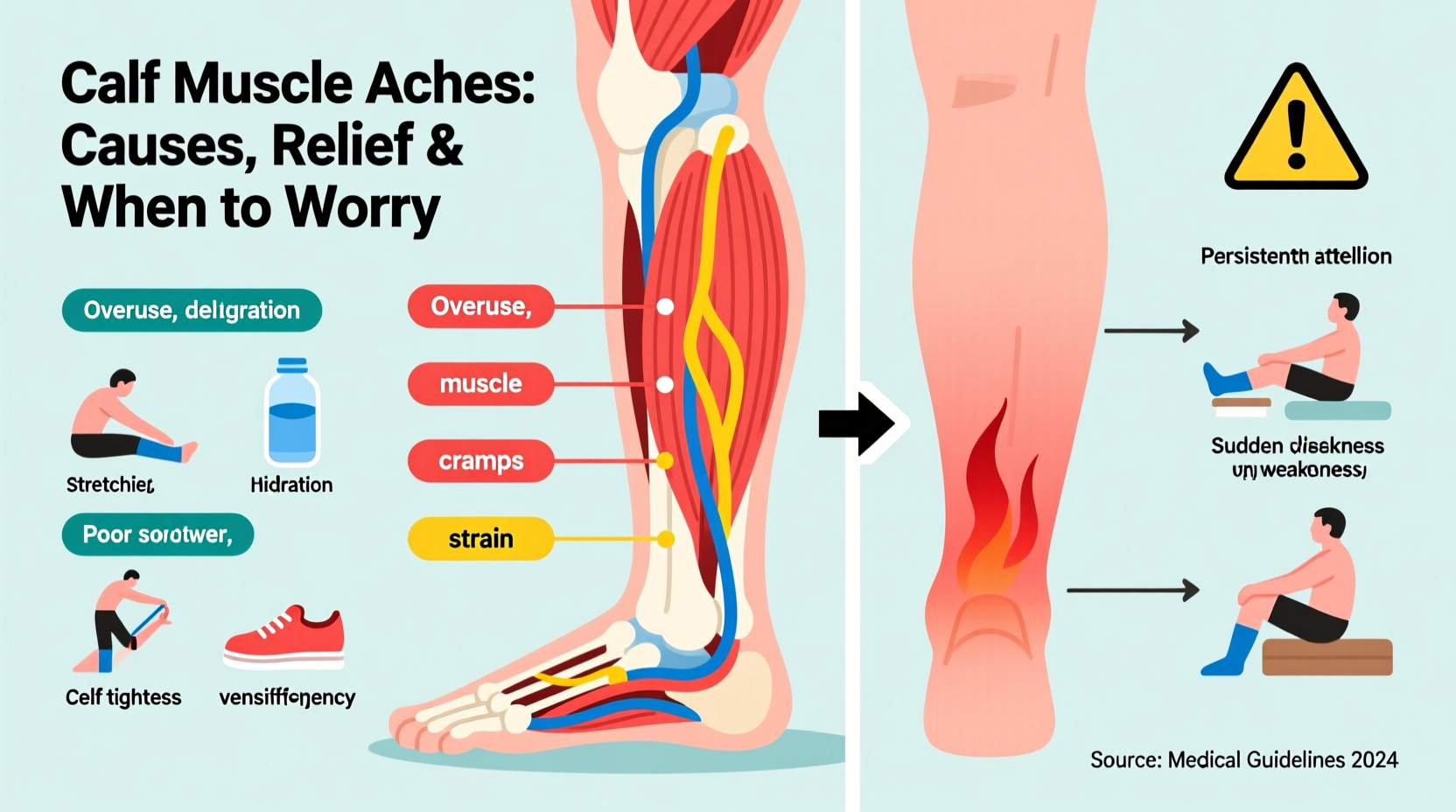
The calf consists primarily of two muscles: the gastrocnemius and soleus. These muscles work together to support walking, running, and jumping. When they become sore or inflamed, several factors may be responsible.
- Overuse or Strain: Sudden increases in physical activity, especially running or jumping, can lead to microtears in muscle fibers, causing soreness.
- Muscle Cramps: Often triggered by dehydration, electrolyte imbalances (especially low potassium, calcium, or magnesium), or prolonged sitting.
- Delayed Onset Muscle Soreness (DOMS): Pain that appears 24–72 hours after unaccustomed exercise.
- Poor Warm-Up or Cool-Down: Skipping stretching routines increases the risk of tightness and strain.
- Peripheral Artery Disease (PAD): Reduced blood flow to the legs causes cramping during activity, which subsides with rest.
- Deep Vein Thrombosis (DVT): A serious condition involving a blood clot in a deep vein, often presenting as sudden, localized calf pain with swelling.
- Nerve Compression: Sciatica or lumbar spine issues can refer pain down to the calf.
- Medication Side Effects: Statins and diuretics are known to cause muscle aches in some individuals.
Effective Relief Strategies
Most calf discomfort resolves with conservative care. The key is identifying the cause and responding appropriately without over-treating minor strains.
Immediate Home Treatments
- Rest: Avoid activities that worsen the pain, especially high-impact exercises.
- Ice Therapy: Apply ice packs for 15–20 minutes every few hours during the first 48 hours to reduce inflammation.
- Compression: Use a light compression wrap to minimize swelling, but avoid wrapping too tightly.
- Elevation: Prop your leg up above heart level when resting to improve circulation.
- Gentle Stretching: Perform slow calf stretches—both straight-knee and bent-knee variations—to relieve tension.
Longer-Term Management
For recurring or chronic calf pain, consider these adjustments:
- Incorporate regular stretching into your routine, particularly before and after workouts.
- Gradually increase exercise intensity to avoid overloading muscles.
- Ensure adequate intake of electrolytes through diet or supplements if needed.
- Wear supportive footwear, especially if you spend long hours on your feet.
- Use foam rolling to release muscle tightness and improve recovery.
“Muscle soreness is often the body’s way of signaling imbalance—either in workload, hydration, or biomechanics. Addressing the root cause prevents recurrence.” — Dr. Lena Torres, Sports Medicine Physician
When to Worry: Red Flags Requiring Medical Attention
While most calf aches are benign, certain symptoms suggest a more serious condition that warrants immediate evaluation.
| Symptom | Possible Cause | Action Required |
|---|---|---|
| Sudden, severe pain with swelling and redness | Deep Vein Thrombosis (DVT) | Seek emergency care—risk of pulmonary embolism |
| Pain that worsens with walking and improves with rest | Peripheral Artery Disease (PAD) | Consult a vascular specialist |
| Numbness, tingling, or weakness in the leg | Sciatic nerve compression or spinal issue | See a neurologist or orthopedic doctor |
| Significant bruising or inability to bear weight | Calf muscle tear or rupture | Medical imaging and possible immobilization |
| Pain accompanied by fever or warmth in the area | Infection or inflammation | Urgent medical assessment needed |
Step-by-Step Guide to Assessing and Managing Calf Pain
Follow this timeline to determine whether your calf ache is manageable at home or requires professional input.
- Day 1 – Onset of Pain: Note when the pain started, what you were doing, and any trauma. Begin R.I.C.E. protocol (Rest, Ice, Compression, Elevation).
- Day 2–3: Monitor changes. If pain decreases, continue gentle movement and stretching. If swelling or discoloration appears, consult a healthcare provider.
- Day 4–7: Gradually reintroduce light activity. Persistent pain beyond one week should be evaluated by a doctor.
- Week 2: If no improvement, seek diagnosis via ultrasound (for DVT), X-ray, or MRI depending on suspected cause.
- Ongoing Prevention: Implement strength training, flexibility work, and proper hydration to reduce future episodes.
Real Example: Recognizing DVT in Time
Mark, a 52-year-old accountant, experienced a dull ache in his left calf after a long international flight. He dismissed it as stiffness from sitting. Over the next 48 hours, the pain intensified, the calf swelled, and the skin became warm and slightly discolored. Concerned, he visited an urgent care clinic where an ultrasound confirmed a deep vein thrombosis. With immediate anticoagulant therapy, he avoided a potentially life-threatening pulmonary embolism. His case underscores how easily serious conditions can be mistaken for simple muscle strain.
Prevention Checklist
Reduce your risk of calf muscle aches with this practical checklist:
- ✅ Warm up before exercise and cool down afterward
- ✅ Stay hydrated, especially during physical activity
- ✅ Maintain balanced electrolyte levels through diet (bananas, leafy greens, nuts)
- ✅ Wear properly fitted shoes with good arch support
- ✅ Stretch calves daily, even if not exercising
- ✅ Avoid prolonged sitting—take standing or walking breaks every hour
- ✅ Gradually increase workout intensity and duration
- ✅ Listen to your body—don’t push through sharp or worsening pain
Frequently Asked Questions
Can calf pain be a sign of a heart problem?
Not directly, but poor circulation due to cardiovascular disease can cause calf pain during walking (claudication). This is often linked to peripheral artery disease, which shares risk factors with heart disease, such as smoking, diabetes, and high cholesterol.
How do I know if my calf pain is a blood clot?
DVT typically presents with one-sided calf pain, swelling, warmth, and redness. The pain may worsen when standing or walking and doesn’t improve with rest or stretching. If you suspect a clot, seek medical attention immediately.
Are calf cramps at night dangerous?
Nocturnal cramps are common, especially in older adults, and usually harmless. However, frequent or severe cramps may indicate dehydration, mineral deficiencies, or nerve issues. Persistent nighttime cramps deserve evaluation to rule out underlying causes.
Conclusion: Take Charge of Your Leg Health
Calf muscle aches are often temporary and manageable with self-care, but they shouldn’t be ignored when warning signs appear. By understanding the difference between ordinary soreness and symptoms of something more serious, you protect not just your mobility but your overall health. Whether you're recovering from a workout or managing chronic discomfort, small changes in hydration, movement, and awareness can make a lasting difference. Pay attention to your body’s signals—early action today can prevent complications tomorrow.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?