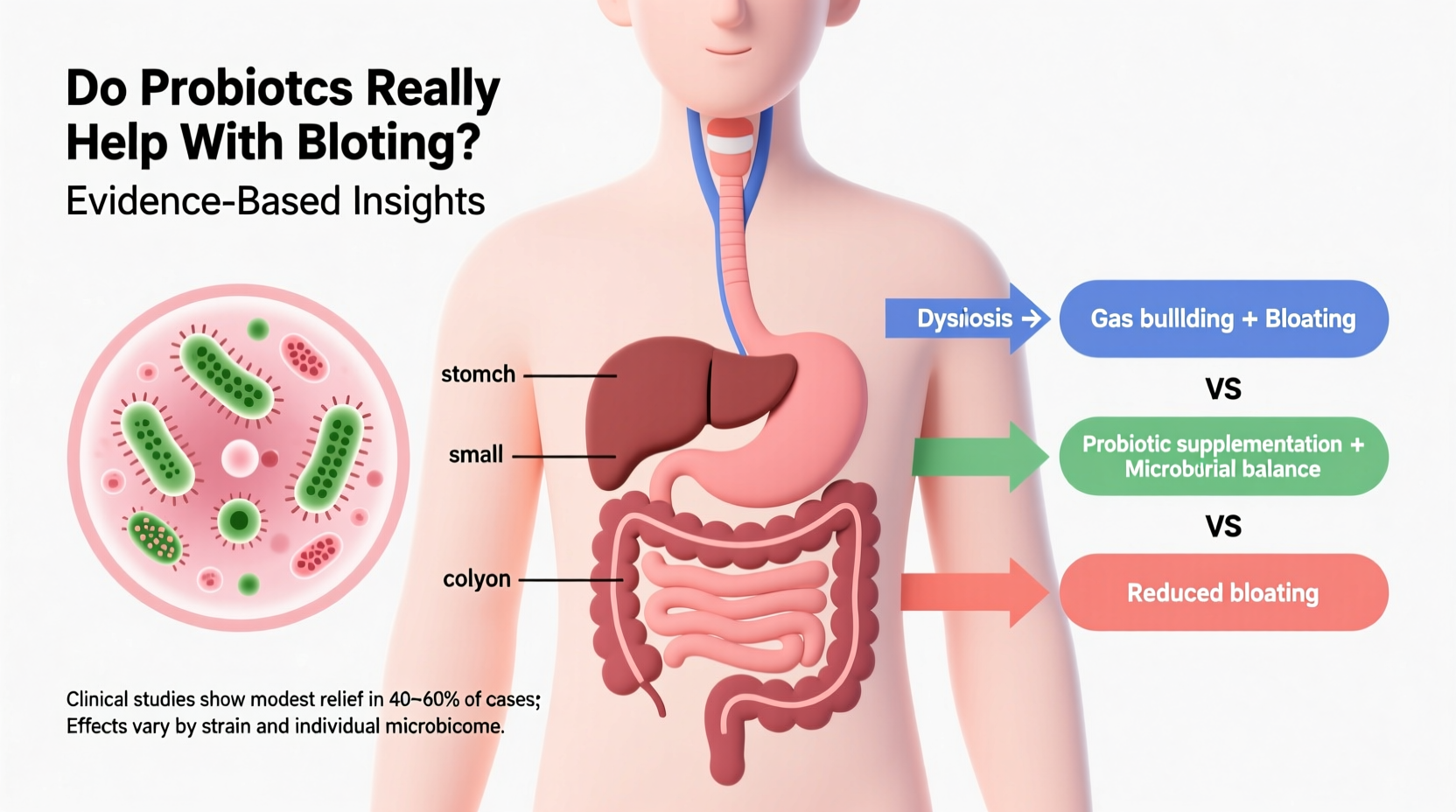
Bloating is one of the most common digestive complaints—millions experience it daily, often after meals or during periods of stress. It’s characterized by a feeling of fullness, tightness, or swelling in the abdomen, sometimes accompanied by gas, discomfort, or even pain. As interest in gut health has surged, probiotics have emerged as a go-to solution for those seeking relief. But are they truly effective, or is the hype outpacing the science?
The answer isn’t a simple yes or no. Probiotics can help some people with bloating—but not all, and not always. Their effectiveness depends on strain specificity, dosage, underlying causes of bloating, and individual gut microbiomes. Understanding when and how they work—and when they might not—is essential to separating real benefit from marketing claims.
How Probiotics Work in the Gut
Probiotics are live microorganisms, primarily bacteria and yeasts, that confer health benefits when consumed in adequate amounts. The most common types belong to the genera Lactobacillus and Bifidobacterium, though others like Saccharomyces boulardii (a beneficial yeast) are also used.
These microbes influence digestion in several ways:
- Restoring microbial balance: Disruptions from antibiotics, poor diet, or illness can tilt the gut microbiome toward harmful bacteria. Probiotics may help reestablish equilibrium.
- Modulating fermentation: Certain strains reduce the production of gas by altering how carbohydrates are broken down in the colon.
- Strengthening the gut barrier: A healthy intestinal lining prevents bacterial translocation and inflammation, both of which can contribute to bloating.
- Reducing visceral hypersensitivity: Some evidence suggests probiotics may calm overactive nerve signals in the gut, decreasing perceived discomfort.
However, not all probiotics act the same. Different strains target different issues. For example, Lactobacillus acidophilus may improve lactose digestion, while Bifidobacterium infantis 35624 has been studied specifically for irritable bowel syndrome (IBS), including bloating symptoms.
What the Research Says About Bloating Relief
Scientific support for probiotics and bloating is promising but nuanced. Clinical trials show mixed results, largely due to variations in study design, participant conditions, and probiotic formulations.
A 2020 meta-analysis published in The American Journal of Clinical Nutrition reviewed 35 randomized controlled trials and found that multi-strain probiotics were more effective than placebo in reducing bloating, particularly in individuals with IBS. However, symptom improvement varied widely—from 20% to 70% across studies.
One landmark trial involving Bifidobacterium infantis 35624 showed significant reductions in bloating, abdominal pain, and bowel irregularity compared to placebo in women with IBS. Another study using a combination of Lactobacillus plantarum and Clostridium butyricum demonstrated faster reduction in post-meal bloating within two weeks.
Yet, not all findings are positive. Some trials report no difference between probiotics and placebo, especially when the cause of bloating isn't microbiome-related. For instance, if bloating stems from small intestinal bacterial overgrowth (SIBO), food intolerances, or motility disorders, probiotics may offer little benefit—or potentially worsen symptoms.
“Probiotics aren’t a universal fix. They’re tools, not magic bullets. Matching the right strain to the right condition is critical.” — Dr. Elena Torres, Gastroenterology Researcher, Johns Hopkins Medicine
When Probiotics Help (and When They Don’t)
Understanding the root cause of bloating is key to determining whether probiotics will help. Below is a breakdown of common scenarios:
| Condition | Can Probiotics Help? | Notes |
|---|---|---|
| Irritable Bowel Syndrome (IBS) | Yes, for some | Strains like B. infantis 35624 and L. plantarum 299v show consistent benefit in clinical trials. |
| Antibiotic-Associated Bloating | Likely yes | Probiotics like S. boulardii and L. rhamnosus GG help prevent dysbiosis caused by antibiotics. |
| Small Intestinal Bacterial Overgrowth (SIBO) | Potentially harmful | Adding more bacteria may exacerbate bloating. Treatment typically requires antibiotics or antimicrobials first. |
| Lactose Intolerance | Mild benefit | Some strains aid lactose digestion, but avoiding dairy or using lactase enzymes is more effective. |
| Constipation-Related Bloating | Maybe | If constipation improves with probiotics, bloating may decrease. Not all strains affect motility. |
| Food Intolerances (e.g., FODMAPs) | Limited impact | Dietary modification (e.g., low-FODMAP) is primary treatment. Probiotics may support but not replace this. |
Real Example: Maria’s Experience with IBS and Probiotics
Maria, a 34-year-old teacher, had struggled with chronic bloating and alternating diarrhea and constipation for years. Diagnosed with IBS-C (constipation-predominant), she tried various over-the-counter remedies with minimal success. Her gastroenterologist recommended a probiotic containing Bifidobacterium lactis HN019 and Lactobacillus acidophilus NCFM.
After three weeks, Maria noticed reduced abdominal distension and more regular bowel movements. By week six, her bloating score dropped from 8/10 to 3/10. She continued the regimen for four months, then gradually tapered off. While symptoms didn’t disappear completely, she gained better control and confidence in managing flare-ups.
Her case illustrates a realistic outcome: partial but meaningful improvement, not a cure. It also highlights the importance of medical guidance—Maria avoided self-prescribing high-dose blends that could have triggered early worsening of gas and bloating.
Choosing the Right Probiotic: A Practical Checklist
Not all probiotics are created equal. To maximize your chances of benefit and minimize risk of disappointment (or side effects), follow this checklist:
- Identify your condition: Are you dealing with IBS, post-antibiotic imbalance, or general discomfort? This guides strain selection.
- Look for clinically studied strains: Choose products with strains proven in human trials for bloating or related symptoms.
- Check CFU count: Doses between 1–10 billion CFUs (colony-forming units) per day are typically sufficient for maintenance; higher doses may be needed short-term.
- Verify shelf life and storage: Some probiotics require refrigeration. Avoid expired or improperly stored products.
- Avoid unnecessary additives: Skip products with fillers, artificial colors, or allergens like dairy or soy if sensitive.
- Start low and slow: Begin with half a dose for the first few days to assess tolerance.
- Give it time: Allow 2–6 weeks before evaluating effectiveness. Microbial shifts take time.
- Discontinue if worsened: If bloating increases significantly, stop use and consult a healthcare provider.
Common Pitfalls and Misconceptions
Despite growing awareness, several myths persist about probiotics and bloating:
- Myth: All probiotics are the same. Reality: Strain, formulation, and delivery method matter profoundly. A yogurt with generic “live cultures” may not help bloating.
- Myth: More CFUs = better results. Reality: High-dose products can overwhelm the gut, causing gas and discomfort, especially initially.
- Myth: Probiotics work immediately. Reality: Most people need at least 1–2 weeks to notice changes. Some see delayed benefits after 4–6 weeks.
- Myth: Natural means safe for everyone. Reality: Immunocompromised individuals or those with severe gut disorders should consult a doctor before use.
Additionally, many consumers overlook the role of prebiotics—fibers that feed beneficial bacteria. While prebiotics like inulin or FOS can enhance probiotic effects, they are fermentable and may actually worsen bloating in sensitive individuals, especially those with IBS.
Step-by-Step Guide to Trying Probiotics for Bloating
If you're considering probiotics, follow this structured approach:
- Week 1: Assess and prepare
- Keep a symptom diary tracking bloating, diet, bowel habits, and stress.
- Rule out serious conditions with a doctor if symptoms are new, severe, or worsening.
- Week 2: Select a targeted product
- Choose a probiotic with strains backed by research for bloating (e.g., B. infantis 35624, L. plantarum 299v).
- Purchase from a reputable brand with third-party testing.
- Weeks 3–4: Begin supplementation
- Take half the recommended dose for the first 3–4 days.
- Gradually increase to full dose with meals to improve survival through the stomach.
- Continue logging symptoms daily.
- Weeks 5–6: Evaluate response
- Compare symptom frequency and severity to baseline.
- If improved, continue for another 4–8 weeks to consolidate gains.
- If no change or worse, discontinue and consider alternative causes.
- Week 7+: Reassess and adjust
- Consult a dietitian or gastroenterologist if unresolved.
- Consider testing for SIBO, food intolerances, or motility issues.
Frequently Asked Questions
Can probiotics make bloating worse?
Yes, especially in the first few days. As the gut microbiome adjusts, increased gas production is common. In individuals with SIBO or histamine intolerance, certain strains may exacerbate symptoms long-term. If bloating persists beyond a week or worsens, stop taking the supplement and consult a professional.
Are probiotic foods like yogurt and kefir enough to relieve bloating?
They can help maintain general gut health, but the strains and concentrations in fermented foods are usually lower and less targeted than in supplements. While beneficial, they may not provide sufficient therapeutic effect for chronic bloating. However, incorporating them into a balanced diet supports overall microbiome diversity.
How long should I take probiotics for bloating?
Most studies showing benefit use probiotics for 4–8 weeks. After that, some people continue long-term, while others taper off. There’s no evidence of harm from prolonged use in healthy individuals, but periodic reassessment is wise. Consider cycling—8 weeks on, 2–4 weeks off—to prevent dependency and monitor ongoing need.
Conclusion: A Measured Approach to Gut Health
Probiotics are neither a miracle cure nor entirely overhyped. For some individuals—particularly those with IBS, antibiotic disruption, or mild dysbiosis—they can offer meaningful relief from bloating. For others, especially those with structural issues, SIBO, or food sensitivities, they may do little or even cause discomfort.
The key lies in informed, personalized use. Rather than blindly trusting labels or influencer endorsements, approach probiotics like any other intervention: with research, caution, and realistic expectations. Pair them with dietary awareness, stress management, and professional guidance when needed.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?