Difficulty taking a deep breath is a sensation many people experience at some point. It can range from a fleeting moment of tightness in the chest after running to a persistent feeling of suffocation that disrupts daily life. While occasional breathlessness may be harmless, recurring or sudden inability to breathe deeply can signal an underlying health issue. Understanding the causes, recognizing associated symptoms, and knowing when to seek medical attention are essential for timely intervention and peace of mind.
Common Causes of Inability to Take a Deep Breath
The sensation of not being able to inhale fully stems from disruptions in the respiratory, cardiovascular, or nervous systems. Some causes are temporary and benign; others require urgent evaluation.
- Anxiety and panic attacks: Hyperventilation, rapid breathing, and chest tightness often accompany anxiety, creating a cycle where fear of not breathing worsens the sensation.
- Asthma: Airway inflammation narrows breathing passages, leading to wheezing, coughing, and a feeling of incomplete inhalation.
- Chronic obstructive pulmonary disease (COPD): Long-term lung damage from smoking or pollution reduces lung elasticity and airflow.
- Heart conditions: Heart failure, arrhythmias, or heart attacks can impair blood oxygenation, causing breathlessness even at rest.
- Pulmonary embolism: A blood clot in the lungs is a medical emergency, often presenting with sudden shortness of breath and sharp chest pain.
- Obesity: Excess weight increases the work of breathing and can compress the diaphragm.
- Pneumonia or lung infections: Fluid or inflammation in the lungs limits air exchange.
- GERD (gastroesophageal reflux disease): Acid reflux can irritate the airways, mimicking respiratory issues.
- Muscle weakness or neuromuscular disorders: Conditions like ALS or myasthenia gravis affect the muscles involved in breathing.
Symptoms That Accompany Breathing Difficulties
The context in which shortness of breath occurs provides critical clues. Isolated breathlessness may be less concerning than when combined with other warning signs.
| Symptom | Possible Implication |
|---|---|
| Chest pain or pressure | Cardiac issue (e.g., heart attack), pulmonary embolism |
| Wheezing or whistling sound | Asthma, COPD, airway obstruction |
| Fatigue and swelling in legs | Heart failure |
| Fever and productive cough | Lung infection such as pneumonia or bronchitis |
| Dizziness or lightheadedness | Hyperventilation, low oxygen, or cardiac event |
| Sudden onset with no prior history | Pulmonary embolism, pneumothorax, or acute asthma attack |
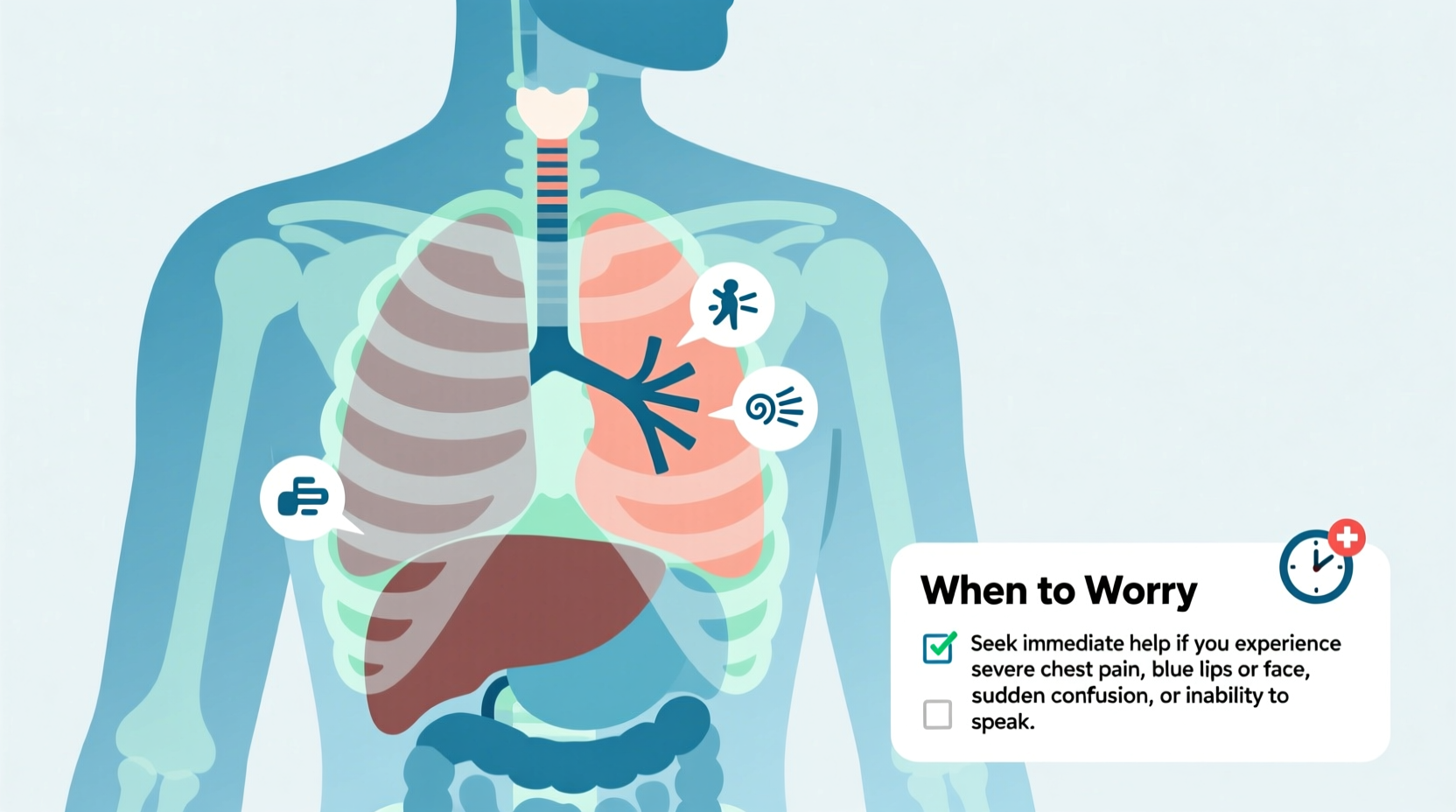
When to Worry: Red Flags Requiring Immediate Attention
Not all cases of breathlessness demand emergency care, but certain signs should never be ignored. The American Thoracic Society emphasizes that sudden or severe difficulty breathing is a red flag.
“Shortness of breath that comes on quickly, especially with chest pain or fainting, requires immediate evaluation. Delaying care can be life-threatening.” — Dr. Alan Reyes, Pulmonologist, Johns Hopkins Medicine
Seek emergency medical help if you experience any of the following:
- Sudden inability to catch your breath, even at rest
- Chest pain that radiates to the arm, neck, or jaw
- Blue lips or fingertips (cyanosis)
- Confusion, dizziness, or near-fainting
- High fever with labored breathing
- Rapid heartbeat (over 120 bpm) without exertion
- Known history of heart or lung disease with worsening symptoms
Mini Case Study: Recognizing a Silent Emergency
Sarah, a 58-year-old office worker, began noticing she couldn’t take a full breath while climbing stairs. She dismissed it as aging and mild fitness decline. Over two weeks, the symptom worsened, occurring while sitting. One evening, she developed sharp chest pain and cold sweats. Her husband called 911. At the hospital, doctors diagnosed a small pulmonary embolism—likely due to prolonged sitting during a recent flight. Prompt treatment saved her life. Sarah’s case illustrates how subtle breathing changes can mask serious conditions.
Diagnosis and Medical Evaluation
If breathlessness persists beyond a few days or recurs frequently, a thorough medical assessment is crucial. Doctors typically follow a stepwise approach:
- Medical history review: Questions about smoking, allergies, medications, and family history of heart or lung disease.
- Physical examination: Listening to lungs and heart, checking oxygen levels, and assessing for swelling or abnormal sounds.
- Lung function tests (spirometry): Measures how much air you can inhale and exhale, helping diagnose asthma or COPD.
- Chest X-ray or CT scan: Detects infections, fluid, tumors, or clots.
- EKG and echocardiogram: Evaluates heart rhythm and pumping function.
- Blood tests: Checks for anemia, infection, or D-dimer (a marker for blood clots).
In some cases, a six-minute walk test or arterial blood gas analysis may be used to assess oxygen delivery and exercise tolerance.
Everyday Tips for Managing Mild Breathing Issues
For those with manageable conditions like mild asthma or anxiety-related breathlessness, lifestyle adjustments can make a significant difference.
Checklist: Daily Habits to Support Easier Breathing
- Practice slow, controlled breathing for 5–10 minutes daily
- Avoid known allergens and indoor pollutants (e.g., smoke, dust, strong perfumes)
- Maintain a healthy weight to reduce strain on the lungs and heart
- Stay up to date on flu and pneumonia vaccines
- Use prescribed inhalers correctly and keep them accessible
- Limit alcohol and caffeine, which can trigger anxiety or acid reflux
- Engage in regular, moderate exercise like walking or swimming
FAQ
Why do I feel like I can’t take a deep breath when I’m lying down?
This may indicate orthopnea, commonly seen in heart failure or severe COPD. When lying flat, fluid can shift into the lungs, making breathing harder. Propping yourself up with pillows often helps. Consult a doctor if this happens regularly.
Can stress really make it hard to breathe?
Yes. During stress or panic, the body enters “fight-or-flight” mode, increasing breathing rate and causing shallow breaths. This can lead to hyperventilation, reducing carbon dioxide levels and causing dizziness and chest tightness. Grounding techniques and paced breathing can restore normal respiration.
Is it normal to feel breathless during pregnancy?
Mild breathlessness is common in pregnancy due to hormonal changes and the growing uterus pressing on the diaphragm. However, sudden or severe shortness of breath, especially with chest pain or swelling, should be evaluated to rule out complications like preeclampsia or pulmonary embolism.
Conclusion: Listen to Your Body and Act Early
Struggling to take a deep breath is more than just discomfort—it’s your body signaling that something may be off. While not every episode indicates a serious problem, ignoring persistent or worsening symptoms can have consequences. Whether the cause is physical, emotional, or a combination, early recognition and professional guidance are key. Keep track of when symptoms occur, what makes them better or worse, and share this information with your healthcare provider. Your breath is vital—protect it with awareness, action, and care.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?