When you visit a doctor with symptoms like chest pain, shortness of breath, or palpitations, two common diagnostic tools often come into play: the electrocardiogram (ECG) and the chest X-ray. While an ECG measures the electrical activity of the heart, a chest X-ray provides a visual image of the heart, lungs, and surrounding structures. It’s not uncommon for both tests to be ordered in sequence—often an ECG first, followed by a chest X-ray. Understanding why this happens and what each test reveals can ease anxiety and help patients make sense of their diagnosis.
Why Is a Chest X-Ray Done After an ECG?
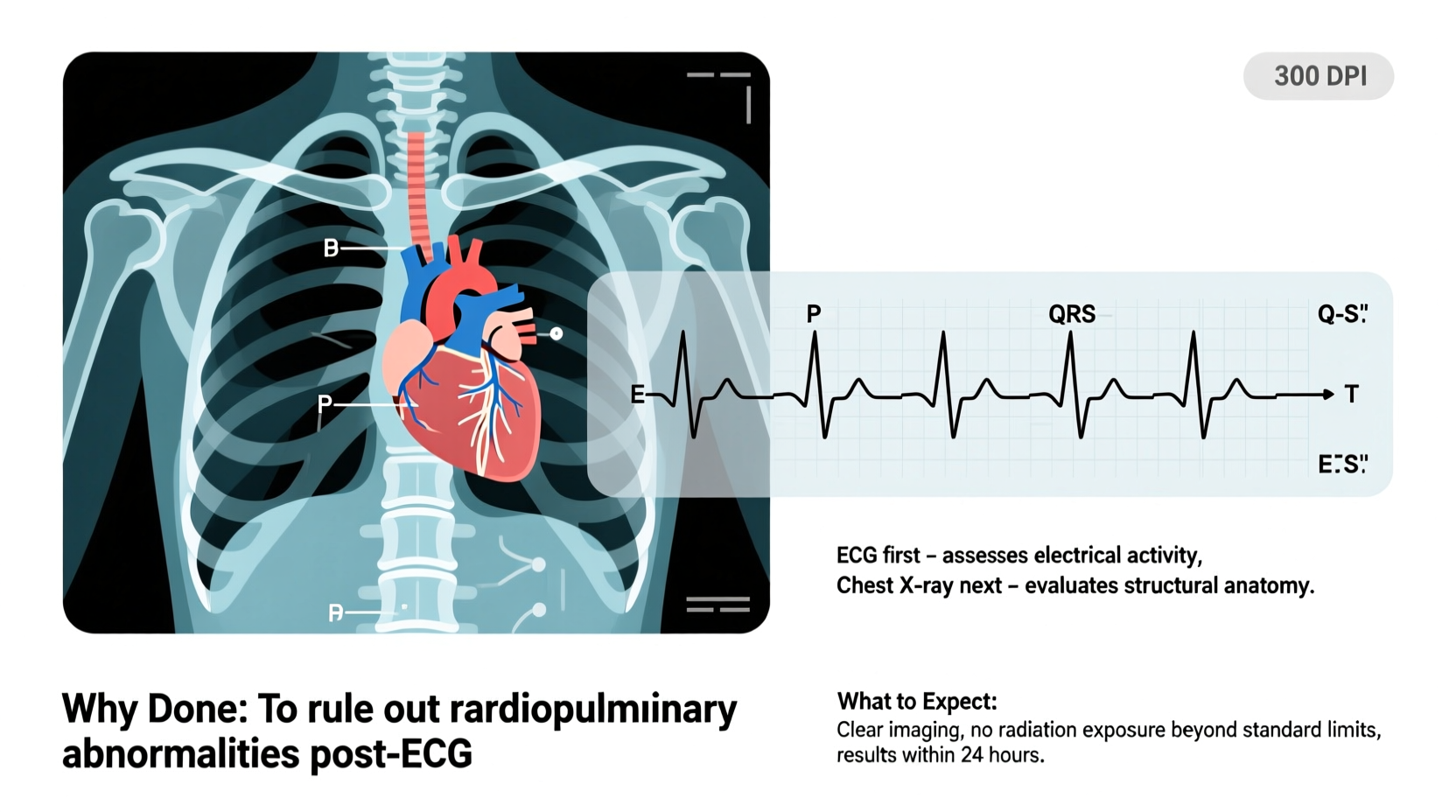
An ECG is typically the first-line cardiac test because it's quick, non-invasive, and highly effective at detecting rhythm abnormalities, signs of ischemia, or previous heart attacks. However, while an ECG gives functional data about the heart’s electrical system, it doesn’t show structural details. That’s where a chest X-ray becomes essential.
A chest X-ray complements the ECG by providing anatomical information. For example, if an ECG shows signs of left ventricular hypertrophy (LVH), a chest X-ray can confirm whether the heart appears enlarged. Similarly, if a patient presents with shortness of breath and the ECG is normal, a chest X-ray might reveal pneumonia, fluid in the lungs (pulmonary edema), or a collapsed lung—conditions that wouldn’t show up on an ECG but could explain the symptoms.
“An ECG tells us how the heart is beating; a chest X-ray tells us how it looks and what’s around it. Together, they offer a more complete clinical picture.” — Dr. Rajiv Mehta, Cardiologist, Cleveland Heart Institute
What Conditions Can Be Detected?
The combination of ECG and chest X-ray helps clinicians evaluate a wide range of conditions:
- Heart failure: An ECG may show arrhythmias or signs of strain, while a chest X-ray can reveal an enlarged heart or fluid buildup in the lungs.
- Pneumonia or lung infection: The ECG might be normal, but the X-ray clearly shows infiltrates or consolidation in the lungs.
- Pulmonary hypertension: ECG changes may suggest right heart strain, and X-rays can show enlarged pulmonary arteries or right ventricle.
- Pleural effusion: Fluid around the lungs is invisible on ECG but easily seen on X-ray.
- Pericardial effusion: A “water bottle” appearance of the heart on X-ray, possibly linked to electrical alternans on ECG.
- COPD or emphysema: Hyperinflated lungs visible on X-ray, sometimes associated with P-pulmonale on ECG.
Step-by-Step: What to Expect During the Process
Understanding the flow of testing can reduce uncertainty. Here’s what typically happens when a chest X-ray follows an ECG:
- Initial consultation: Your doctor reviews your symptoms and medical history.
- ECG (5–10 minutes): Electrodes are placed on your chest, arms, and legs. You lie still while the machine records your heart’s electrical activity.
- Review of ECG results: The physician examines the tracing for arrhythmias, ischemia, or structural clues.
- Referral for chest X-ray: Based on ECG findings or persistent symptoms, a chest X-ray is ordered.
- Chest X-ray (10–15 minutes): You stand or sit in front of an imaging plate. Two views are usually taken: one from the back to the front (PA view) and one from the side (lateral view).
- Image interpretation: A radiologist analyzes the X-ray for heart size, lung clarity, bone integrity, and signs of disease.
- Integrated diagnosis: Both reports are combined to form a comprehensive assessment.
No special preparation is needed for either test. You remain fully clothed, though you may need to change into a gown if your clothing has metal components. The entire process—from ECG to X-ray—usually takes under 30 minutes in outpatient settings.
Do’s and Don’ts Before and After Testing
| Do’s | Don’ts |
|---|---|
| Wear comfortable, easy-to-remove clothing | Wear jewelry or metal accessories during the X-ray |
| Inform your doctor of pregnancy (especially for X-ray) | Delay reporting symptoms like severe chest pain |
| Breathe normally during ECG; hold breath briefly during X-ray | Move during image capture—it can blur the X-ray |
| Bring prior test results if available | Assume a normal ECG means everything is fine—structural issues may still exist |
Real-World Example: When Both Tests Made the Difference
Consider Mr. Thompson, a 68-year-old man who visited his clinic complaining of fatigue and mild shortness of breath. His ECG showed atrial fibrillation with a rapid ventricular response. While this explained his palpitations, it didn’t account for his worsening breathlessness. A chest X-ray was ordered immediately.
The X-ray revealed cardiomegaly (an enlarged heart) and vascular congestion in the lungs—classic signs of congestive heart failure. With this combined data, his physician initiated appropriate treatment: rate control medication, diuretics, and referral to a cardiologist. Without the chest X-ray, the extent of heart involvement might have been missed, delaying critical care.
This case illustrates how functional and structural tests together guide accurate, timely intervention.
Frequently Asked Questions
Can a chest X-ray detect a heart attack?
Not directly. A chest X-ray cannot diagnose an acute heart attack like an ECG or blood tests (e.g., troponin levels) can. However, it may show indirect signs such as an enlarged heart, fluid in the lungs, or changes in heart shape that suggest prior damage or complications from a heart attack.
Is radiation from a chest X-ray dangerous?
The radiation dose from a standard chest X-ray is very low—about 0.1 mSv, equivalent to 10 days of natural background radiation. The benefits of accurate diagnosis far outweigh the minimal risk, especially when medically indicated.
Why do I need both tests if one seems normal?
Each test evaluates different aspects. An ECG might be normal even if there’s lung disease, and a chest X-ray might appear clear despite serious arrhythmias. Using both increases diagnostic accuracy and reduces the chance of missing underlying conditions.
Preparing Mentally and Physically: Tips for a Smooth Experience
Many patients feel anxious about medical tests, especially those involving the heart. Here’s how to prepare effectively:
- Stay informed: Ask your doctor why each test is being ordered and how results will influence your care.
- Practice relaxation: Deep breathing can help if you’re nervous during the ECG, which requires lying still.
- Bring a list of medications: This helps doctors interpret findings in context.
- Ask about follow-up: Know when and how you’ll receive results.
Conclusion: Taking Control of Your Cardiovascular Health
Having a chest X-ray after an ECG isn’t a sign of something going wrong—it’s a sign of thorough, thoughtful medicine. These two tests serve different but complementary roles in evaluating your heart and lungs. Whether you’re being assessed for chest pain, shortness of breath, or routine monitoring, understanding the purpose and process empowers you to participate actively in your healthcare.
Don’t hesitate to ask questions, follow through on recommendations, and share concerns with your provider. Early detection and accurate diagnosis are the foundation of effective treatment. By staying informed and proactive, you take meaningful steps toward better heart and lung health.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?