For many, occasional difficulty passing stool is a minor inconvenience. But when bowel movements become infrequent, painful, or incomplete over weeks or months, it may signal chronic constipation—a condition affecting nearly 15% of adults globally. More than just discomfort, chronic constipation can interfere with quality of life, energy levels, and overall health. Understanding its root causes and knowing how to manage symptoms effectively is essential for lasting relief.
What Defines Chronic Constipation?
Medically, chronic constipation is diagnosed when symptoms persist for at least three months, with onset at least six months prior. The Rome IV criteria—widely used in gastroenterology—define it by two or more of the following:
- Straining during bowel movements more than 25% of the time
- Hard or lumpy stools more than 25% of the time
- Sensation of incomplete evacuation
- Feeling of anorectal blockage
- Need for manual maneuvers (e.g., digital disimpaction) to pass stool
- Less than three bowel movements per week
It’s not simply about frequency. The consistency of stool, effort required, and sense of completion are all key indicators. If these patterns disrupt daily life, it’s time to look deeper than temporary fixes like laxatives.
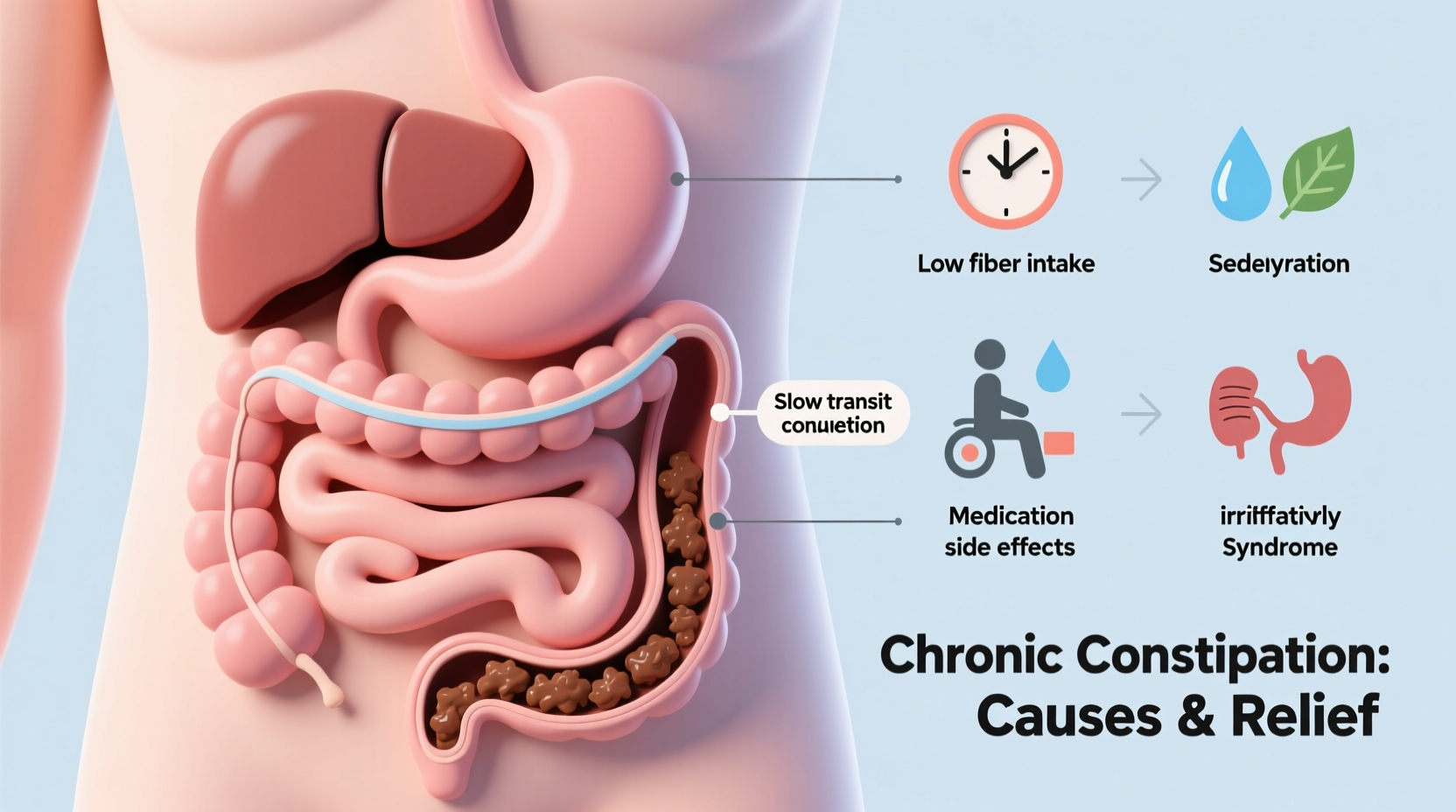
Common Causes Behind Persistent Constipation
Chronic constipation rarely has a single cause. It typically results from a combination of lifestyle, physiological, and medical factors. Identifying which apply is crucial for targeted treatment.
Dietary Deficiencies
A low-fiber diet is one of the most common contributors. Fiber adds bulk to stool and helps it move through the intestines. Diets high in processed foods, dairy, and red meat while lacking fruits, vegetables, and whole grains slow digestion significantly.
Inadequate Hydration
Water softens stool. When the body is dehydrated, the colon absorbs more water from waste, leading to dry, hard stools that are difficult to pass.
Sedentary Lifestyle
Lack of physical activity slows intestinal motility. Even moderate exercise like walking stimulates the muscles involved in bowel contractions.
Medications
Certain drugs contribute to constipation as a side effect. These include:
- Opioid painkillers
- Antidepressants (especially tricyclics)
- Calcium channel blockers for blood pressure
- Iron supplements
- Antacids containing aluminum or calcium
Underlying Medical Conditions
Several conditions affect gut function:
- Irritable Bowel Syndrome (IBS-C): Constipation-predominant IBS involves altered gut-brain signaling.
- Diabetes: Nerve damage (diabetic neuropathy) can impair intestinal motility.
- Hypothyroidism: Low thyroid hormone slows metabolism and digestion.
- Parkinson’s disease: Neurodegeneration impacts autonomic nervous system control of bowels.
- Colon strictures or tumors: Physical obstructions require immediate evaluation.
“Chronic constipation isn’t something to just ‘live with.’ It’s often a sign of an underlying imbalance that needs attention.” — Dr. Lena Patel, Gastroenterologist, Johns Hopkins Medicine
Effective Relief Strategies That Work
Relief begins with sustainable changes, not quick fixes. While laxatives have their place, long-term management relies on addressing root causes.
1. Optimize Your Diet
Increase both soluble and insoluble fiber gradually to avoid bloating. Aim for 25–35 grams daily from sources like:
- Leafy greens, broccoli, carrots
- Legumes (lentils, chickpeas)
- Whole grains (oats, quinoa, brown rice)
- Fruits with skin (apples, pears, berries)
Prunes are particularly effective due to their natural sorbitol content, a sugar alcohol that draws water into the colon.
2. Hydrate Strategically
Drink at least 8 cups (64 oz) of water daily. Warm liquids in the morning—like herbal tea or warm lemon water—can stimulate the gastrocolic reflex, triggering bowel movement.
3. Move Your Body
Engage in 30 minutes of moderate exercise most days. Walking, cycling, or yoga—especially poses like knees-to-chest or spinal twists—can enhance colonic transit.
4. Establish a Bathroom Routine
Go at the same time daily, ideally 15–30 minutes after breakfast. This leverages the body’s natural post-meal motility surge. Don’t rush; allow time without distractions.
5. Consider Targeted Supplements
When dietary changes aren’t enough, certain supplements may help:
| Supplement | How It Works | Recommended Use |
|---|---|---|
| Magnesium citrate | Draws water into the colon | 200–400 mg before bed |
| Psyllium husk | Bulking agent, improves stool consistency | 1 tsp in water daily, with extra fluids |
| Probiotics (e.g., Bifidobacterium strains) | Support gut microbiome balance | Daily, preferably refrigerated brands |
When Laxatives Are Necessary—and When to Avoid Them
Not all laxatives are equal. Overuse of stimulant types (e.g., senna, bisacodyl) can lead to dependency and weakened bowel tone. Use them only short-term unless directed otherwise by a doctor.
Better options for ongoing use include:
- Osmotic agents: Polyethylene glycol (PEG/Miralax) pulls water into the colon safely over time.
- Bulking agents: Psyllium or methylcellulose increase stool mass naturally.
Always pair laxative use with lifestyle adjustments. They should support—not replace—long-term digestive health.
Real-Life Example: Maria’s Turnaround
Maria, a 48-year-old office worker, struggled with constipation for over two years. She relied on stimulant laxatives weekly but felt bloated and fatigued. After consulting a dietitian, she discovered her routine included little fiber, minimal movement, and frequent dehydration.
She began incorporating oatmeal with chia seeds for breakfast, added a 20-minute walk after lunch, and committed to drinking two liters of water daily. Within six weeks, her bowel movements normalized without laxatives. A follow-up blood test also revealed mild hypothyroidism, which was treated with medication. Her case highlights how combining self-management with medical evaluation leads to lasting improvement.
Step-by-Step Guide to Restoring Regularity
Follow this 4-week plan to reset your digestive rhythm:
- Week 1: Track food, water intake, and bowel movements. Identify low-fiber meals and dehydration patterns.
- Week 2: Add one high-fiber food at each meal (e.g., avocado at breakfast, salad at lunch, steamed veggies at dinner). Begin daily walks.
- Week 3: Introduce a fiber supplement like psyllium. Set a consistent bathroom time each morning.
- Week 4: Evaluate progress. If improvement is limited, consult a healthcare provider to rule out medical causes.
FAQ: Common Questions About Chronic Constipation
Can stress really cause constipation?
Yes. The gut and brain are closely linked via the vagus nerve. Chronic stress alters gut motility and can delay transit time. Mind-body practices like meditation or diaphragmatic breathing may improve symptoms.
Is it dangerous to go several days without a bowel movement?
Occasionally, no—but if it becomes routine and is accompanied by abdominal pain, nausea, or bloating, it could indicate fecal impaction or a structural issue. Seek medical advice if symptoms persist beyond a week despite interventions.
Are enemas safe for regular use?
No. Regular use of enemas can disrupt electrolyte balance and reduce natural bowel reflexes. They should be reserved for acute relief under medical guidance.
Conclusion: Take Control of Your Digestive Health
Chronic constipation is not a life sentence. With careful attention to diet, hydration, movement, and underlying health, most people can achieve reliable relief. The goal isn’t just more frequent bowel movements—it’s restoring the body’s natural rhythm and preventing recurrence. Small, consistent changes often yield the most powerful results. If symptoms persist despite your efforts, don’t hesitate to seek professional evaluation. Your digestive health is foundational to your overall well-being.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?