Waking up with cold, damp palms. Feeling your shirt stick to your back during a meeting. Noticing sweat beads form on your forehead even in cool weather—these are signs of clammy and sweaty skin, a condition that affects millions. While occasional sweating is normal, persistent or unexplained dampness can signal underlying health issues, environmental triggers, or lifestyle factors. Understanding the root causes and knowing how to respond makes a significant difference in comfort, confidence, and long-term well-being.
What Does “Clammy and Sweaty” Really Mean?
Clamminess refers to skin that feels cool, moist, and sticky—often accompanied by pallor or chills. Unlike regular sweating due to heat or exercise, clammy skin typically results from the body’s response to stress, illness, or autonomic nervous system activity. It often appears on the palms, feet, forehead, and underarms but can spread across the body.
Sweating itself is a natural cooling mechanism. The eccrine glands release moisture (mostly water and salt) to regulate temperature. However, when this process activates without physical exertion or high temperatures, it may point to something deeper than overheating.
Common Causes of Clammy and Sweaty Skin
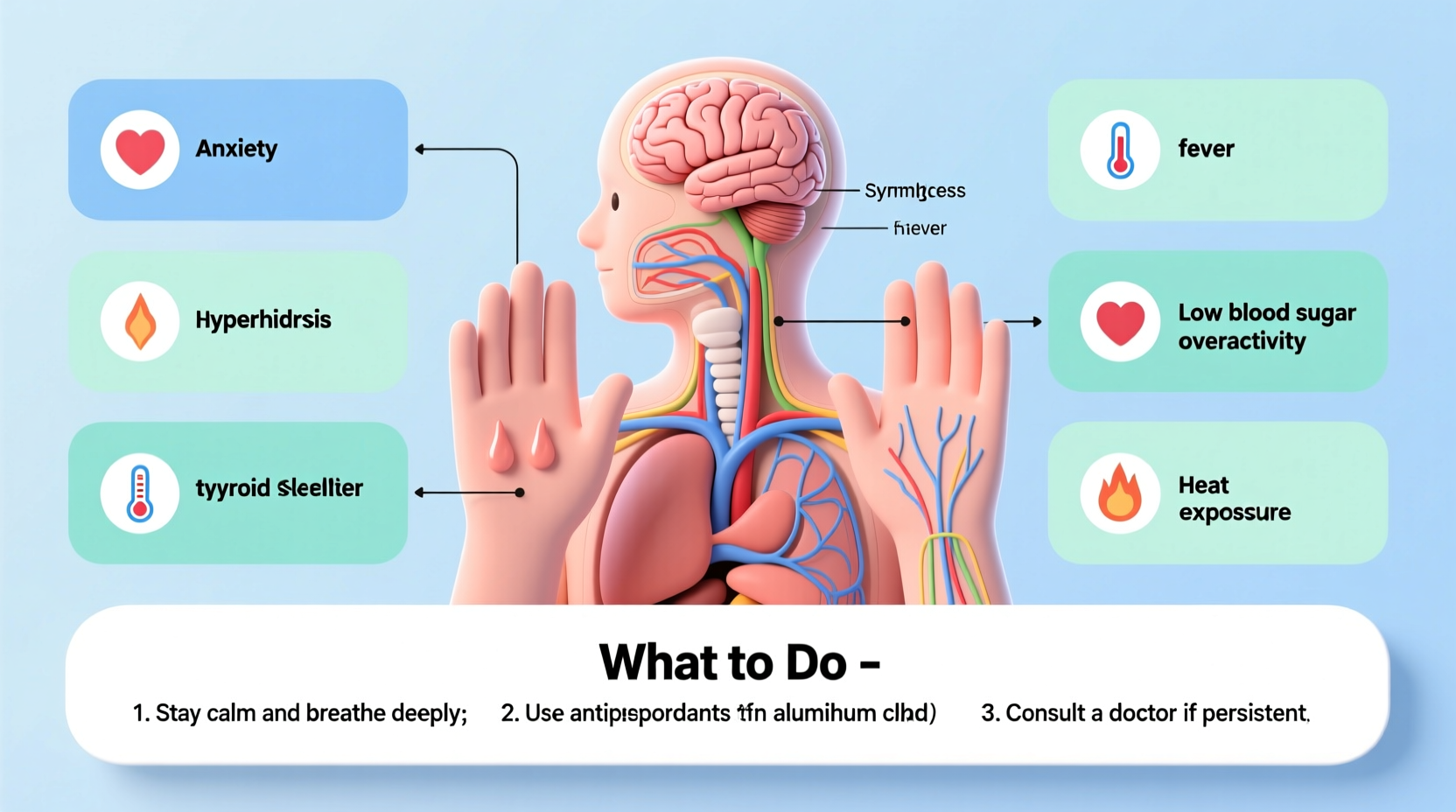
Several factors contribute to excessive or inappropriate sweating. These range from temporary triggers to chronic medical conditions.
1. Emotional Stress and Anxiety
The sympathetic nervous system kicks in during emotional distress, triggering sweat production as part of the “fight-or-flight” response. This type of sweating primarily affects the palms, soles, and armpits—even in cool environments.
2. Low Blood Sugar (Hypoglycemia)
When blood glucose drops—common in people with diabetes or those who skip meals—the body releases adrenaline, which stimulates sweat glands. Symptoms include trembling, dizziness, hunger, and sudden onset of clamminess.
3. Infections and Fever
Bacterial or viral infections prompt the immune system to raise body temperature. As fever breaks, the body cools down through sweating, often leaving the skin damp and cool to the touch.
4. Cardiovascular Issues
Heart attacks, angina, or shock can cause sudden, intense sweating unrelated to temperature. Clammy skin combined with chest pain, shortness of breath, or nausea requires immediate medical attention.
“Cold sweats without exertion can be a red flag for cardiovascular distress. Don’t ignore them, especially if paired with chest discomfort.” — Dr. Lena Torres, Cardiologist
5. Hyperhidrosis
This chronic condition involves overactive sweat glands, leading to excessive sweating beyond what’s needed for thermoregulation. It can be localized (e.g., hands, feet) or generalized. Primary hyperhidrosis has no clear cause; secondary hyperhidrosis stems from another condition like thyroid disease or medication side effects.
6. Hormonal Changes
Menopause, pregnancy, and thyroid disorders (especially hyperthyroidism) disrupt hormonal balance, increasing metabolic rate and heat production, which leads to more frequent sweating.
7. Medications and Substances
Antidepressants, opioids, hormone therapies, and some diabetes medications list sweating as a side effect. Withdrawal from alcohol or drugs can also induce severe night sweats and clamminess.
Do’s and Don’ts: Managing Clammy Skin
| Do | Avoid |
|---|---|
| Wear breathable, moisture-wicking fabrics like cotton or bamboo | Synthetic materials that trap heat and moisture |
| Use clinical-strength antiperspirants at night | Overusing deodorants that don’t block sweat |
| Stay hydrated to support natural temperature regulation | Dehydration, which stresses the body’s cooling systems |
| Monitor symptoms and keep a symptom journal | Ignoring recurring episodes without seeking evaluation |
| Practice relaxation techniques like meditation or yoga | High-caffeine or spicy foods that trigger flare-ups |
Step-by-Step Guide to Addressing Excessive Sweating
- Track Your Episodes: Note when sweating occurs, duration, location, and any triggers (stress, food, time of day).
- Review Medications: Consult your doctor about whether prescriptions could be contributing.
- Adjust Lifestyle Factors: Reduce caffeine, avoid spicy foods, wear layered clothing, and maintain good hygiene.
- Try Over-the-Counter Solutions: Use aluminum-based antiperspirants nightly for better absorption.
- Seek Medical Evaluation: If sweating interferes with daily life, see a healthcare provider to rule out conditions like hyperthyroidism, diabetes, or heart disease.
- Explore Advanced Treatments: Depending on diagnosis, options include prescription wipes (e.g., Qbrexza), Botox injections, iontophoresis, or surgery.
Real-Life Example: When Sweating Was a Warning Sign
Mark, a 52-year-old accountant, began experiencing frequent episodes of cold sweats at work. He dismissed them as stress-related until one afternoon he felt lightheaded, nauseous, and suddenly soaked in sweat while sitting at his desk. His colleague noticed his pale face and insisted he go to urgent care. Tests revealed unstable angina—a warning sign of an impending heart attack. Early intervention prevented a major cardiac event. Mark now manages his condition with medication, lifestyle changes, and regular monitoring. His story underscores that not all sweating is benign.
When to Seek Immediate Medical Help
While many cases of clammy skin resolve on their own, certain symptoms demand urgent attention:
- Chest pain or pressure
- Rapid heartbeat or palpitations
- Dizziness or fainting
- Shortness of breath
- Confusion or disorientation
- Sudden, unexplained sweating with no trigger
If these accompany clamminess, call emergency services immediately. Sudden cold sweats can indicate heart attack, septic shock, or severe hypoglycemia—all requiring rapid treatment.
Effective Home and Long-Term Management Strategies
For non-emergency cases, consistent self-care can significantly reduce discomfort.
Consider using absorbent powders or foot sprays if sweating affects your feet. For hand sweating, portable sweat wipes or iontophoresis devices (which use mild electrical currents to reduce sweat) offer relief. Air conditioning, fans, and staying in cooler environments help minimize triggers.
Mind-body practices such as biofeedback, cognitive behavioral therapy (CBT), and acupuncture have shown promise in reducing stress-related sweating. A 2020 study published in *The Journal of Clinical and Aesthetic Dermatology* found that patients with hyperhidrosis who practiced mindfulness reported a 30% reduction in symptom severity over eight weeks.
Frequently Asked Questions
Why do I sweat when I’m nervous but not when I exercise?
Nervous sweating is controlled by the emotional centers of the brain and tends to activate the palms and soles more intensely. Exercise-related sweating is thermoregulatory and spreads evenly across the body. The two systems operate independently, explaining the difference in patterns.
Can diet affect how much I sweat?
Yes. Spicy foods, hot beverages, alcohol, and caffeine stimulate the nervous system and increase internal heat, prompting sweat. Reducing intake of these can lead to noticeable improvement, especially in sensitive individuals.
Is there a cure for hyperhidrosis?
There’s no universal “cure,” but effective treatments exist. Many people achieve long-term control with antiperspirants, medications, or procedures like Botox or miraDry. In severe cases, endoscopic thoracic sympathectomy (ETS) surgery may be considered, though it carries risks like compensatory sweating elsewhere.
Take Control of Your Comfort and Health
Clammy and sweaty skin isn’t just uncomfortable—it can impact confidence, social interactions, and quality of life. But most causes are manageable with the right approach. Whether it’s adjusting your wardrobe, addressing anxiety, or ruling out medical concerns, small, informed actions make a big difference. Pay attention to your body’s signals. Track changes. And never hesitate to consult a professional if sweating feels out of sync with your environment or activities.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?