Coughing up blood—medically known as hemoptysis—is a symptom that can range from a few streaks in mucus to large volumes of pure blood. While it may not always signal a life-threatening condition, it should never be ignored. The presence of blood in sputum can originate from the lungs, bronchial tubes, or upper respiratory tract, and its underlying cause varies widely. Understanding the potential reasons behind this symptom and recognizing when immediate medical attention is necessary can make a critical difference in outcomes.
What Does Coughing Blood Look Like?
The appearance of coughed-up blood can vary significantly. It might appear:
- Fresh and bright red, mixed with frothy sputum
- Streaked through clear or yellow mucus
- Dark and rust-colored, resembling coffee grounds (less common in true hemoptysis)
It's important to distinguish hemoptysis from bleeding originating in the gastrointestinal tract (hematemesis), where blood is vomited and often darker due to stomach acid. True hemoptysis comes from the respiratory system and is typically accompanied by coughing, chest discomfort, or shortness of breath.
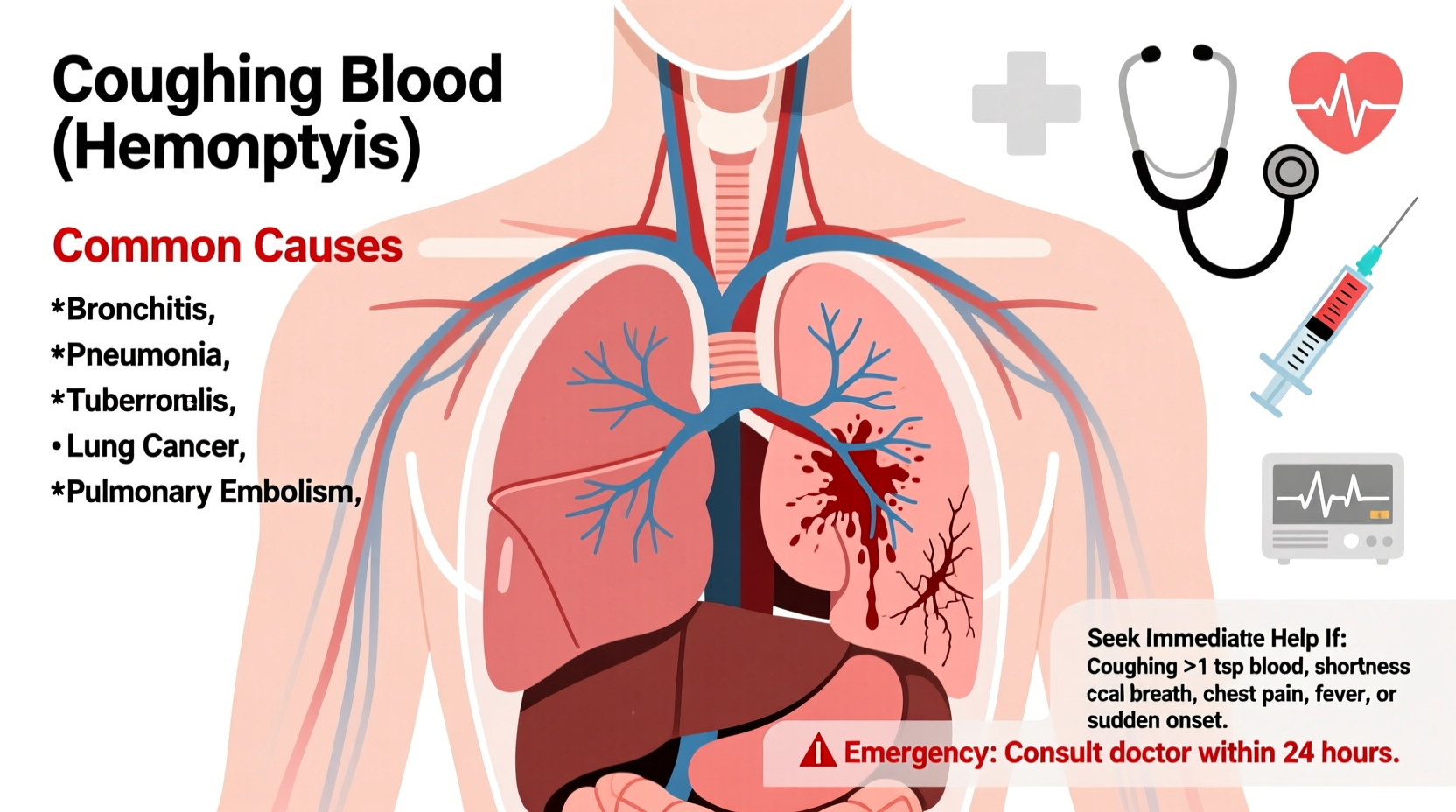
Common Causes of Hemoptysis
Several conditions can lead to coughing blood. Some are relatively benign and easily treatable, while others require urgent intervention. Below are the most frequent causes grouped by severity and origin.
1. Respiratory Infections
Infections are among the most common causes of mild hemoptysis. These include:
- Acute bronchitis: Inflammation of the bronchial tubes often leads to bloody mucus, especially after prolonged coughing.
- Pneumonia: Lung infection causing inflamed air sacs that may bleed slightly.
- Tuberculosis (TB): A serious bacterial infection prevalent in certain regions; hemoptysis is a hallmark symptom in advanced cases.
2. Chronic Lung Diseases
Long-term respiratory conditions increase the risk of blood in sputum:
- Chronic obstructive pulmonary disease (COPD): Frequent coughing and damaged airways can lead to minor bleeding.
- Bronchiectasis: Abnormal widening of the bronchial tubes results in mucus buildup and recurrent infections, often associated with intermittent hemoptysis.
3. Pulmonary Embolism
A blood clot in the lungs (pulmonary embolism) can cause sudden shortness of breath, chest pain, and sometimes coughing up small amounts of blood. This is a medical emergency requiring immediate treatment.
4. Lung Cancer
In smokers or former smokers over 40, persistent cough with blood-tinged sputum may indicate lung cancer. While not always present early on, hemoptysis becomes more common as tumors grow and invade blood vessels.
5. Trauma or Foreign Body
Physical injury to the chest or inhaling a foreign object can damage airway linings and result in bleeding. This is more common in children or individuals with altered consciousness.
6. Autoimmune and Vascular Conditions
Rarer systemic diseases such as granulomatosis with polyangiitis (GPA) or Goodpasture syndrome affect small blood vessels in the lungs and kidneys, leading to recurrent or severe hemoptysis.
“Any episode of hemoptysis warrants investigation. Even if it resolves quickly, identifying the source early improves prognosis, especially in cases like lung cancer or tuberculosis.” — Dr. Alan Reyes, Pulmonologist, Massachusetts General Hospital
When to Seek Immediate Medical Help
Not all cases of coughing blood require an ER visit, but knowing when to act fast is crucial. The volume and frequency of bleeding, along with accompanying symptoms, determine urgency.
| Symptom Severity | Signs to Watch For | Action Required |
|---|---|---|
| Mild | Small streaks of blood in mucus, one-time occurrence, no other symptoms | Schedule doctor visit within 24–48 hours |
| Moderate | Blood volume less than a teaspoon, recurring over days, plus fatigue or low-grade fever | See physician promptly; possible imaging needed |
| Severe | More than a few teaspoons of blood, repeated episodes, dizziness, chest pain, difficulty breathing | Call emergency services or go to ER immediately |
Diagnostic Process and Medical Evaluation
If you present with hemoptysis, doctors will work quickly to identify the source. The evaluation typically follows this sequence:
- Medical history review: Smoking status, travel history, exposure to TB, existing lung conditions, recent trauma, or use of blood thinners.
- Physical examination: Listening to lung sounds, checking oxygen levels, and assessing vital signs.
- Imaging: A chest X-ray is usually first; if inconclusive, a CT scan provides detailed views of the lungs and airways.
- Lab tests: Sputum culture, complete blood count, coagulation profile, and possibly autoimmune markers.
- Specialized procedures: Bronchoscopy allows direct visualization of the airways and can both diagnose and treat bleeding sources.
Mini Case Study: Recognizing Early Signs
John, a 58-year-old construction worker and former smoker, noticed pink-tinged phlegm for three mornings. He initially dismissed it as a lingering cold. When the streaks persisted and he developed fatigue and night sweats, he visited his primary care doctor. A chest X-ray revealed a mass in his right lung. Further testing confirmed non-small cell lung cancer at an early stage. Thanks to timely intervention, he underwent surgery and remains cancer-free two years later. His case underscores how even minimal hemoptysis can be a warning sign worth investigating.
Do’s and Don’ts When Coughing Blood
| Do’s | Don’ts |
|---|---|
| Measure and record the amount and color of blood | Ignore repeated episodes, even if small |
| Stop smoking immediately | Use over-the-counter cough suppressants without consulting a doctor |
| Stay calm and sit upright if bleeding occurs | Assume it’s just from throat irritation without evaluation |
| Seek care if you have risk factors like COPD or smoking history | Delay imaging or specialist referral if symptoms persist |
FAQ
Is coughing a little blood always dangerous?
Not always. Small streaks after intense coughing due to bronchitis or sinus drainage can be harmless. However, any recurrence or progression should be evaluated by a healthcare provider to rule out serious conditions.
Can medications cause you to cough up blood?
Yes. Blood thinners like warfarin, apixaban, or aspirin can increase bleeding risk, including in the respiratory tract. They don’t cause hemoptysis directly but may worsen bleeding from an existing condition.
How is massive hemoptysis treated?
Massive hemoptysis (over 100–600 mL in 24 hours) is managed in intensive care. Treatments include bronchoscopic interventions, embolization (blocking the bleeding vessel), or surgery if necessary. Securing the airway is the top priority.
Preventive Steps and Long-Term Care
While not all causes of hemoptysis are preventable, certain lifestyle choices reduce risk:
- Quit smoking: The single most effective step to protect lung health and lower risks of cancer, COPD, and infections.
- Manage chronic lung diseases: Follow treatment plans for asthma, COPD, or bronchiectasis to minimize flare-ups.
- Get vaccinated: Flu and pneumococcal vaccines help prevent infections that could trigger bleeding.
- Avoid environmental irritants: Limit exposure to dust, pollution, and chemical fumes that inflame airways.
Conclusion: Take Action Before It’s Too Late
Coughing blood is a symptom that demands attention—not panic, but purposeful action. Whether it's a fleeting trace after a bad cold or a recurring issue, understanding the possible causes empowers you to make informed decisions. Early diagnosis can turn a potentially fatal condition into a manageable one. If you or someone you know experiences this symptom, don’t wait for it to worsen. Consult a healthcare professional, advocate for proper testing, and prioritize lung health. Your body is sending a message—listen to it.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?