A cough that lingers beyond a few weeks is more than just an annoyance—it can be a signal from your body that something requires attention. While most short-term coughs resolve within two to three weeks, a cough lasting three months or longer enters the category of chronic cough. This duration warrants evaluation, especially if symptoms worsen or are accompanied by other concerning signs. Understanding when to worry, what underlying conditions may be at play, and how to respond can make a significant difference in outcomes.
When a Cough Crosses the Line
A cough lasting up to three weeks is often linked to common respiratory infections like colds or flu. However, once it persists past eight weeks in adults (or four weeks in children), it’s classified as chronic. At the three-month mark, the cause is unlikely to be a simple viral infection. Instead, it points toward an ongoing condition that needs proper diagnosis.
Chronic cough isn’t a disease itself but a symptom of an underlying issue. The body uses coughing to clear irritants or mucus from the airways. When this reflex continues without resolution, it suggests irritation or inflammation that hasn’t been addressed—or a more serious pathology developing beneath the surface.
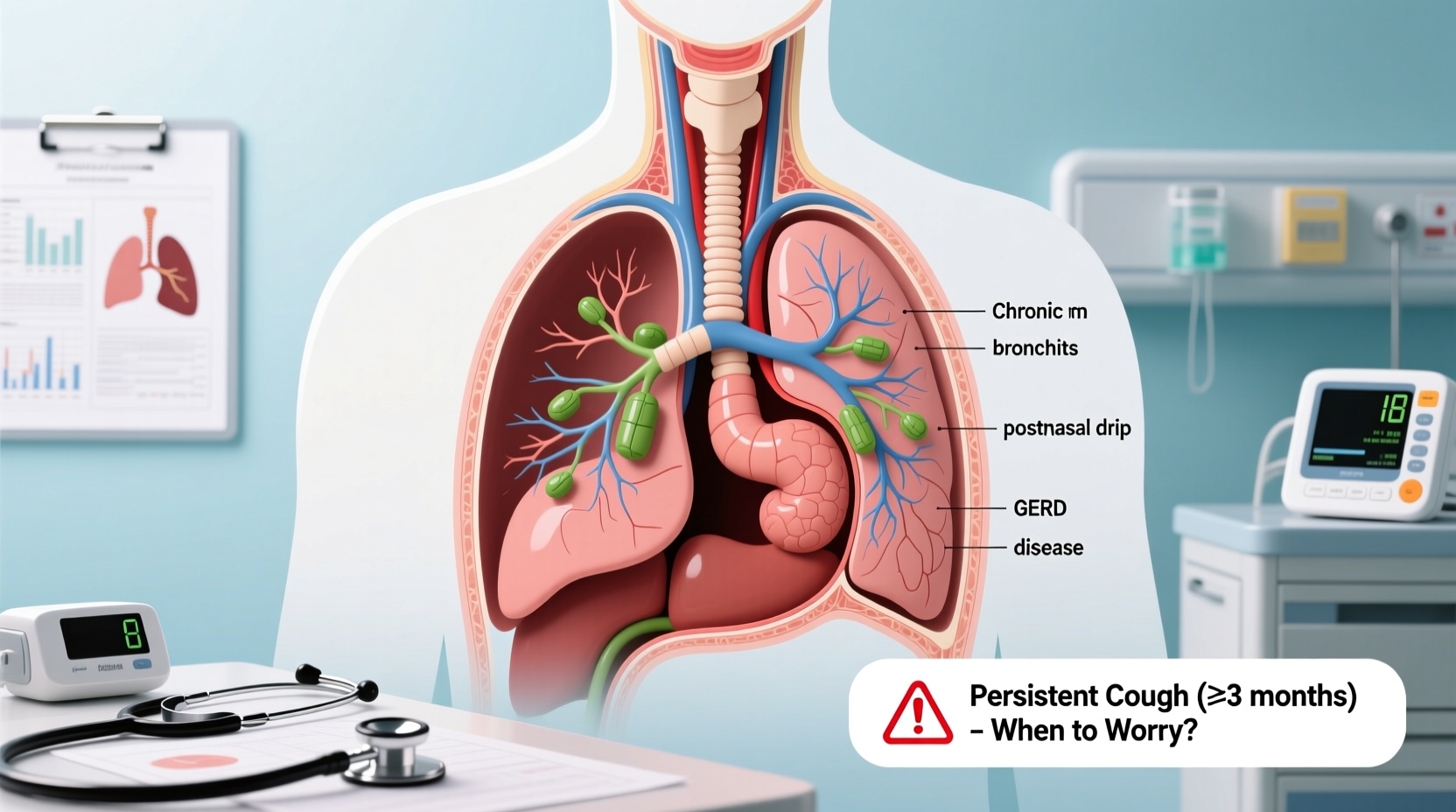
Possible Causes of a Three-Month Cough
The list of potential causes for a prolonged cough is extensive, ranging from manageable lifestyle factors to serious medical conditions. Below are the most common and clinically relevant explanations.
Postnasal Drip
One of the leading causes of chronic cough, postnasal drip occurs when excess mucus from the sinuses drains down the back of the throat, triggering irritation and cough reflexes. It’s often associated with allergies, sinusitis, or environmental irritants like dust or smoke.
Asthma and Cough-Variant Asthma
Asthma doesn’t always present with wheezing. In some cases, especially in adults, the only symptom is a dry, persistent cough—often worse at night or after physical activity. This form is known as cough-variant asthma and responds well to asthma medications once diagnosed.
Gastroesophageal Reflux Disease (GERD)
GERD affects millions and frequently goes undiagnosed. Stomach acid refluxes into the esophagus and sometimes reaches the throat, irritating the airways and causing a chronic cough, especially when lying down. Many people don’t experience heartburn, making GERD a hidden culprit.
Chronic Bronchitis
Common in smokers or those exposed to lung irritants, chronic bronchitis involves long-term inflammation of the bronchial tubes. It’s defined by a productive cough (with mucus) on most days for at least three months over two consecutive years. It falls under the umbrella of chronic obstructive pulmonary disease (COPD).
Medication Side Effects
Certain blood pressure medications, particularly ACE inhibitors (like lisinopril or enalapril), can cause a persistent dry cough in up to 20% of users. If the cough began shortly after starting such medication, this could be the source—even if you’ve taken it for months without issues.
Infections
Some infections leave behind lingering effects. Pertussis (whooping cough), tuberculosis, or fungal lung infections can cause prolonged coughing. In regions where TB is prevalent, a three-month cough should prompt screening.
Lung Conditions and Cancer
While less common, a persistent cough can be an early sign of lung cancer, especially in current or former smokers over age 50. Other red flags include coughing up blood, unexplained weight loss, or chest pain.
“Any cough lasting more than eight weeks deserves investigation. Dismissing it as ‘just a smoker’s cough’ can delay diagnosis of treatable or serious conditions.” — Dr. Lena Patel, Pulmonologist, Cleveland Clinic
Warning Signs That Demand Immediate Attention
Not every chronic cough signals danger, but certain symptoms should never be ignored. These are indicators that prompt medical evaluation is essential.
| Symptom | Possible Implication | Action Required |
|---|---|---|
| Coughing up blood (even small streaks) | Bronchitis, infection, or lung cancer | Seek care within 24–48 hours |
| Unintentional weight loss | Chronic infection, malignancy, or systemic illness | Medical evaluation needed |
| Shortness of breath or wheezing | Asthma, COPD, or heart/lung disease | See a doctor promptly |
| Fever lasting more than 10 days | Ongoing infection (bacterial, TB, fungal) | Requires diagnostic testing |
| Chest pain when breathing or coughing | Pleurisy, pneumonia, or pulmonary embolism | Urgent assessment recommended |
Step-by-Step: What to Do If You’ve Been Coughing for 3 Months
If your cough has persisted for three months, follow this structured approach to get answers and relief.
- Document Your Symptoms: Record frequency, timing, triggers (e.g., food, smoke, lying down), and whether the cough is dry or productive.
- Review Medications: Check if you’re on an ACE inhibitor. Discuss alternatives with your doctor if suspected.
- Assess Lifestyle Factors: Consider smoking history, exposure to allergens, or occupational hazards (dust, chemicals).
- See Your Primary Care Physician: They can perform initial tests like chest X-rays, spirometry (lung function), or refer you to a specialist.
- Follow Up with Specialists if Needed: A pulmonologist, ENT, or gastroenterologist may be necessary depending on findings.
Real-Life Example: Recognizing a Hidden Cause
Mark, a 44-year-old office worker, had been coughing for nearly four months. He assumed it was due to seasonal allergies and used over-the-counter antihistamines with little improvement. His cough worsened at night and after meals, but he had no heartburn. After his primary care doctor ordered a pH impedance test, Mark was diagnosed with silent reflux—GERD without typical symptoms. With dietary changes and proton-pump inhibitors, his cough resolved within six weeks. This case highlights how non-respiratory conditions can manifest primarily through coughing.
Checklist: Questions to Ask Your Doctor
- Could my medications be causing this cough?
- Do I need a chest X-ray or lung function test?
- Should I be evaluated for asthma or GERD?
- Is there any sign of infection, including tuberculosis?
- Could this be related to allergies or postnasal drip?
- What lifestyle changes might help reduce my symptoms?
Frequently Asked Questions
Can a chronic cough go away on its own?
It’s unlikely after three months without identifying and treating the root cause. While symptoms may fluctuate, true resolution usually requires intervention—whether it’s stopping a medication, managing asthma, or treating reflux.
I’m not a smoker—can I still have a serious lung condition?
Absolutely. Non-smokers can develop asthma, GERD-related cough, infections, or even lung cancer. Environmental exposures, genetics, and autoimmune conditions also play roles.
How long will it take to diagnose the cause?
Most patients receive a preliminary diagnosis within 1–3 visits. However, complex cases involving rare infections or interstitial lung diseases may require weeks of testing and specialist input.
Conclusion: Don’t Wait Until It Gets Worse
A cough lasting three months is not normal, regardless of how mild it seems. It’s your body’s way of signaling that something is off. Whether it’s a manageable condition like postnasal drip or a more serious issue like undiagnosed asthma or lung disease, early action leads to better outcomes. Ignoring the symptom risks prolonged discomfort, reduced quality of life, and potentially missed opportunities for effective treatment.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?