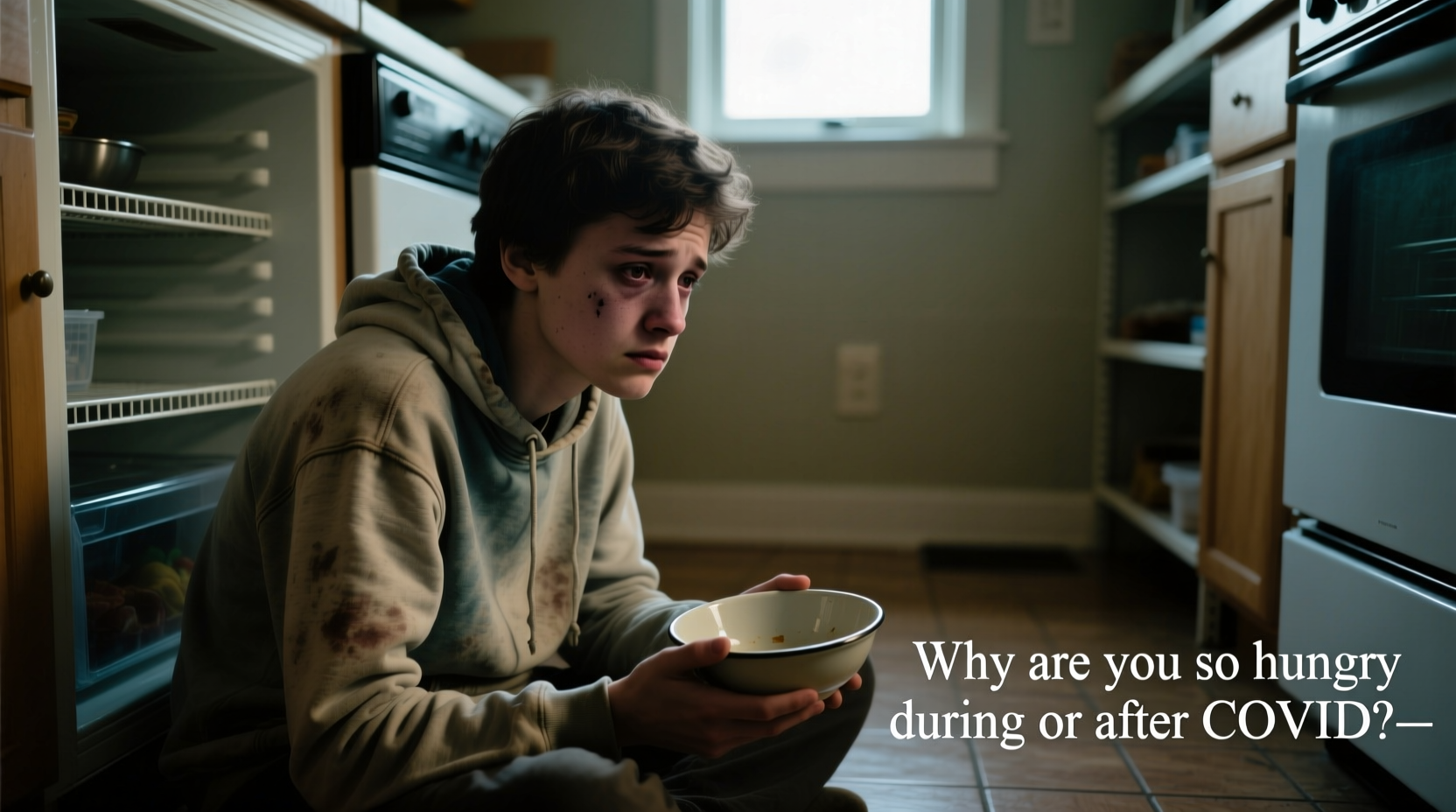
Many people recovering from a SARS-CoV-2 infection report a surprising symptom: an unusually strong appetite. While fatigue, brain fog, and respiratory issues dominate discussions about long COVID, intense hunger is emerging as a lesser-known but widespread experience. This sudden or persistent increase in appetite can be confusing—especially when it follows a period of illness that may have included loss of taste, appetite suppression, or even nausea. So why does this happen? The answer lies at the intersection of immune response, metabolic shifts, and neurological regulation.
Understanding the biological mechanisms behind post-COVID hunger not only demystifies the experience but also empowers individuals to respond with informed dietary and lifestyle choices. Whether you're weeks or months into recovery, recognizing the root causes can help prevent unwanted weight gain, support healing, and restore balance to your body’s signals.
The Body’s Recovery Mode and Energy Demands
After fighting off a viral infection like COVID-19, the body enters a phase of repair. Immune activity during infection increases energy expenditure significantly—even more than typical daily activities. Inflammation, fever, and cellular regeneration all require calories. Once the acute phase passes, the body may signal increased hunger to replenish depleted energy stores and support tissue healing.
This isn’t unique to COVID-19; other infections can trigger similar responses. However, the scale and duration of immune activation seen in some cases of SARS-CoV-2 infection appear to amplify this effect. Studies suggest that prolonged inflammatory markers, such as elevated C-reactive protein (CRP), can persist post-infection, keeping metabolism elevated and increasing caloric needs.
Hormonal Imbalances Linked to Appetite Regulation
The hormones that regulate hunger—leptin and ghrelin—are often disrupted during and after illness. Leptin, produced by fat cells, signals fullness to the brain. Ghrelin, known as the \"hunger hormone,\" stimulates appetite. Research has shown that viral infections, including COVID-19, can interfere with the normal secretion of these hormones.
A 2022 study published in Obesity found that patients recovering from moderate to severe COVID-19 exhibited lower leptin levels and higher ghrelin concentrations compared to controls, even weeks after symptom resolution. This hormonal imbalance creates a physiological drive to eat more, regardless of actual energy needs.
In addition, cortisol—the stress hormone—often remains elevated during recovery. Chronic stress from illness, isolation, or anxiety about health can further dysregulate appetite circuits in the hypothalamus, leading to cravings, especially for high-sugar or high-fat comfort foods.
“Post-viral appetite changes are more common than we realize. The body is trying to heal, and sometimes its signals get misinterpreted or amplified.” — Dr. Lena Patel, Endocrinologist and Metabolism Specialist
Metabolic Changes and Insulin Sensitivity
Emerging evidence suggests that SARS-CoV-2 can affect pancreatic beta cells and insulin signaling, potentially altering glucose metabolism. Some patients develop temporary or even persistent insulin resistance after infection, which may contribute to increased hunger.
When cells become less responsive to insulin, glucose remains in the bloodstream instead of being absorbed for energy. The brain interprets this as a lack of fuel, triggering hunger signals despite adequate calorie intake. This cycle can lead to overeating, particularly carbohydrates, in an attempt to satisfy perceived energy deficits.
This phenomenon may explain why some individuals feel ravenous shortly after eating, especially if their meals are high in refined sugars or simple carbs. Balancing macronutrients becomes crucial in stabilizing blood sugar and reducing false hunger cues.
Do’s and Don’ts for Managing Post-COVID Hunger
| Do’s | Don’ts |
|---|---|
| Eat balanced meals with protein, fiber, and healthy fats | Skip meals or rely on sugary snacks |
| Stay hydrated—thirst is often mistaken for hunger | Ignore portion sizes due to increased appetite |
| Monitor blood sugar if you have risk factors for diabetes | Assume the hunger will resolve on its own without intervention |
| Engage in light physical activity to regulate appetite | Restrict calories severely, which can worsen metabolic recovery |
Neurological Impact and Taste Recovery
Loss of smell and taste (anosmia and ageusia) was one of the hallmark symptoms of early-stage COVID-19. As these senses return—sometimes gradually or with distortions like phantosmia (smelling odors that aren’t there)—the brain re-engages with food in new ways. For many, the restored ability to enjoy flavors leads to a psychological rebound in eating behavior.
This “taste reawakening” can create a heightened interest in food, almost like rediscovering pleasure in eating. Combined with physical recovery needs, this sensory resurgence may amplify the desire to eat frequently or in larger quantities. It’s not just biological—it’s also emotional and experiential.
In some cases, people who lost weight during acute illness may subconsciously strive to regain it, interpreting hunger as a sign of returning health. While regaining strength is important, unchecked eating can lead to rapid weight gain, especially if activity levels remain low during convalescence.
Mini Case Study: Sarah’s Experience with Post-COVID Hunger
Sarah, a 42-year-old teacher, contracted COVID-19 in early 2023. During her two-week illness, she lost 7 pounds due to fever, poor appetite, and altered taste. Three weeks after testing negative, she noticed an overwhelming urge to eat—particularly sweets and starchy foods. Despite consuming more than usual, she still felt unsatisfied after meals.
Her primary care provider ordered blood work, which revealed mildly elevated fasting insulin and low leptin levels. With guidance, Sarah adjusted her diet to include more protein at breakfast, added leafy greens and legumes, and began walking 20 minutes daily. Within six weeks, her hunger normalized, and she regained energy without excessive weight gain.
Sarah’s case illustrates how multiple factors—metabolic disruption, hormonal imbalance, and sensory recovery—can converge to create persistent hunger after infection.
Step-by-Step Guide to Regulating Post-COVID Appetite
- Track your intake and symptoms: Keep a journal of meals, hunger levels, and energy for at least one week to identify patterns.
- Prioritize protein and fiber: Include lean meats, eggs, beans, oats, and vegetables in every meal to increase satiety.
- Space meals evenly: Eat every 3–4 hours to stabilize blood sugar and reduce hunger spikes.
- Stay hydrated: Drink water throughout the day; dehydration mimics hunger.
- Get tested if needed: Ask your doctor to check thyroid function, fasting glucose, insulin, and inflammatory markers.
- Manage stress: Practice mindfulness, breathing exercises, or gentle yoga to lower cortisol.
- Gradually resume activity: Light exercise helps regulate appetite hormones and improve insulin sensitivity.
Frequently Asked Questions
Is it normal to feel extremely hungry after having COVID?
Yes, it is increasingly recognized as a common post-viral symptom. Your body may be compensating for energy used during illness, repairing tissues, or adjusting hormone levels. If hunger persists beyond 6–8 weeks or leads to rapid weight gain, consult a healthcare provider.
Can long COVID cause ongoing appetite changes?
Yes. Long COVID can disrupt autonomic nervous system function, including digestion and appetite control. Some patients report fluctuating hunger, early satiety, or cravings as part of broader metabolic dysregulation. Multidisciplinary care may be needed for persistent symptoms.
Should I be worried about developing diabetes after COVID?
While most people won’t develop diabetes, research shows an increased risk of new-onset type 2 diabetes following SARS-CoV-2 infection, especially in those with pre-existing risk factors. Monitoring blood sugar and maintaining a healthy lifestyle can mitigate this risk.
Checklist: Managing Hunger After COVID-19
- ✅ Eat balanced meals with protein, complex carbs, and healthy fats
- ✅ Drink at least 8 glasses of water daily
- ✅ Avoid skipping meals to prevent overeating later
- ✅ Monitor portion sizes, even with healthy foods
- ✅ Incorporate movement, even light walking
- ✅ Track symptoms and discuss them with your doctor
- ✅ Limit ultra-processed foods and added sugars
Conclusion
Increased hunger during or after a bout of COVID-19 is not merely psychological—it reflects real physiological changes in metabolism, hormones, and neural signaling. Recognizing this helps shift the narrative from guilt or confusion to understanding and action. By supporting your body with nutritious food, mindful habits, and appropriate medical follow-up, you can navigate this phase of recovery with greater confidence.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?