Abdominal cramping without a menstrual period can be confusing and concerning. While it's easy to assume pregnancy is the only explanation, several other factors—ranging from hormonal imbalances to digestive issues—can cause similar sensations. Understanding the potential reasons behind this experience helps reduce anxiety and guides timely medical decisions. This article explores the most common causes of cramping in the absence of menstruation, offering practical insights for women navigating this symptom.
Hormonal Fluctuations and Cycle Variability
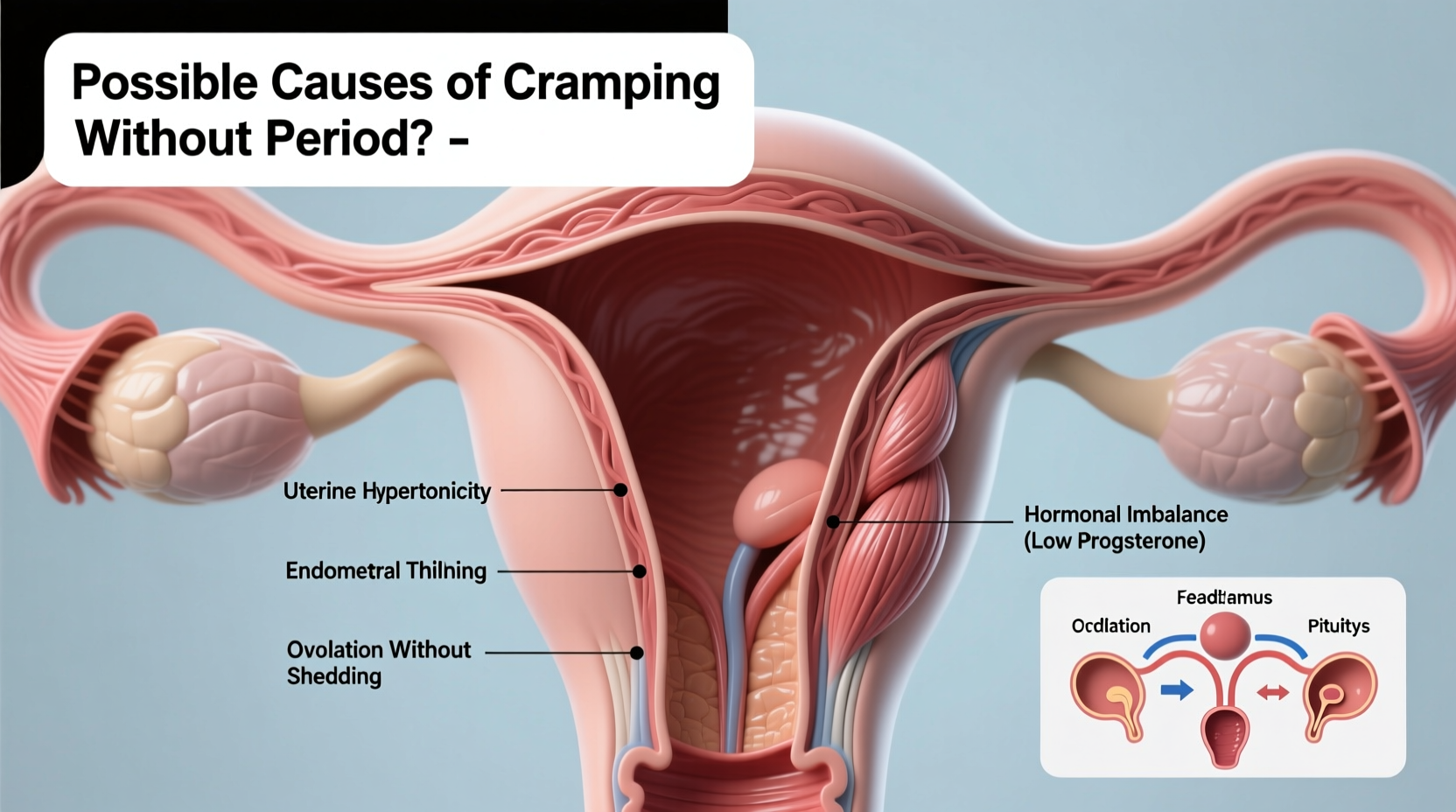
The menstrual cycle is regulated by a delicate balance of hormones, primarily estrogen and progesterone. Even minor disruptions can delay ovulation or menstruation while still triggering cramp-like symptoms. For example, late ovulation may shift the entire cycle, leading to mid-cycle or premenstrual-type cramps despite the absence of bleeding.
Stress, significant weight changes, intense exercise, or travel can all interfere with the hypothalamus—the brain region that signals hormone production. When this happens, the body might prepare the uterine lining for shedding (causing cramping) but fail to initiate the final hormonal cascade needed for menstruation.
Pregnancy and Early Implantation
One of the most common reasons for cramping without a period is early pregnancy. Around 6–12 days after fertilization, the embryo implants into the uterine lining—a process known as implantation. Some women experience mild cramping during this phase, often mistaken for an impending period.
In addition to cramps, early signs of pregnancy may include:
- Light spotting (implantation bleeding)
- Breast tenderness
- Fatigue
- Nausea
- Increased urination
It’s important to note that not all pregnancies produce obvious symptoms early on. A missed period combined with persistent cramping warrants a pregnancy test—even if initial results are negative, especially if testing was done too soon.
“Many patients come in convinced they aren’t pregnant because their test was negative, only to find out weeks later they tested too early. Timing matters.” — Dr. Lena Patel, OB-GYN Specialist
Medical Conditions That Mimic Menstrual Cramping
Several gynecological and non-gynecological conditions can cause pelvic discomfort resembling menstrual cramps. These should be considered when periods are absent or irregular.
Polycystic Ovary Syndrome (PCOS)
PCOS affects up to 10% of women of reproductive age and disrupts normal ovulation. Women with PCOS often experience infrequent or absent periods, along with symptoms like acne, weight gain, and excess hair growth. Despite not ovulating regularly, some still feel ovarian pain or pelvic pressure due to cyst development.
Endometriosis
This condition occurs when tissue similar to the uterine lining grows outside the uterus, commonly on the ovaries, fallopian tubes, or bowel. Endometriosis can cause chronic pelvic pain, painful intercourse, and cramping at various points in the cycle—even when no period is present.
Pelvic Inflammatory Disease (PID)
Often caused by untreated sexually transmitted infections like chlamydia or gonorrhea, PID leads to inflammation of the reproductive organs. Symptoms include lower abdominal pain, fever, unusual discharge, and irregular bleeding—or no bleeding at all.
Ovarian Cysts
Functional cysts form naturally during the menstrual cycle and usually resolve on their own. However, larger cysts can rupture or twist, causing sharp or dull cramping on one side of the pelvis. These episodes may occur independently of menstruation.
| Condition | Key Symptoms | When to Seek Help |
|---|---|---|
| PCOS | Irregular cycles, acne, insulin resistance | After three missed periods |
| Endometriosis | Cyclic pelvic pain, painful periods, infertility | If pain interferes with daily life |
| PID | Fever, foul discharge, pain during sex | Immediately—requires antibiotics |
| Ovarian Cysts | One-sided pain, bloating, nausea | If sudden severe pain or vomiting |
Digestive and Urinary System Causes
Not all lower abdominal pain originates from the reproductive system. The proximity of the intestines, bladder, and uterus means discomfort from gastrointestinal or urinary issues can easily be mistaken for menstrual cramps.
Irritable Bowel Syndrome (IBS): IBS often flares cyclically and can cause cramping, bloating, gas, and changes in bowel habits. Hormonal shifts during the menstrual cycle can exacerbate IBS symptoms, making them appear linked to menstruation even when no period occurs.
Urinary Tract Infections (UTIs): UTIs cause pelvic pressure, burning during urination, and frequent urges to go. Lower abdominal discomfort may resemble cramping, especially in early stages before classic symptoms emerge.
Constipation: Stool buildup in the colon can create pressure and dull aching in the lower abdomen, mimicking menstrual pain. This is particularly common in individuals with low fiber intake or irregular bowel movements.
Stress, Lifestyle, and Weight-Related Factors
Chronic stress activates the body’s fight-or-flight response, suppressing reproductive function through cortisol release. Over time, this can halt ovulation and delay menstruation. Yet, the uterus may still contract mildly due to residual hormonal activity or muscle tension, producing cramp-like feelings.
Similarly, extreme weight loss, eating disorders, or excessive exercise can lead to functional hypothalamic amenorrhea—where periods stop due to insufficient energy availability. Athletes, dancers, and those with restrictive diets are particularly vulnerable.
On the other end of the spectrum, obesity increases estrogen production from fat tissue, which can disrupt normal cycling and lead to irregular or absent periods with intermittent pelvic discomfort.
Mini Case Study: Sarah’s Experience
Sarah, a 28-year-old graduate student, began experiencing monthly cramps but hadn’t had a period in four months. She wasn’t sexually active, so pregnancy was ruled out. After blood tests and an ultrasound, her doctor diagnosed her with stress-induced amenorrhea. High academic pressure and poor sleep had disrupted her hormonal axis. With lifestyle adjustments—including mindfulness practices and improved nutrition—her cycle returned within two months, and the cramping subsided.
Action Plan: What to Do If You’re Cramping Without a Period
Follow this step-by-step approach to assess your situation and determine next steps:
- Take a pregnancy test – Use a first-morning urine sample for accuracy, especially if your period is more than five days late.
- Review recent lifestyle changes – Consider stress levels, diet, exercise intensity, and sleep quality.
- Track symptoms for 5–7 days – Note pain location, duration, associated symptoms (e.g., nausea, fever), and whether bleeding starts.
- Evaluate over-the-counter relief – NSAIDs like ibuprofen may ease cramping but won’t address underlying causes.
- Schedule a medical consultation – Especially if cramping persists beyond a week, worsens, or is accompanied by fever, vomiting, or dizziness.
Checklist: When to See a Doctor
- ✅ Missed period for more than six weeks
- ✅ Severe or worsening pelvic pain
- ✅ Fever, chills, or unusual vaginal discharge
- ✅ Pain during urination or bowel movements
- ✅ History of PCOS, endometriosis, or infertility
- ✅ Positive or inconclusive pregnancy test
Frequently Asked Questions
Can you have cramps and not be pregnant?
Yes. Cramping without a period is common and can result from hormonal imbalances, stress, digestive issues, or gynecological conditions like PCOS or ovarian cysts. Pregnancy is just one of many possibilities.
How soon can I test for pregnancy after cramping starts?
Wait until at least the first day of your missed period for the most accurate result. Testing too early may yield a false negative, especially if implantation occurred late.
Are occasional missed periods normal?
Occasional irregularities (one or two per year) are common and often tied to temporary stress or illness. However, consistently missing periods requires evaluation to rule out hormonal or structural issues.
Conclusion: Listen to Your Body and Take Action
Cramping without a period is more than just a puzzling symptom—it’s a signal from your body that something may be off-balance. Whether it’s stress, a hormonal shift, or an underlying condition, ignoring persistent discomfort can delay diagnosis and treatment. By tracking your cycle, recognizing patterns, and seeking professional guidance when needed, you empower yourself to maintain long-term reproductive health.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?