Waking up with a pounding headache every single day is more than just frustrating—it can be debilitating. Migraines that occur daily disrupt work, relationships, and quality of life. While occasional migraines are common, chronic daily headaches often signal an underlying issue that requires attention. Understanding why you’re experiencing these relentless attacks—and what actionable steps you can take—is the first step toward relief.
Understanding Chronic Daily Migraines
Chronic migraine is defined as having headaches on 15 or more days per month for at least three months, with at least eight of those days featuring migraine-specific symptoms such as nausea, light sensitivity, or throbbing pain. When this becomes a daily experience, it’s often referred to as \"chronic daily migraine,\" though the term encompasses several subtypes including chronic migraine, medication-overuse headache, and new daily persistent headache (NDPH).
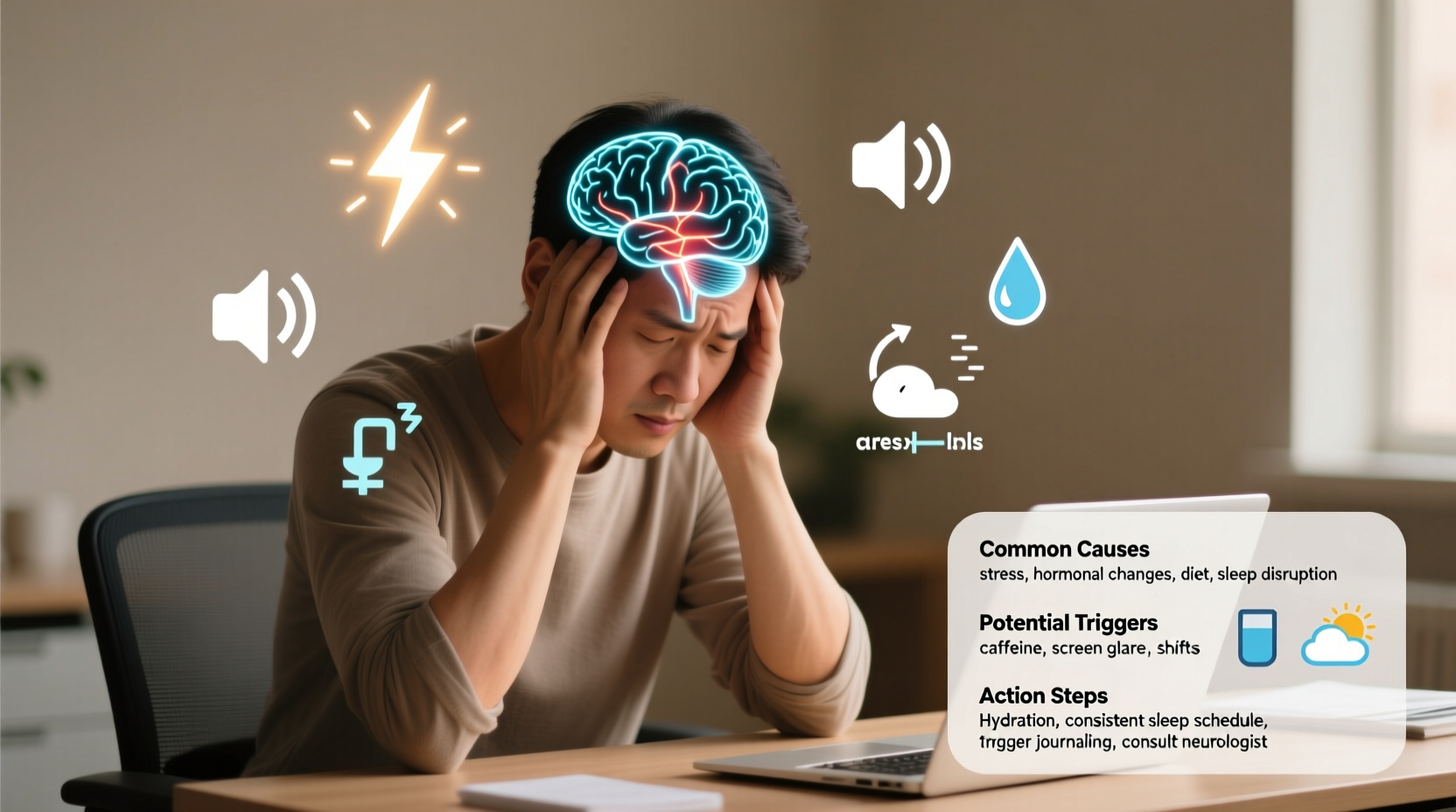
The shift from episodic to daily migraines typically happens gradually. It may begin with increased frequency due to stress, hormonal changes, or poor sleep, eventually leading the nervous system into a state of constant hyperexcitability. This means your brain becomes primed to trigger pain responses more easily—even in response to normally harmless stimuli like bright lights or mild stress.
Common Causes of Daily Migraines
There is rarely one single cause behind daily migraines. Instead, they usually result from a combination of biological, environmental, and behavioral factors. Identifying potential triggers is essential to managing and reducing their frequency.
- Hormonal fluctuations: Especially in women, estrogen shifts during menstruation, pregnancy, or menopause can provoke migraines.
- Medication overuse: Frequent use of pain relievers (like ibuprofen, acetaminophen, or triptans) more than two or three times a week can lead to rebound headaches.
- Sleep disturbances: Both insufficient sleep and oversleeping can trigger migraines. Irregular sleep schedules are particularly problematic.
- Dietary triggers: Common culprits include aged cheeses, processed meats, alcohol (especially red wine), caffeine, and artificial sweeteners like aspartame.
- Stress and anxiety: Chronic psychological stress keeps the nervous system on high alert, lowering the threshold for migraine attacks.
- Environmental factors: Bright or flickering lights, strong odors, weather changes, and loud noises can all contribute.
- Dehydration and skipped meals: Going too long without water or food destabilizes blood sugar and electrolyte balance, both of which influence headache risk.
“Patients who develop daily migraines often have multiple overlapping triggers. The key isn’t elimination alone—it’s pattern recognition and systemic change.” — Dr. Lena Patel, Neurologist & Headache Specialist
What You Can Do: A Step-by-Step Approach
Managing daily migraines requires a structured plan. Jumping between remedies without consistency rarely works. Follow this timeline to identify root causes and implement sustainable solutions.
- Week 1–2: Begin tracking. Use a notebook or digital app to record headache intensity, duration, timing, possible triggers (food, sleep, mood), and medications used. Note any associated symptoms like nausea, vision changes, or neck stiffness.
- Week 3: Review patterns. Look for trends—do headaches follow poor sleep? Occur after certain foods? Align with your menstrual cycle? Share findings with your doctor.
- Week 4: Eliminate medication overuse. If you're using acute pain medication more than two days a week, consult your physician about tapering off safely. Abrupt cessation can worsen headaches initially but is often necessary.
- Month 2: Optimize lifestyle habits. Prioritize consistent sleep, hydration, regular meals, and stress-reduction techniques like mindfulness or gentle exercise.
- Month 3: Explore preventive treatments. Depending on severity, your doctor may recommend daily medications (such as beta-blockers, anticonvulsants, or CGRP inhibitors), Botox injections, or neuromodulation devices.
Do’s and Don’ts: Managing Daily Migraines
| Do’s | Don’ts |
|---|---|
| Maintain a consistent sleep schedule—even on weekends | Use OTC painkillers more than 2–3 times per week |
| Stay hydrated throughout the day (aim for ~2L of water) | Skimp on meals or fast for extended periods |
| Practice relaxation techniques like deep breathing or yoga | Ignore early warning signs (auras, neck stiffness, mood shifts) |
| Work with a neurologist to explore preventive therapies | Self-diagnose or delay medical consultation when headaches become daily |
| Limit caffeine to one moderate dose per day (e.g., small coffee) | Consume known dietary triggers regularly without tracking impact |
A Real-Life Example: Sarah’s Turnaround
Sarah, a 34-year-old teacher, began experiencing headaches four days a week. Over six months, they escalated to daily occurrences. She relied on ibuprofen almost every afternoon, which provided temporary relief but worsened her condition over time. After seeing a neurologist, she discovered she was suffering from medication-overuse headache compounded by poor sleep and high stress.
Her doctor helped her taper off NSAIDs and prescribed a low-dose preventive medication. Sarah started going to bed at 10:30 PM consistently, eliminated red wine and processed meats from her diet, and began practicing 10 minutes of guided meditation each morning. Within two months, her headache days dropped from 30 to 10 per month. By month five, she averaged only 3–4 mild headaches, none requiring medication.
When to See a Doctor
While occasional headaches are normal, daily migraines warrant professional evaluation. Seek immediate medical attention if you experience:
- Sudden, severe headache (\"thunderclap\" onset)
- Headache with fever, stiff neck, confusion, or seizures
- Weakness, numbness, or vision loss accompanying pain
- New headaches after age 50
For chronic daily headaches, a neurologist can help differentiate between primary headache disorders and secondary causes like hypertension, brain lesions, or autoimmune conditions. Diagnostic tools may include MRI or CT scans, blood tests, and detailed patient history analysis.
Frequently Asked Questions
Can dehydration really cause daily migraines?
Yes. Even mild dehydration affects cerebral blood flow and neurotransmitter activity, making the brain more susceptible to pain signals. Many people unknowingly exist in a state of low-grade dehydration, especially if they consume diuretics like coffee or alcohol regularly.
Is there a link between anxiety and daily migraines?
Definitely. Anxiety activates the sympathetic nervous system, increasing muscle tension, altering serotonin levels, and lowering pain thresholds. This creates a feedback loop where migraines increase anxiety, which in turn increases migraine frequency. Treating both conditions simultaneously often yields better outcomes.
Are there non-drug treatments that actually work?
Yes. Cognitive behavioral therapy (CBT), biofeedback, acupuncture, and neuromodulation devices (like Cefaly or gammaCore) have shown efficacy in clinical studies. Devices that deliver mild electrical stimulation to cranial nerves can reduce attack frequency by modulating pain pathways.
Take Control Starting Today
Daily migraines don’t have to be your new normal. While they can feel overwhelming, most people see meaningful improvement with the right approach. Start by gathering data through tracking, then systematically address lifestyle factors and medication use. Partner with a healthcare provider who specializes in headache disorders—this isn’t something you need to manage alone.
Relief begins with action. Whether it’s setting a bedtime alarm, eliminating a dietary trigger, or scheduling a doctor’s appointment, choose one step you can take today. Small decisions build momentum. Your journey back to fewer headaches—and a fuller life—starts now.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?