Experiencing pain during urination is never normal—and when it happens alongside dehydration, it can signal more than just a dry throat. While many assume that drinking less water only leads to thirst or fatigue, its impact on the urinary system is profound. Dehydration concentrates urine, irritates the bladder lining, and increases the risk of infections, all of which can make peeing not just uncomfortable but sharp or burning. Understanding the connection between low fluid intake and urinary pain is essential for both immediate relief and long-term urinary health.
The Science Behind Urine Concentration and Bladder Irritation
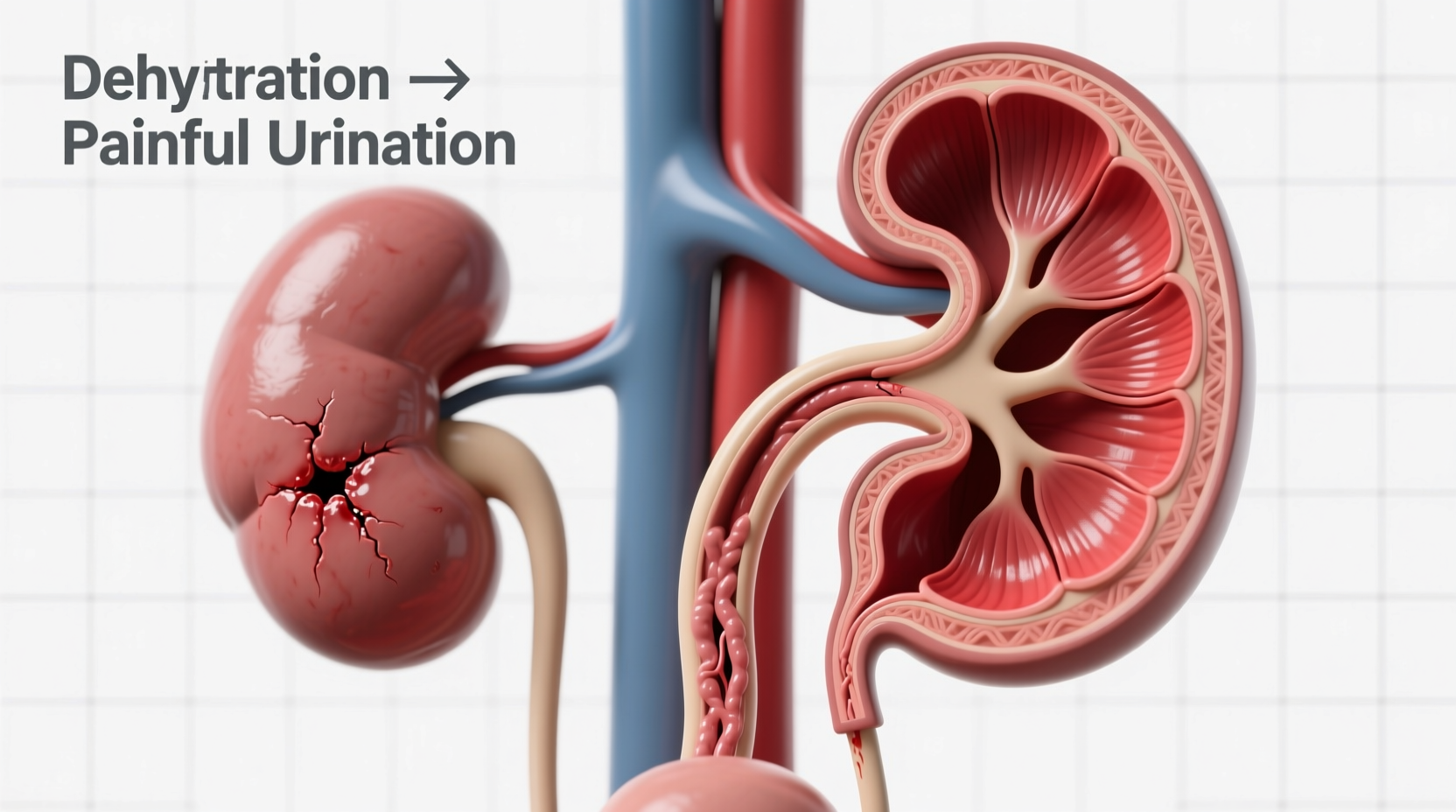
When your body lacks sufficient water, the kidneys work harder to conserve fluid. This results in less urine volume, but with a much higher concentration of waste products like urea, creatinine, and salts. Concentrated urine becomes darker in color—often amber or even brown—and more acidic. This acidity can inflame the delicate tissues of the urethra and bladder lining, causing stinging or burning sensations during urination.
Additionally, concentrated urine slows the natural flushing action of the urinary tract. Normally, regular urination helps wash away bacteria from the urethra. When urine output drops due to dehydration, bacteria have more time to multiply, increasing the risk of urinary tract infections (UTIs), which are a common cause of painful urination.
Dehydration and Its Role in UTIs
Urinary tract infections are one of the most frequent causes of painful urination. While bacteria—especially E. coli—are the direct culprits, dehydration creates the ideal environment for infection to take hold. Without adequate hydration, the body cannot flush out pathogens effectively. The stagnant, concentrated urine allows bacteria to adhere to the walls of the bladder and urethra, leading to inflammation and infection.
Women are particularly vulnerable due to their shorter urethras, but men and children can also develop dehydration-related UTIs. Symptoms include urgency, frequency, cloudy or foul-smelling urine, pelvic pressure, and, notably, a burning sensation when urinating.
“Chronic dehydration is a silent contributor to recurrent UTIs. I often see patients who don’t drink enough water throughout the day, then wonder why they keep getting infections.” — Dr. Lena Torres, Urologist at Pacific Health Institute
Other Contributing Factors That Amplify Discomfort
While dehydration plays a central role, several other factors can worsen urinary pain:
- Dietary irritants: Caffeine, alcohol, spicy foods, and artificial sweeteners can further irritate an already sensitive bladder.
- Holding urine too long: Delaying bathroom trips reduces flushing and increases bacterial growth.
- Poor hygiene: Wiping back to front (in women) introduces bacteria into the urethra.
- Medications: Some drugs, like antihistamines or decongestants, reduce urine output and contribute to retention.
In some cases, painful urination without infection may point to conditions like interstitial cystitis or urethral syndrome—both of which can be aggravated by concentrated urine.
Step-by-Step Guide to Relief and Recovery
If you're experiencing pain when peeing and suspect dehydration is the cause, follow this timeline to restore balance and ease symptoms:
- Day 1 – Immediate Rehydration: Begin sipping water every 15–20 minutes. Aim for at least 8–10 glasses (2–2.5 liters) over 24 hours. Avoid caffeine and alcohol.
- Day 1–2 – Monitor Symptoms: Track changes in urine color, odor, and pain level. Clear to light yellow urine indicates improvement.
- Day 2–3 – Supportive Care: Drink cranberry water (unsweetened), herbal teas like chamomile or marshmallow root, which may soothe the urinary tract.
- Day 3+ – Evaluate Need for Medical Help: If pain persists beyond 48 hours after rehydrating, or if fever, back pain, or nausea develops, seek medical evaluation for possible UTI or kidney involvement.
- Ongoing – Prevent Recurrence: Maintain consistent daily water intake, urinate regularly, and practice good hygiene.
Do’s and Don’ts: Managing Dehydration-Related Urinary Pain
| Do’s | Don’ts |
|---|---|
| Drink water consistently throughout the day | Wait until you’re thirsty to drink |
| Use a reusable water bottle as a reminder | Consume sugary drinks or energy beverages |
| Urinate as soon as you feel the urge | Hold urine for hours, especially during work |
| Wipe front to back after using the toilet | Use scented soaps or douches near the genital area |
| Include hydrating foods like cucumber, watermelon, and oranges | Ignore persistent burning or cloudy urine |
Real Example: How One Woman Resolved Recurrent Pain
Sarah, a 34-year-old project manager, began experiencing frequent stinging when she urinated during a particularly busy work quarter. She was drinking minimal water, relying on coffee to stay alert. After two weeks of worsening discomfort, she visited her primary care provider. Tests revealed no active infection, but her urine was highly concentrated. Her doctor emphasized that chronic dehydration had irritated her bladder lining.
Following a structured hydration plan—starting her day with 16 oz of water, carrying a marked bottle, and setting phone reminders—Sarah noticed improvement within 36 hours. By the end of the week, the pain was gone. She now prioritizes hydration as part of her wellness routine, preventing recurrence.
FAQ: Common Questions About Dehydration and Painful Urination
Can drinking more water cure a UTI?
While increased water intake alone won’t cure an established bacterial UTI, it supports recovery by helping flush out pathogens. Most UTIs require antibiotics prescribed by a healthcare provider. However, staying well-hydrated can sometimes prevent mild infections from progressing.
Why does my urine burn even after drinking water?
If pain persists despite rehydration, it could indicate an underlying infection, bladder inflammation, or sensitivity condition like interstitial cystitis. It may also be due to lingering irritation. If symptoms last more than two days after proper hydration, consult a doctor.
How much water should I drink to avoid urinary issues?
The general recommendation is 8–10 cups (about 2–2.5 liters) per day, but individual needs vary based on activity level, climate, and health status. A good rule: your urine should be pale yellow or clear. Dark urine means you need more fluids.
Conclusion: Take Control of Your Urinary Health
Painful urination isn’t something to ignore or push through. When linked to dehydration, it’s your body’s way of signaling imbalance—one that can often be corrected with simple, consistent habits. Hydration is more than just quenching thirst; it’s a foundational element of urinary and overall health. By understanding how fluid intake affects your bladder and taking proactive steps, you can prevent discomfort, reduce infection risk, and support long-term wellness.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?