Dizziness upon standing or while walking is a surprisingly common experience, especially among older adults. While often harmless and fleeting, it can sometimes signal an underlying health issue that requires attention. The sensation—ranging from lightheadedness to vertigo or unsteadiness—can disrupt daily activities and even increase the risk of falls. Understanding the root causes and knowing when to take action are essential for maintaining balance and overall well-being.
What Happens When You Feel Dizzy Upon Standing?
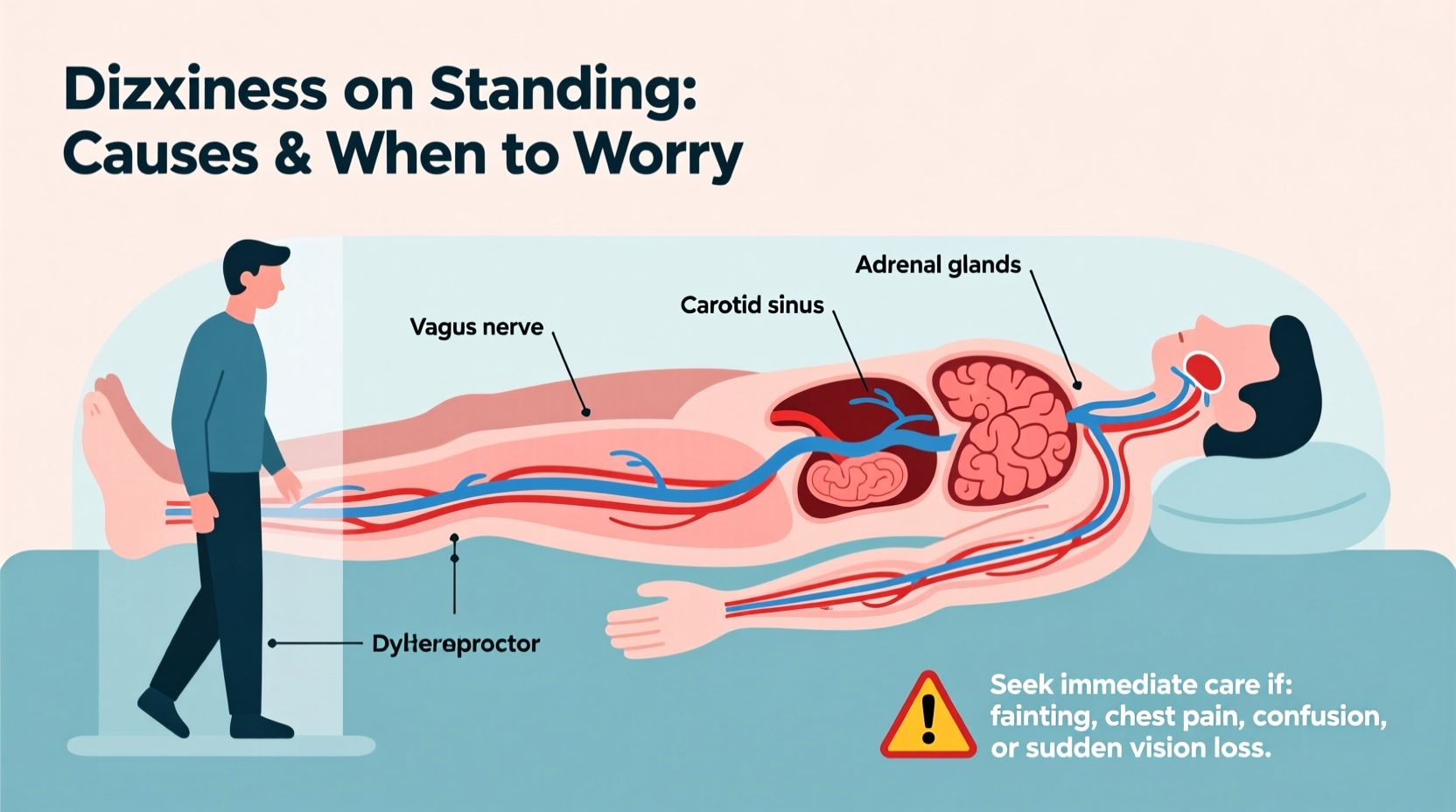
When you rise from a seated or lying position, gravity pulls blood downward into your legs and abdomen. Normally, your body compensates by increasing heart rate and constricting blood vessels to maintain steady blood flow to the brain. If this system falters, blood pressure drops suddenly—a condition known as orthostatic hypotension—leading to dizziness, blurred vision, or even fainting.
This temporary drop in cerebral perfusion usually resolves within seconds. However, if symptoms persist or worsen during walking, other neurological, cardiovascular, or metabolic factors may be involved.
Common Causes of Dizziness When Standing or Walking
Dizziness isn't a diagnosis but a symptom with multiple possible origins. Some causes are benign and easily managed; others require medical evaluation.
1. Orthostatic Hypotension
A sudden drop in blood pressure upon standing affects up to 30% of older adults. Risk increases with dehydration, prolonged bed rest, diabetes, Parkinson’s disease, or medications like diuretics and antidepressants.
2. Inner Ear Disorders
The vestibular system in the inner ear controls balance. Conditions such as benign paroxysmal positional vertigo (BPPV), Meniere’s disease, or vestibular neuritis can cause disorientation, spinning sensations, and imbalance—especially during movement.
3. Medication Side Effects
Many prescription drugs—including antihypertensives, sedatives, opioids, and certain antidepressants—can impair balance or lower blood pressure excessively. Polypharmacy (taking four or more medications) significantly raises the risk.
4. Dehydration and Low Blood Sugar
Inadequate fluid intake or skipping meals can lead to dizziness. Electrolyte imbalances from excessive sweating, vomiting, or diarrhea also contribute.
5. Neurological Conditions
Diseases like Parkinson’s, multiple sclerosis, or cerebellar ataxia affect coordination and gait. These often present with progressive imbalance, tremors, or difficulty initiating movement.
6. Cardiovascular Issues
Irregular heart rhythms (arrhythmias), heart valve problems, or reduced cardiac output may limit oxygen delivery to the brain, causing dizziness during exertion or ambulation.
“Transient dizziness after standing is common, but persistent imbalance during walking should never be dismissed as ‘just aging.’ It warrants investigation.” — Dr. Lena Torres, Neurologist, Johns Hopkins Medicine
When to Worry: Red Flags That Demand Medical Attention
Most episodes of dizziness resolve quickly and don’t indicate serious illness. However, certain symptoms suggest a need for prompt medical evaluation:
- Sudden onset of severe dizziness or vertigo lasting more than an hour
- Fainting or near-fainting spells
- Chest pain, palpitations, or shortness of breath
- Slurred speech, facial drooping, or limb weakness (possible stroke)
- Frequent falls or inability to walk without support
- Dizziness accompanied by hearing loss or ringing in the ears
- Numbness, tingling, or confusion
These warning signs could point to conditions such as transient ischemic attack (TIA), arrhythmia, internal bleeding, or central nervous system disorders. Immediate assessment is crucial.
Diagnosis and Evaluation Process
If dizziness persists or raises concern, a healthcare provider will typically conduct a thorough evaluation. This includes:
- Medical history review: Focus on timing, triggers, duration, associated symptoms, and medication use.
- Orthostatic vital signs: Blood pressure and heart rate measured lying down, then after one and three minutes of standing.
- Neurological exam: Testing balance, coordination, eye movements, and reflexes.
- Hearing and vestibular tests: Electronystagmography (ENG) or videonystagmography (VNG) to assess inner ear function.
- Cardiac monitoring: ECG, Holter monitor, or echocardiogram if arrhythmia is suspected.
- Blood work: To check for anemia, infection, electrolyte imbalances, or diabetes.
In some cases, imaging such as MRI or CT scans may be necessary to rule out structural brain abnormalities.
Action Plan: What You Can Do at Home
While professional diagnosis is key, several lifestyle adjustments can reduce dizziness and improve stability.
- ✅ Rise slowly from bed: Sit at the edge for 30 seconds before standing
- ✅ Drink 6–8 glasses of water daily (more in heat or during exercise)
- ✅ Eat balanced meals regularly to avoid low blood sugar
- ✅ Review all medications with your doctor every 6 months
- ✅ Limit alcohol and avoid hot environments (e.g., saunas, long hot showers)
- ✅ Use assistive devices (cane, walker) if balance is impaired
- ✅ Perform balance exercises (e.g., tai chi, heel-to-toe walking)
Real-Life Example: Maria’s Experience
Maria, a 68-year-old retired teacher, began experiencing dizziness whenever she stood up from her favorite chair. At first, she dismissed it as fatigue. But after two near-falls while walking to the kitchen, she consulted her physician. Her blood pressure dropped from 130/80 mmHg lying down to 90/60 mmHg after standing. Further review revealed her blood pressure medication had recently been increased.
After adjusting her dosage and incorporating slow standing techniques, Maria’s symptoms improved dramatically within a week. Her case highlights how a simple medication change—combined with awareness—can make a significant difference.
Do’s and Don’ts: Managing Dizziness Safely
| Do’s | Don’ts |
|---|---|
| Stay hydrated, especially in warm weather | Stand up too quickly after lying down |
| Use compression stockings if recommended | Ignore repeated dizziness or falls |
| Keep a symptom diary (timing, triggers, severity) | Self-adjust medications without consulting your doctor |
| Engage in regular, moderate physical activity | Exercise in extreme heat or humidity |
| Install grab bars in bathrooms and ensure good lighting | Drive or operate machinery if dizzy |
Frequently Asked Questions
Can anxiety cause dizziness when walking?
Yes. Anxiety and panic attacks can trigger hyperventilation, which alters carbon dioxide levels in the blood and leads to lightheadedness or a floating sensation. However, it’s important to rule out physical causes first, especially if symptoms are new or worsening.
Is dizziness a sign of low iron?
Definitely. Iron-deficiency anemia reduces the blood’s oxygen-carrying capacity, which can lead to fatigue, pale skin, and dizziness—particularly during physical activity. A simple blood test can confirm whether low iron is contributing to your symptoms.
Why do I feel dizzy only when walking, not when standing still?
This may indicate a problem with proprioception (body position sense), vestibular dysfunction, or cerebellar issues. Walking requires complex integration between vision, inner ear signals, and muscle feedback. Disruption in any of these systems can cause imbalance specifically during motion.
Conclusion: Take Control of Your Balance and Health
Dizziness when standing up or walking should not be ignored, especially if it interferes with daily life or occurs frequently. While many causes are manageable through hydration, medication adjustments, or physical therapy, some point to serious underlying conditions. Recognizing red flags and seeking timely care can prevent complications like falls, fractures, or cardiovascular events.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?