Waking up or lying down should be moments of rest, not episodes of disorientation. Yet for many, the simple act of reclining triggers a sudden spinning sensation—dizziness that can last seconds or linger into minutes. This symptom, often dismissed as fatigue or dehydration, may point to underlying vestibular or neurological conditions. Understanding why dizziness occurs when lying down is the first step toward relief. More importantly, knowing how to respond empowers individuals to take control of their health without unnecessary alarm.
The Science Behind Positional Dizziness
Dizziness triggered by changes in head position—especially when lying down or rolling over in bed—is commonly linked to the inner ear. The vestibular system, located deep within the ear, detects motion and helps maintain balance. When this system misfires due to displaced particles or inflammation, it sends false signals to the brain, creating the illusion of movement even when the body is still.
One of the most frequent culprits is benign paroxysmal positional vertigo (BPPV). In BPPV, tiny calcium crystals called otoconia break loose from their normal location in the utricle and migrate into one of the semicircular canals. When you change your head position, these particles shift, stimulating nerve endings and causing brief but intense vertigo. Episodes typically last less than a minute and are reproducible with specific movements.
“Positional vertigo is often underdiagnosed because patients assume it’s just ‘getting old’ or stress-related. But with proper testing and maneuvers, we can resolve it in most cases.” — Dr. Lena Torres, Neurotologist
Common Causes of Dizziness When Lying Down
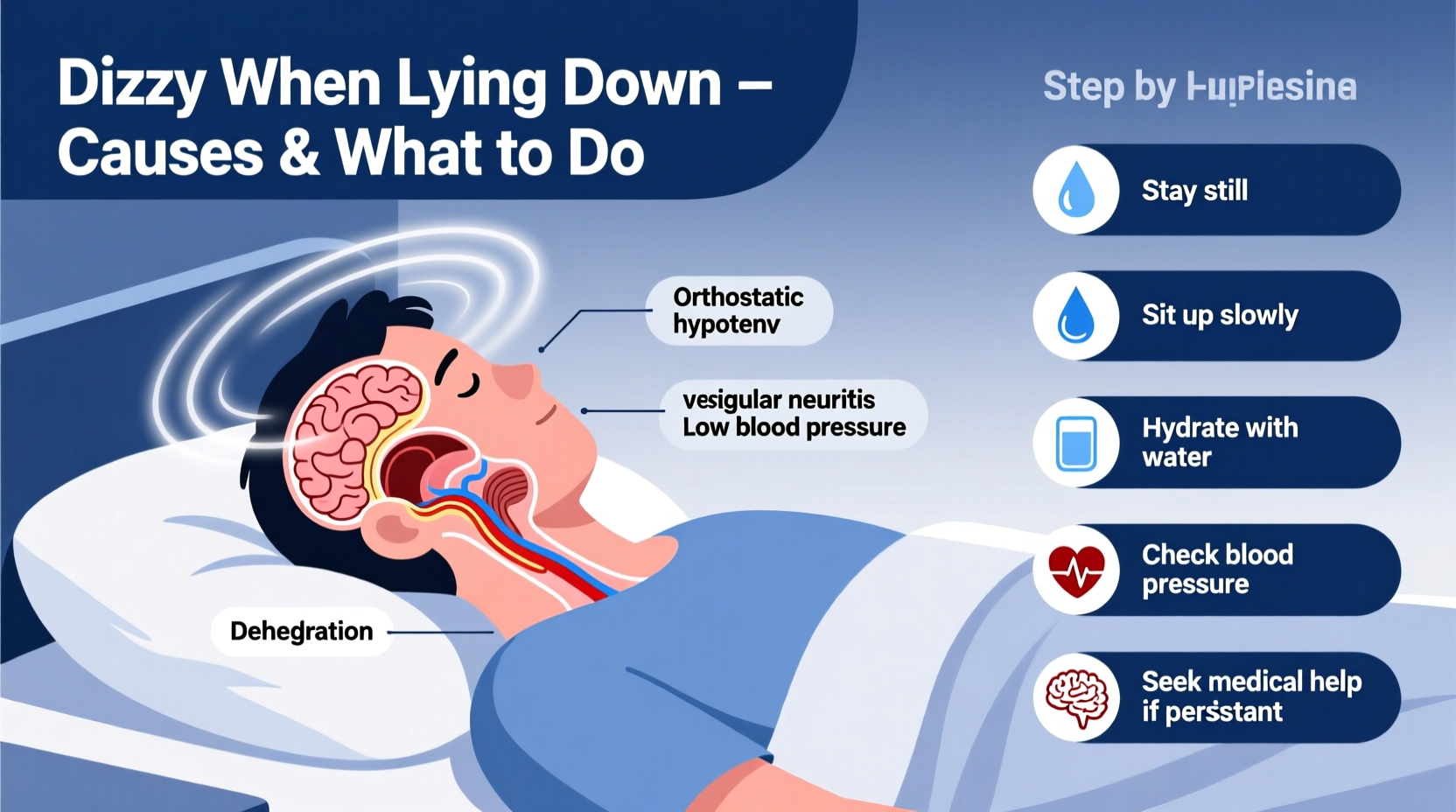
While BPPV is the leading cause, several other conditions can produce similar symptoms:
- BPPV (Benign Paroxysmal Positional Vertigo): Sudden spinning with head movement; most common in adults over 50.
- Labyrinthitis: Inner ear inflammation, often following a viral infection, causing prolonged dizziness and hearing changes.
- Vestibular Neuritis: Inflammation of the vestibular nerve, leading to persistent imbalance without hearing loss.
- Ménière’s Disease: Characterized by episodic vertigo, tinnitus, and fluctuating hearing loss, often worsening at night.
- Orthostatic Hypotension: A drop in blood pressure upon changing position, which may cause lightheadedness rather than true vertigo.
- Cervicogenic Dizziness: Neck dysfunction affecting proprioception, sometimes mimicking positional vertigo.
- Central Causes: Rarely, brainstem or cerebellar issues such as stroke or MS can present with positional dizziness—especially if accompanied by slurred speech, weakness, or double vision.
Diagnosis: How Doctors Identify the Cause
A thorough evaluation begins with a detailed history. Clinicians will ask about onset, frequency, associated symptoms (nausea, hearing loss, headache), and whether certain positions trigger the dizziness. The physical exam often includes the Dix-Hallpike maneuver—a diagnostic test for BPPV.
During the Dix-Hallpike, the patient is quickly moved from sitting to lying with the head turned and extended. If BPPV is present, nystagmus (involuntary eye movement) and vertigo occur after a few seconds and last less than a minute. The direction and latency of nystagmus help determine which ear and canal are affected.
In cases where central pathology is suspected—such as sudden-onset dizziness with neurological signs—imaging like MRI may be warranted. However, for typical BPPV, imaging is unnecessary and not recommended routinely.
Do’s and Don’ts When Experiencing Positional Dizziness
| Do’s | Don’ts |
|---|---|
| Move slowly when changing positions, especially from lying to sitting | Jump out of bed quickly in the morning |
| Sleep with your head slightly elevated on two pillows | Sleep flat on your back if symptoms worsen in that position |
| Perform prescribed repositioning maneuvers (e.g., Epley) | Attempt unguided exercises that could worsen symptoms |
| Stay hydrated and monitor blood pressure | Ignore recurrent dizziness lasting more than a few days |
| Consult a vestibular therapist or ENT specialist | Self-diagnose using online videos alone |
Effective Treatments and Home Management
For BPPV, the gold standard treatment is mechanical repositioning. The Epley maneuver guides dislodged crystals back to their proper chamber using a sequence of head and body positions. It can be performed in a clinic or taught for home use with high success rates—up to 90% resolution after one or two sessions.
Step-by-Step: Performing the Epley Maneuver (Right Ear Affected)
- Sit upright on a bed, turn your head 45 degrees to the right.
- Quickly lie back, keeping your head on the pillow at the same angle. Wait 30 seconds or until dizziness stops.
- Turn your head 90 degrees to the left (now facing left) without raising it. Wait another 30 seconds.
- Rotate your entire body and shoulders to the left, so you’re lying on your left side. Your head should remain in line, looking down at about 45 degrees. Wait 30 seconds.
- Slowly sit up on the left side, remaining still for a moment before standing.
This maneuver should be repeated only as directed, usually once per day until symptoms resolve. Incorrect performance can move crystals into another canal, complicating recovery.
For non-BPPV causes, treatment varies. Vestibular rehabilitation therapy (VRT) helps retrain the brain to compensate for balance deficits. Medications like meclizine or diazepam may reduce acute symptoms but are not recommended long-term as they delay natural compensation.
Real-Life Example: Recovering from Recurrent Nighttime Dizziness
Sarah, a 58-year-old teacher, began experiencing sharp dizziness every time she rolled over in bed. She initially attributed it to stress but noticed the episodes lasted 20–30 seconds and occurred mostly at night. After recording her symptoms and visiting an ENT, she was diagnosed with left-sided BPPV via the Dix-Hallpike test.
Her doctor performed the Epley maneuver in-office. Sarah reported immediate improvement. She was given instructions to avoid rapid head movements and perform the maneuver at home if symptoms recurred. Within a week, her dizziness resolved completely. Six months later, she had no relapses and resumed yoga and swimming confidently.
Sarah’s case highlights the importance of accurate diagnosis and timely intervention. Left untreated, BPPV can persist for weeks or months, impacting sleep and quality of life unnecessarily.
Frequently Asked Questions
Can dehydration cause dizziness when lying down?
Dehydration typically causes lightheadedness upon standing (orthostatic hypotension), not true rotational vertigo when lying down. While it may contribute to general dizziness, it does not mimic BPPV. Staying hydrated supports overall balance function but won’t resolve crystal-induced vertigo.
Is it dangerous to ignore positional dizziness?
Most cases of BPPV are benign and self-limiting, but persistent or worsening symptoms should never be ignored. Central causes like stroke or tumors are rare but serious. Seek urgent care if dizziness is accompanied by slurred speech, limb weakness, severe headache, or double vision.
Can children get BPPV?
It’s uncommon in children but possible, especially after head trauma. Pediatric dizziness is more often linked to migraines, vestibular migraine, or post-viral syndromes. Evaluation by a pediatric ENT or neurologist is recommended if symptoms persist.
Take Control of Your Balance
Dizziness when lying down is more than an inconvenience—it disrupts sleep, increases fall risk, and affects daily confidence. While many causes are treatable, early recognition and appropriate action make all the difference. Whether through targeted maneuvers like the Epley, lifestyle adjustments, or professional care, relief is within reach.
If you’ve experienced recurring vertigo with position changes, don’t wait for it to “pass.” Consult a healthcare provider trained in vestibular disorders. With the right approach, most people regain full stability and return to restful nights without fear of spinning.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?