Waking up or feeling dizzy when lying down is more than just an occasional annoyance—it can disrupt sleep, affect balance, and raise concerns about underlying health. This sensation, often described as vertigo or lightheadedness, may stem from benign conditions or point to more complex neurological or cardiovascular issues. Understanding why it happens and how to manage it empowers individuals to take control of their well-being without unnecessary anxiety.
What Causes Dizziness When Lying Down?
Dizziness upon reclining isn’t always a sign of something serious, but it should never be ignored if it occurs frequently. The most common causes involve the vestibular system—the network in the inner ear responsible for balance—or changes in blood flow and blood pressure. Here are the primary contributors:
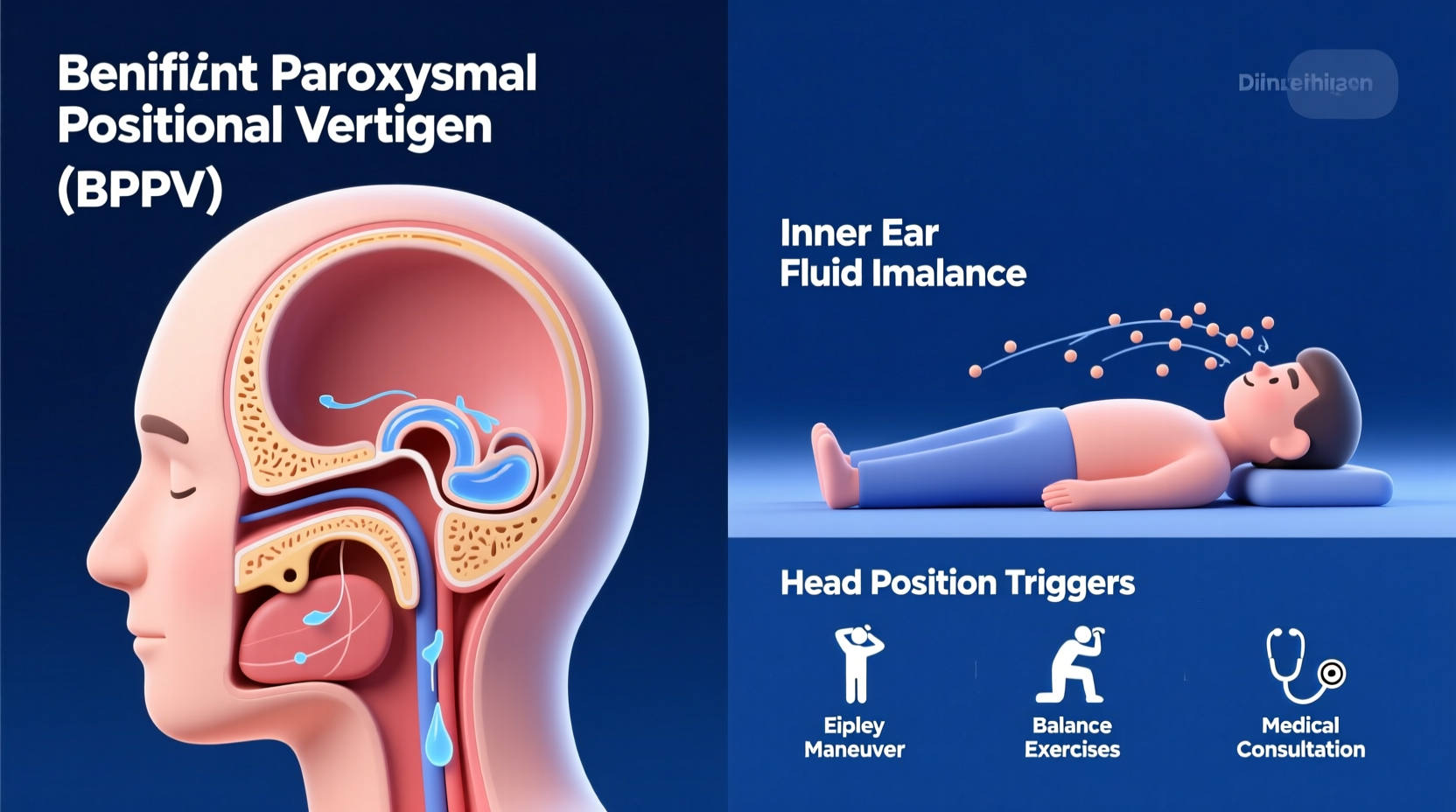
- Benign Paroxysmal Positional Vertigo (BPPV): The leading cause of positional dizziness. Tiny calcium crystals in the inner ear become dislodged and move into canals that detect head motion, sending false signals to the brain.
- Orthostatic Hypotension: A sudden drop in blood pressure when changing positions—such as lying down after standing—can reduce blood flow to the brain, causing lightheadedness.
- Labyrinthitis or Vestibular Neuritis: Inflammation of the inner ear or the nerves connecting it to the brain, often following a viral infection.
- Migraine-Associated Vertigo: Some people experience dizziness as part of a vestibular migraine, even without a headache.
- Anxiety and Hyperventilation: Rapid breathing due to stress can alter carbon dioxide levels in the blood, triggering dizziness, especially when lying still.
“Positional vertigo is one of the most treatable forms of dizziness—if diagnosed correctly.” — Dr. Alan Wong, Neurotologist, Johns Hopkins Medicine
How BPPV Triggers Dizziness at Night
BPPV is particularly notorious for causing dizziness when turning in bed or lying down. The posterior semicircular canal is most commonly affected, and movements like rolling over or tilting the head back can provoke brief but intense episodes of spinning sensations lasting less than a minute.
The condition often begins spontaneously but can follow head trauma, prolonged bed rest, or aging-related degeneration of the inner ear structures. While not dangerous, untreated BPPV can persist for weeks or months, significantly affecting quality of life.
Diagnosis and Medical Evaluation
Accurate diagnosis is essential because treatment varies widely depending on the cause. A healthcare provider will typically perform a physical exam focusing on balance, eye movements, and responses to positional changes.
The Dix-Hallpike maneuver is a standard test for BPPV. During this procedure, the clinician quickly moves your head and body into specific positions while observing for nystagmus—rapid, involuntary eye movements—that confirm inner ear involvement.
In some cases, further testing may be needed:
- Videonystagmography (VNG) to assess inner ear function
- Head CT or MRI scans if neurological causes are suspected
- Blood pressure monitoring during position changes
Do’s and Don’ts When Experiencing Nighttime Dizziness
| Do | Don't |
|---|---|
| Move slowly when changing positions | Jump out of bed quickly |
| Use adequate lighting at night to prevent falls | Ignore recurring episodes |
| Stay hydrated throughout the day | Consume excessive alcohol or caffeine before bed |
| Perform prescribed repositioning exercises | Self-diagnose using online symptom checkers |
Effective Solutions and Treatments
Treatment depends entirely on the root cause. For many, simple maneuvers and lifestyle adjustments bring fast relief.
Epley Maneuver for BPPV
The Epley maneuver is a series of guided head movements designed to reposition displaced otoconia (calcium crystals) back into their proper location in the inner ear. It has a success rate of over 80% after one or two sessions.
- Sit upright on a bed with legs extended.
- Turn your head 45 degrees toward the affected side.
- Quickly lie back, keeping your head tilted off the edge of the bed.
- Wait 30 seconds or until dizziness stops.
- Turn your head 90 degrees to the opposite side without lifting it.
- Rotate your entire body and face downward for another 30 seconds.
- Slowly sit up on the side opposite where you started.
This should be performed under medical supervision initially. Once confirmed safe, it can be done at home.
Managing Blood Pressure-Related Dizziness
If orthostatic hypotension is the culprit, focus on stabilizing blood volume and circulation:
- Rise gradually from sitting or lying positions.
- Increase salt and fluid intake (with doctor approval).
- Avoid hot showers or environments that dilate blood vessels.
- Review medications with your physician—some drugs (like diuretics or antihypertensives) can worsen symptoms.
Mini Case Study: Recovering from Recurrent Nighttime Vertigo
Sarah, a 52-year-old teacher, began experiencing sharp dizziness every time she rolled over in bed. At first, she assumed it was stress or dehydration. After several weeks of disrupted sleep and fear of falling, she consulted an ENT specialist. The Dix-Hallpike test revealed classic signs of right-sided BPPV.
She underwent the Epley maneuver in the clinic and was taught how to repeat it safely at home. Within 48 hours, her symptoms improved dramatically. By the end of the week, the dizziness had resolved completely. Follow-up care included avoiding rapid head motions and sleeping with her head slightly elevated.
Sarah’s case highlights how timely diagnosis and targeted therapy can transform outcomes—even when symptoms seem alarming.
Prevention and Long-Term Management
While not all causes of dizziness can be prevented, certain habits reduce risk and recurrence:
Vestibular Rehabilitation Therapy (VRT)
For chronic or recurrent dizziness, VRT is a customized exercise program led by a physical therapist. It retrains the brain to compensate for inner ear deficits and improves coordination between vision, balance, and spatial awareness.
Lifestyle Adjustments Checklist
- ✅ Stay well-hydrated daily (at least 8 glasses of water)
- ✅ Limit alcohol and caffeine, especially in the evening
- ✅ Maintain consistent sleep patterns
- ✅ Avoid bending over quickly or extending the neck excessively
- ✅ Install night lights in bedrooms and hallways
- ✅ Perform balance-strengthening routines 3 times per week
Frequently Asked Questions
Why do I feel dizzy only when I lie on my left side?
This likely indicates unilateral BPPV affecting the left ear. The dizziness occurs when the dislodged crystals shift within the semicircular canal during that specific movement. Diagnosis via the Dix-Hallpike test can confirm which side is involved.
Can dehydration cause dizziness when lying down?
Yes. Dehydration reduces blood volume, making it harder for your body to regulate blood pressure during position changes. Even mild fluid loss can trigger lightheadedness, especially in older adults or those taking blood pressure medication.
Is it normal to feel dizzy when getting up at night to use the bathroom?
Occasional mild dizziness may happen, but frequent or severe episodes are not normal. Nocturnal dizziness could signal BPPV, orthostatic hypotension, or medication side effects. Persistent symptoms warrant evaluation.
Take Control of Your Balance and Sleep
Dizziness when lying down doesn’t have to become a nightly struggle. Most causes are highly treatable with proper assessment and targeted interventions. Whether it's mastering the Epley maneuver, adjusting medications, or improving hydration and sleep posture, small steps lead to significant improvements in comfort and confidence.
If you’ve been dismissing these symptoms as “just part of aging” or stress, reconsider. Seek professional guidance, track your triggers, and apply evidence-based strategies. Your balance—and peace of mind—is worth protecting.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?