Feeling lightheaded or dizzy upon standing is a surprisingly common experience—especially among older adults—but it’s not something to ignore. This sensation, often described as the room spinning or a sudden wave of unsteadiness, typically occurs when blood pressure drops too quickly upon changing posture. While occasional dizziness may be harmless, recurrent or severe episodes can signal underlying health issues. Understanding the causes, knowing how to respond, and recognizing warning signs can help prevent falls and serious complications.
What Happens When You Get Dizzy After Standing?
When you transition from sitting or lying down to standing, gravity pulls blood into your lower body. In response, your heart and nervous system work together to maintain adequate blood flow to the brain. If this process falters, blood pressure drops suddenly—a condition known as orthostatic hypotension (or postural hypotension)—leading to dizziness, blurred vision, or even fainting.
This drop in blood pressure is usually temporary, lasting only seconds to minutes. However, if your body doesn’t compensate efficiently, symptoms can persist and increase fall risk, especially in older individuals.
Common Causes of Dizziness Upon Standing
Dizziness when standing isn’t a diagnosis but a symptom with multiple possible origins. Some are benign and situational; others point to chronic conditions requiring medical attention.
- Dehydration: Low fluid volume reduces blood pressure and impairs circulation.
- Medications: Diuretics, blood pressure drugs, antidepressants, and Parkinson’s medications can affect vascular tone.
- Aging: The autonomic nervous system becomes less responsive over time.
- Prolonged bed rest: Inactivity weakens cardiovascular adaptation.
- Diabetes: Can damage nerves involved in blood pressure regulation (autonomic neuropathy).
- Anemia: Reduced oxygen-carrying capacity leads to fatigue and dizziness.
- Heart conditions: Arrhythmias, heart failure, or valve problems limit cardiac output.
- Parkinson’s disease and other neurological disorders: Impair autonomic control.
“Orthostatic symptoms are often dismissed as normal aging, but they should never be ignored. They can be early red flags for cardiovascular or neurological disease.” — Dr. Lena Patel, Neurologist at Boston General Hospital
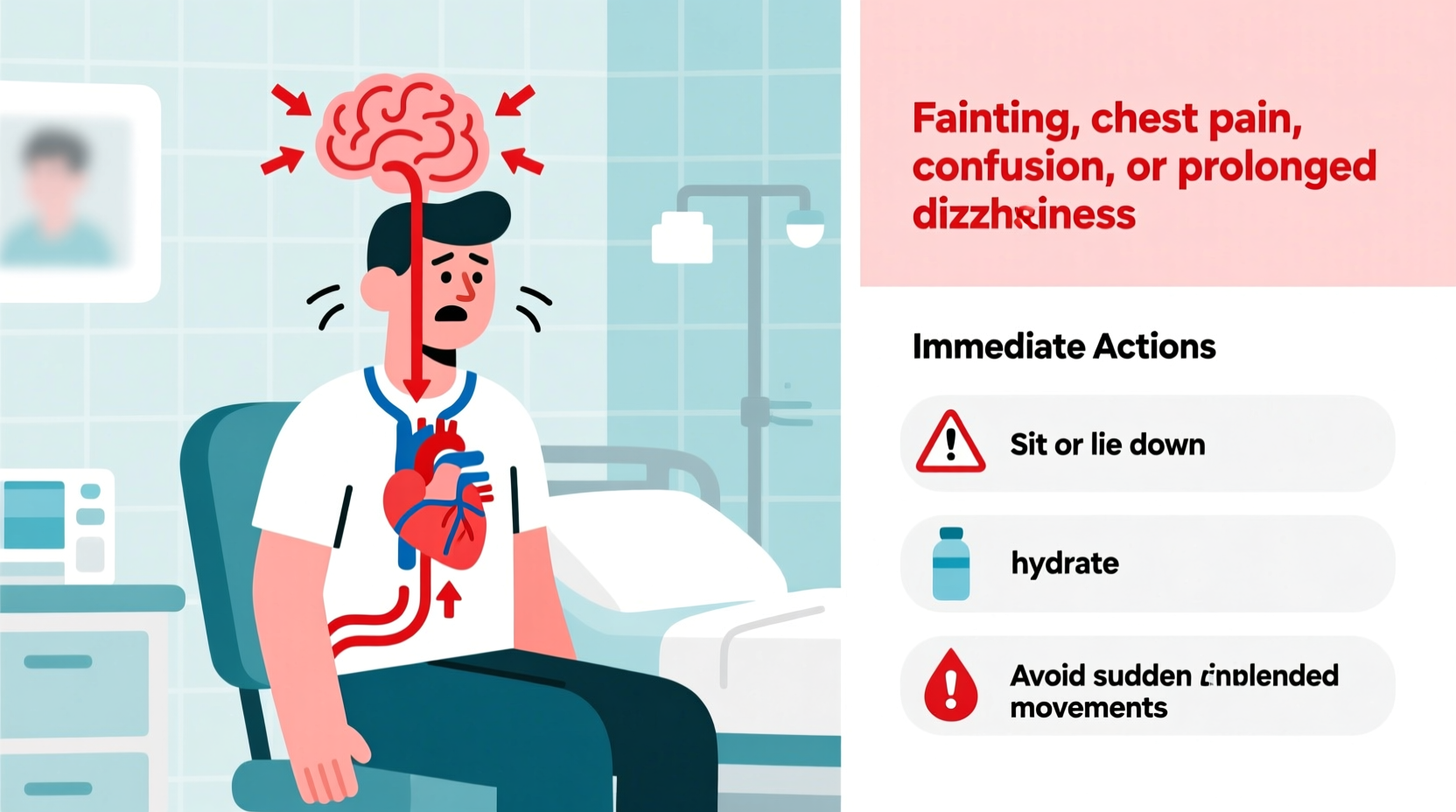
What to Do When You Feel Dizzy Upon Standing
If you feel lightheaded after rising, immediate action can prevent injury and reduce symptom severity. Follow these steps:
- Stop moving: Freeze in place to avoid falling.
- Sit or lie down: Lower your body to restore blood flow to the brain.
- Elevate your legs: If lying down, raise them slightly above heart level.
- Stay still until symptoms pass: Wait 30–60 seconds even after feeling better.
- Hydrate: Drink water, especially if dehydrated or overheated.
For frequent episodes, consider lifestyle adjustments such as increasing salt intake (if approved by your doctor), wearing compression stockings, and avoiding large carbohydrate-heavy meals that can divert blood to the gut.
When to Worry: Red Flags That Require Medical Attention
Not all dizziness is dangerous, but certain symptoms indicate a need for prompt evaluation. Seek medical care if you experience any of the following:
| Symptom | Why It's Concerning | Action |
|---|---|---|
| Fainting or near-fainting | May indicate serious heart rhythm issues or neurological problems | See a doctor within 48 hours |
| Chest pain or palpitations | Possible arrhythmia or heart disease | Seek emergency care |
| Slurred speech or weakness | Could signal stroke or TIA | Call emergency services immediately |
| Dizziness lasting more than 5 minutes | Suggests poor autonomic compensation | Schedule a cardiology or neurology consult |
| Frequent recurrence despite precautions | May require medication review or diagnostic testing | Follow up with primary care provider |
Mini Case Study: Maria’s Morning Dizziness
Maria, a 68-year-old retired teacher, began experiencing dizziness every morning when getting out of bed. At first, she brushed it off as fatigue. But after nearly falling twice while walking to the bathroom, she consulted her physician. Blood tests revealed mild anemia and low sodium levels. Her blood pressure dropped from 130/80 mmHg lying down to 90/60 mmHg after standing for one minute—a clear sign of orthostatic hypotension. Her doctor adjusted her hypertension medication, recommended increased fluid and salt intake, and advised slow positional changes. Within two weeks, her symptoms improved significantly. This case highlights how seemingly minor symptoms can have treatable causes when properly evaluated.
Step-by-Step Guide to Managing Recurrent Dizziness
If you’re prone to dizziness when standing, follow this daily routine to minimize risk:
- Before rising: Perform “bed edge sits”—lie awake for a minute, then sit at the edge of the bed for another minute before standing.
- Morning hydration: Drink a glass of water before getting out of bed to boost circulating volume.
- Monitor medications: Review all prescriptions and supplements with your doctor every six months.
- Check blood pressure: Use a home monitor to track readings lying and standing weekly.
- Exercise regularly: Focus on leg strength and cardiovascular fitness to improve circulation.
- Wear compression stockings: These help reduce blood pooling in the legs.
- Avoid alcohol and heavy meals: Both can worsen postural drops.
Do’s and Don’ts: Quick Reference Table
| Do’s | Don’ts |
|---|---|
| Rise slowly from bed or chair | Stand up quickly after lying down |
| Drink plenty of fluids daily | Go long periods without drinking water |
| Review meds with your doctor annually | Self-adjust doses without guidance |
| Use assistive devices if unsteady | Ignore repeated near-falls |
| Stay physically active | Spend long stretches in bed or on the couch |
Frequently Asked Questions
Is it normal to feel dizzy when standing up occasionally?
Yes, brief lightheadedness lasting a few seconds can happen to anyone, especially after dehydration or prolonged sitting. However, regular or worsening dizziness should be evaluated by a healthcare provider.
Can low iron cause dizziness when standing?
Absolutely. Iron-deficiency anemia reduces the blood’s ability to carry oxygen. This can amplify symptoms of orthostatic hypotension, particularly in women with heavy menstrual cycles or poor dietary intake.
Should I see a specialist for recurring dizziness?
If primary care evaluation doesn’t identify the cause, referral to a cardiologist, neurologist, or autonomic specialist may be necessary. Tests like tilt-table assessments or autonomic function panels can provide deeper insights.
Conclusion: Take Control Before a Fall Happens
Dizziness upon standing is more than just an inconvenience—it’s a signal from your body that something needs attention. Whether due to medication side effects, dehydration, or an underlying condition, addressing the root cause can dramatically improve quality of life and prevent dangerous falls. Small changes in daily habits, combined with timely medical input, make a significant difference. Don’t wait for a serious incident to act. Pay attention to your body, track your symptoms, and advocate for thorough evaluation when needed.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?