Many people experience a sudden wave of dizziness or lightheadedness when transitioning from sitting or lying down to standing. While occasional episodes may seem harmless, frequent or severe dizziness upon standing can signal an underlying issue with blood pressure regulation, hydration, or nervous system function. This sensation—often described as the room spinning or feeling faint—is medically referred to as orthostatic hypotension. Understanding why this occurs is key to managing it effectively and preventing falls or complications.
What Happens When You Stand Up?
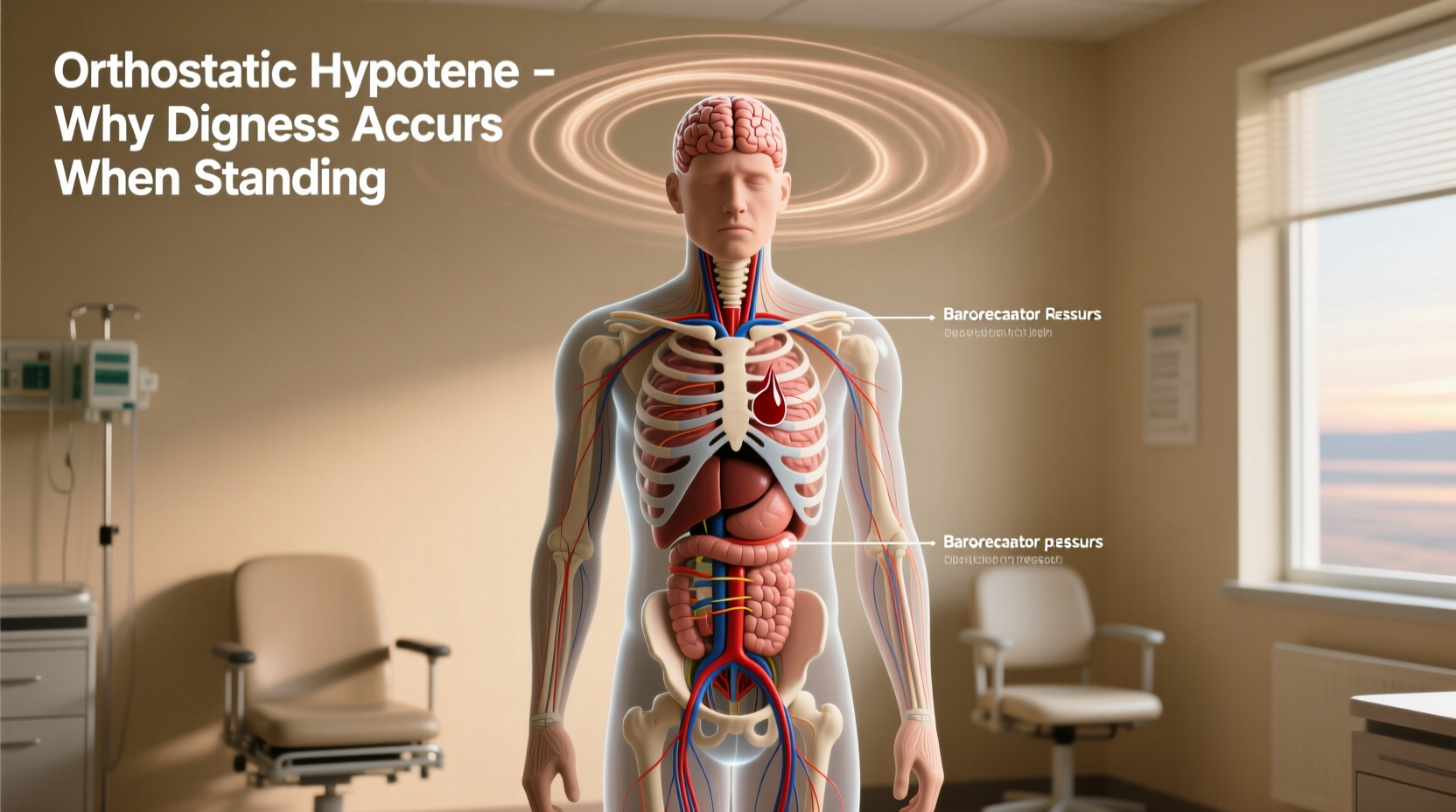
When you stand up, gravity pulls blood downward into your legs and abdomen. In response, your body must quickly adjust to maintain adequate blood flow to the brain. Normally, the autonomic nervous system signals the heart to beat faster and blood vessels to constrict, ensuring consistent cerebral perfusion. However, if this mechanism falters—even briefly—blood pressure drops, leading to reduced oxygen delivery to the brain and causing dizziness, blurred vision, or even near-fainting.
This temporary drop in blood pressure is known as orthostatic (or postural) hypotension. It’s diagnosed when systolic blood pressure falls by at least 20 mm Hg or diastolic pressure drops by 10 mm Hg within three minutes of standing.
Common Causes of Dizziness Upon Standing
Dizziness when rising isn’t always a sign of serious illness, but identifying the root cause helps determine whether lifestyle changes or medical evaluation are needed. Several factors contribute to orthostatic hypotension:
- Dehydration: Insufficient fluid intake reduces blood volume, making it harder for the body to compensate during posture changes.
- Medications: Diuretics, blood pressure drugs, antidepressants, and Parkinson’s medications can interfere with vascular tone or heart rate.
- Aging: As we age, the autonomic nervous system becomes less responsive, increasing susceptibility.
- Prolonged bed rest: Extended immobility weakens cardiovascular adaptation.
- Neurological conditions: Parkinson’s disease, multiple system atrophy, and diabetic neuropathy impair nerve signaling involved in blood pressure control.
- Heart problems: Bradycardia, heart valve issues, or heart failure limit cardiac output during positional shifts.
- Anemia or low blood sugar: These reduce oxygen-carrying capacity or energy supply to the brain.
“Orthostatic hypotension is more than just a nuisance—it’s a window into how well your cardiovascular and nervous systems communicate.” — Dr. Lena Patel, Neurologist and Autonomic Specialist
Who Is Most at Risk?
Certain populations face higher risks due to physiological changes or chronic health conditions. Recognizing vulnerability allows for early intervention.
| Group | Risk Factors | Prevention Focus |
|---|---|---|
| Adults over 65 | Reduced baroreflex sensitivity, polypharmacy, lower muscle mass | Hydration, slow position changes, medication review |
| People with diabetes | Autonomic neuropathy damaging blood pressure nerves | Blood sugar control, foot exams, regular BP monitoring |
| Those on antihypertensives | Excessive lowering of baseline BP | Dose adjustment under supervision, timing of doses |
| Individuals with Parkinson’s | Neurodegeneration affecting autonomic pathways | Compression garments, increased salt intake (if approved) |
Step-by-Step Guide to Managing Orthostatic Dizziness
If you frequently feel dizzy when standing, follow these evidence-based steps to improve stability and reduce symptoms:
- Stay Hydrated: Aim for 6–8 glasses of water daily. Dehydration thickens blood and lowers volume, worsening drops in pressure.
- Rise Slowly: After lying down, sit on the edge of the bed for 30 seconds before standing. Use your arms to push up gently.
- Perform Counterpressure Maneuvers: Cross your legs and tense leg muscles before standing; this helps push blood upward.
- Review Medications: Consult your doctor about any drugs that may be contributing, especially those taken in the morning.
- Increase Salt Intake (Cautiously): For some, slightly more dietary sodium helps retain fluid—but only if not contraindicated by hypertension or kidney disease.
- Wear Compression Stockings: These help prevent blood pooling in the legs, particularly useful for those with venous insufficiency.
- Monitor Blood Pressure: Check readings lying down and after standing to detect patterns. Track them over several days.
Mini Case Study: Recovering Stability After Surgery
Sarah, a 72-year-old recovering from hip replacement surgery, began experiencing frequent dizziness when getting out of bed. She nearly fell twice in one week. Her primary care physician suspected orthostatic hypotension secondary to immobility and pain medication use. A simple bedside test confirmed a 25 mm Hg drop in systolic pressure upon standing.
The care team advised Sarah to increase her fluid intake, perform seated leg lifts before rising, and temporarily discontinue a low-dose diuretic. Within ten days, her symptoms improved significantly. By incorporating slow transitions and compression socks, she regained confidence in her mobility without fear of falling.
This case highlights how reversible factors—especially medication effects and deconditioning—can play a major role in postural dizziness, even in otherwise healthy seniors.
Do’s and Don’ts for Preventing Postural Dizziness
| Do’s | Don’ts |
|---|---|
| Drink water regularly throughout the day | Stand up abruptly from bed or couch |
| Use assistive devices like grab bars in bathrooms | Ignore repeated episodes of lightheadedness |
| Elevate the head of your bed slightly at night | Consume alcohol, which dilates blood vessels and worsens drops |
| Engage in light physical activity like walking or swimming | Self-adjust blood pressure medications without guidance |
Frequently Asked Questions
Is it normal to feel dizzy when standing up occasionally?
Yes, mild and infrequent dizziness upon standing—especially after prolonged sitting or lying down—is common and often resolves within seconds. However, if it happens regularly, lasts longer than a minute, or is accompanied by fainting, confusion, or chest pain, medical evaluation is recommended.
Can anxiety cause dizziness when standing?
Anxiety itself doesn’t directly cause orthostatic hypotension, but hyperventilation or panic attacks can lead to lightheadedness that mimics it. True orthostatic dizziness is tied to measurable blood pressure changes, while anxiety-related dizziness tends to persist regardless of posture.
Should I see a doctor if I feel dizzy every time I stand?
Yes. Recurrent dizziness upon standing warrants assessment to rule out cardiovascular, neurological, or metabolic disorders. Early diagnosis can prevent falls and improve quality of life, especially in older adults.
Conclusion: Take Control of Your Balance
Dizziness when standing up is more than just a fleeting discomfort—it’s a signal from your body that something in your circulatory or nervous system needs attention. Whether triggered by dehydration, medication side effects, or an underlying condition, most cases can be managed with thoughtful lifestyle adjustments and proper medical guidance. By staying hydrated, moving mindfully, and monitoring symptoms, you can regain confidence in your daily movements and reduce the risk of injury.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?