The human gut is home to trillions of microorganisms—bacteria, viruses, fungi—that collectively form the gut microbiome. This complex ecosystem plays a crucial role in digestion, immune function, mental health, and even inflammation control. As awareness of gut health grows, so does the popularity of probiotic supplements. But do they actually improve gut health, or is dietary intake the more powerful factor? The answer isn’t binary. Both matter—but their roles differ significantly depending on individual circumstances, lifestyle, and existing gut conditions.
While probiotics can offer targeted support in specific cases, long-term gut health is fundamentally shaped by consistent dietary patterns. Understanding how these two elements interact allows for smarter, more effective decisions about digestive wellness.
The Role of Probiotic Supplements: Benefits and Limitations
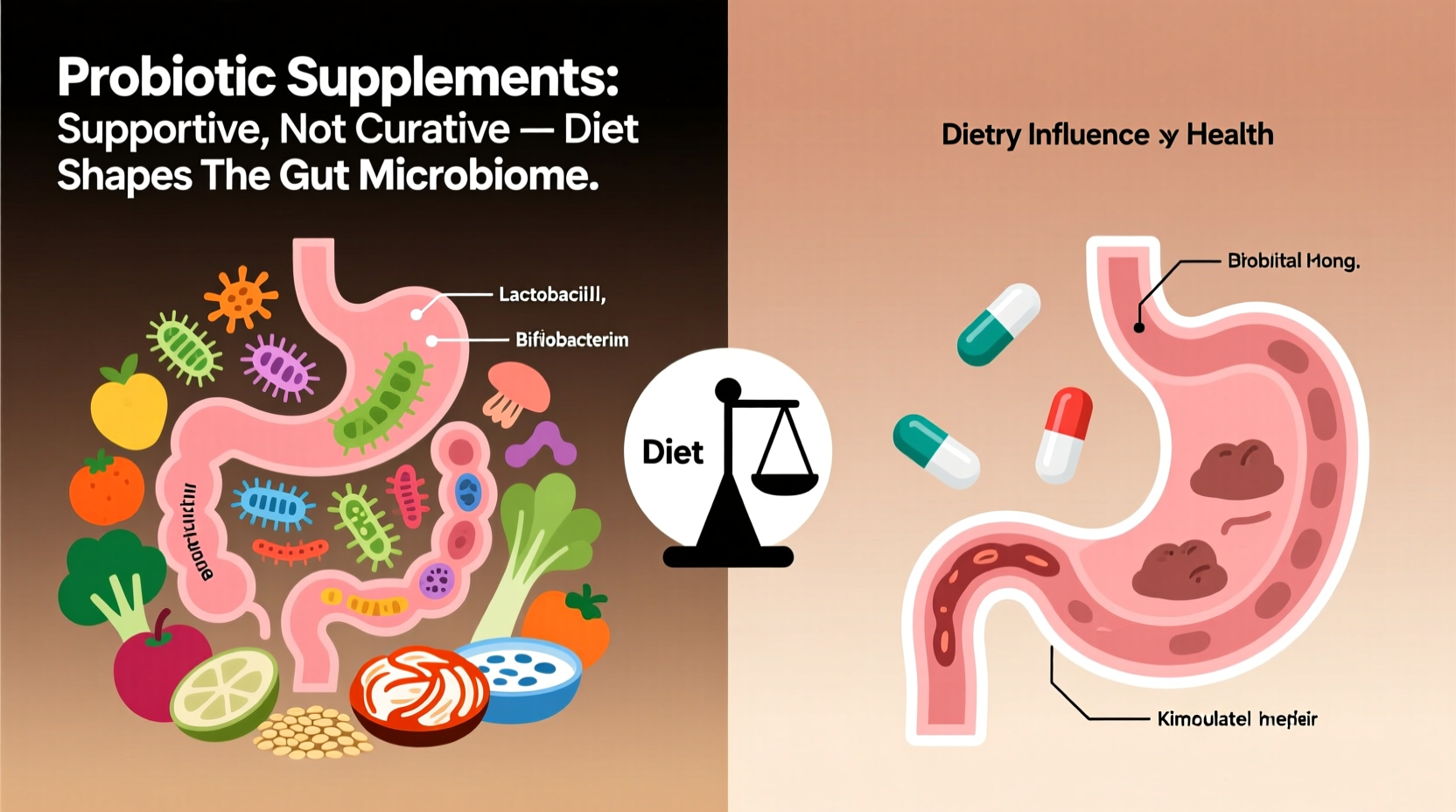
Probiotics are live microorganisms that, when administered in adequate amounts, confer a health benefit on the host (as defined by the World Health Organization). Common strains include Lactobacillus, Bifidobacterium, and certain yeasts like Saccharomyces boulardii. These are available in capsule, powder, and liquid forms, often marketed for bloating relief, improved digestion, or immune support.
Research shows probiotics can be beneficial in several clinical scenarios:
- Antibiotic-associated diarrhea: Taking specific strains like S. boulardii or Lactobacillus rhamnosus GG during antibiotic treatment reduces the risk of diarrhea by up to 50%.
- Irritable Bowel Syndrome (IBS): Some multi-strain formulations have been shown to reduce bloating, gas, and irregular bowel movements.
- Prevention of Clostridioides difficile infection: In high-risk patients, certain probiotics lower recurrence rates after infection.
However, benefits are strain-specific and not universal. A supplement labeled “probiotic” doesn’t guarantee results unless the exact strain and dose used in clinical trials match what’s on the label.
Despite their potential, most probiotics don’t permanently colonize the gut. They act transiently—passing through the digestive tract and exerting influence for days or weeks. Once supplementation stops, levels return to baseline. This suggests that while probiotics may provide short-term modulation, they don’t restructure the microbiome long-term without ongoing use or supportive lifestyle factors.
Diet as the Foundation of Gut Health
If probiotics are temporary visitors, diet is the architect of the gut environment. What you eat directly shapes which microbes thrive and which decline. Unlike supplements, food delivers not only microbes (in fermented varieties) but also the substrates—prebiotics—that feed beneficial bacteria.
A diverse, fiber-rich diet promotes microbial diversity, which is strongly linked to better metabolic health, reduced inflammation, and resilience against pathogens. The average Western diet, low in fiber and high in processed foods, starves beneficial bacteria and encourages the growth of pro-inflammatory species.
“Dietary fiber is the primary fuel for our gut microbes. Without it, even the best probiotic won’t have the environment it needs to function.” — Dr. Emily Carter, Gastroenterology Researcher, Johns Hopkins University
Foods that support a healthy microbiome include:
- Vegetables and fruits: Rich in soluble and insoluble fiber (e.g., onions, garlic, bananas, apples).
- Whole grains: Oats, barley, and brown rice contain beta-glucans and resistant starch.
- Legumes: Beans, lentils, and chickpeas are excellent sources of prebiotic fiber.
- Fermented foods: Yogurt, kefir, sauerkraut, kimchi, miso, and kombucha introduce live cultures naturally.
Studies show that people who consume 30+ different plant-based foods per week have significantly more diverse gut microbiomes than those who eat fewer than 10. This diversity is more predictive of gut health than probiotic use alone.
Comparing Impact: Supplements vs. Diet
To understand the relative influence of each, consider this analogy: probiotics are like planting flowers in a garden, while diet determines the quality of the soil. You can add new plants, but if the soil lacks nutrients, sunlight, or water, they won’t survive long.
| Factor | Probiotic Supplements | Diet |
|---|---|---|
| Impact Duration | Short-term (days to weeks) | Long-term (months to years) |
| Microbial Diversity | Limited increase | Significant improvement |
| Colonization Ability | Rarely permanent | Promotes stable communities |
| Cost Over Time | Moderate to high | Low to moderate |
| Evidence Strength | Strong for specific conditions | Strong for overall health |
This comparison highlights a key insight: supplements work best when layered on top of a solid dietary foundation. For instance, taking a probiotic while eating a high-sugar, low-fiber diet is unlikely to yield meaningful benefits.
When Supplements Make Sense: A Targeted Approach
That said, there are clear situations where probiotic supplements offer measurable advantages:
- During or after antibiotic use: Antibiotics disrupt the gut microbiota. Probiotics can help mitigate side effects and accelerate recovery of balance.
- Traveler’s diarrhea prevention: Strains like S. boulardii have been shown to reduce risk when traveling to high-risk regions.
- Managing IBS or functional bloating: Multi-strain blends such as VSL#3 or specific formulations like Align (Bifidobacterium infantis 35624) may reduce symptoms.
- Immune support in vulnerable populations: Older adults or immunocompromised individuals may benefit under medical supervision.
Yet even in these cases, pairing supplementation with dietary improvements enhances outcomes. For example, someone using a probiotic for IBS will likely see better symptom control if they also increase fiber intake gradually and eliminate common triggers like artificial sweeteners.
Mini Case Study: Sarah’s Gut Health Journey
Sarah, a 34-year-old office worker, struggled with bloating, irregular stools, and fatigue for over a year. She started taking a popular probiotic brand after seeing an influencer recommend it. After two weeks, she noticed slight improvement but still felt off.
She consulted a registered dietitian who reviewed her diet: low in vegetables, high in refined carbs, minimal fermented foods. The dietitian recommended stopping the probiotic temporarily and focusing on dietary changes—adding two servings of vegetables per meal, swapping white bread for whole grain, and including yogurt or kefir daily.
After six weeks, Sarah reported significant improvement in digestion and energy. She then reintroduced a clinically backed probiotic strain (Lactobacillus rhamnosus GG) during a round of antibiotics for a sinus infection. This time, she avoided the gastrointestinal side effects she’d experienced previously.
Her case illustrates that diet created the foundation; probiotics played a supporting role when medically indicated.
Building a Sustainable Gut-Health Strategy
For lasting gut health, focus on consistency over quick fixes. Below is a practical checklist to guide your approach:
- Consume at least 25–30g of fiber daily from varied plant sources
- Eat fermented foods 3–5 times per week (e.g., yogurt, kimchi, sauerkraut)
- Limit ultra-processed foods, artificial sweeteners, and added sugars
- Stay hydrated—water supports mucosal lining and motility
- Use probiotic supplements strategically (e.g., during antibiotics, for diagnosed IBS)
- Read labels: Choose supplements with strain specificity and third-party testing
- Manage stress and sleep—both affect gut barrier function and microbial balance
It’s also important to recognize individual variability. Genetics, medication use, stress levels, and prior antibiotic exposure all shape how one responds to both diet and supplements. What works for one person may not work for another.
Step-by-Step Guide to Optimizing Gut Health
- Week 1–2: Audit Your Diet
Track your current intake. Note fiber sources, processed foods, and fermented items. Identify gaps. - Week 3–4: Increase Fiber Gradually
Add one high-fiber food per day (e.g., chia seeds, lentils, berries). Drink more water to prevent bloating. - Week 5–6: Introduce Fermented Foods
Start with small portions of plain yogurt or sauerkraut to assess tolerance. - Week 7–8: Evaluate Symptoms
Note changes in digestion, energy, and mood. Consider a stool test if issues persist (consult a healthcare provider). - Week 9+: Consider Targeted Supplementation
If needed, choose a probiotic based on evidence for your specific concern (e.g., IBS, antibiotic recovery).
This gradual approach minimizes discomfort and supports sustainable change.
Frequently Asked Questions
Can I get enough probiotics from food instead of supplements?
Yes, for most people, consuming a variety of fermented foods provides sufficient beneficial microbes. Foods like yogurt, kefir, and kimchi contain live cultures and additional nutrients that enhance their effectiveness. Supplements are useful when dietary intake is inconsistent or for specific medical needs.
Are all probiotic supplements the same?
No. Different strains have different effects. A supplement containing Lactobacillus acidophilus may not help with IBS, while a blend with Bifidobacterium strains might. Always check for strain specificity, CFU count, expiration date, and third-party verification (e.g., USP, NSF).
How long does it take to improve gut health?
Noticeable changes can occur within 2–4 weeks of dietary improvements. Microbial composition shifts rapidly with diet, though full stabilization may take months. Consistency is key—short-term efforts rarely lead to lasting results.
Conclusion: Prioritize Diet, Use Supplements Wisely
Probiotic supplements can play a valuable role in gut health—but only when used appropriately and in conjunction with a nourishing diet. Relying solely on pills while neglecting nutrition is like watering a single plant while ignoring the rest of the garden. True gut resilience comes from daily habits: eating diverse fibers, minimizing processed foods, and supporting microbial life through whole-food choices.
For most people, the best strategy is simple: build a diet rich in plants and fermented foods first, then consider supplements as targeted tools when needed. This approach not only supports digestive wellness but also improves overall health—from immunity to mental clarity.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?