Vaginal discharge is a natural part of the female reproductive system’s self-cleaning process. It helps remove dead cells and bacteria, maintaining a healthy balance within the vagina. While some variation in color, texture, and volume is normal, persistent or sudden changes—especially a noticeable increase in dripping white discharge—can signal underlying conditions. Understanding what’s typical versus what may require medical attention is essential for long-term reproductive wellness.
The consistency and appearance of discharge fluctuate throughout the menstrual cycle due to hormonal shifts. However, when white discharge becomes excessive, thick, clumpy, or is accompanied by odor, itching, or discomfort, it may point to infections or hormonal imbalances. This article explores the common causes, different types, and warning signs that indicate when you should consult a healthcare provider.
Normal vs. Abnormal White Discharge
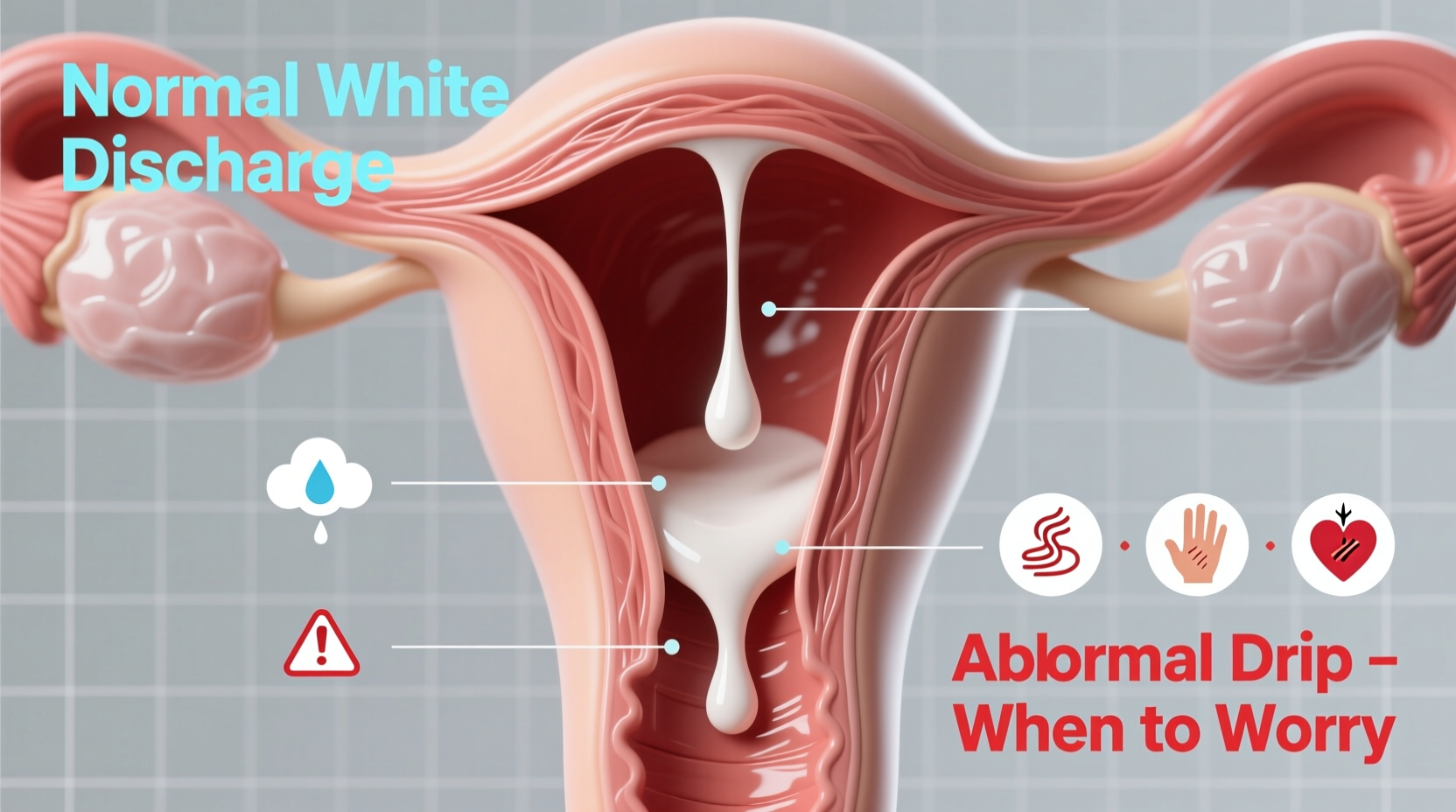
Not all white discharge is cause for concern. In fact, many women experience increased clear or milky-white discharge during ovulation, pregnancy, or sexual arousal—all of which are normal physiological responses. Normal discharge typically has no strong smell, doesn’t cause irritation, and varies in thickness depending on where you are in your cycle.
Abnormal discharge, however, often comes with additional symptoms. These include:
- Strong or foul odor (especially fishy)
- Itching, burning, or redness around the vulva
- Pain during urination or sex
- Change in color (yellow, green, gray)
- Thick, cottage cheese-like texture
- Sudden heavy flow unrelated to cycle phase
“Vaginal discharge is like a window into reproductive health. Changes in pattern or sensation shouldn’t be ignored, especially if they disrupt daily life.” — Dr. Lena Patel, OB-GYN Specialist
Common Causes of Dripping White Discharge
Several factors can lead to an increase in white vaginal discharge. Some are harmless; others require treatment. Below are the most frequent causes categorized by origin.
1. Hormonal Fluctuations
Hormones like estrogen regulate cervical mucus production. During ovulation, estrogen peaks, leading to stretchy, egg-white-like discharge designed to aid sperm movement. Similarly, elevated hormone levels in early pregnancy often result in increased milky-white discharge known as leukorrhea.
2. Yeast Infection (Candidiasis)
A common fungal infection caused by an overgrowth of Candida albicans. Symptoms include thick, white, clumpy discharge resembling cottage cheese, intense itching, and swelling. Unlike bacterial infections, yeast-related discharge usually lacks a strong odor.
Risk factors include antibiotic use, uncontrolled diabetes, high-sugar diets, tight synthetic clothing, and weakened immunity.
3. Bacterial Vaginosis (BV)
BV occurs when the natural balance of vaginal bacteria is disrupted, allowing harmful anaerobes to multiply. The discharge is often thin, white or gray, and emits a distinct fishy odor—particularly after intercourse. While not classified as an STI, BV increases susceptibility to sexually transmitted infections.
4. Sexually Transmitted Infections (STIs)
Chlamydia and gonorrhea can cause white or yellowish discharge, though many cases are asymptomatic initially. Trichomoniasis, another STI, leads to frothy, greenish-yellow discharge with a bad smell, along with irritation and pain.
5. Cervical or Uterine Conditions
Less commonly, excessive discharge may stem from cervical polyps, cervicitis (inflammation of the cervix), or even precancerous changes. These often present with post-coital bleeding, irregular periods, or pelvic discomfort alongside discharge.
Types of White Discharge and What They Mean
Understanding the visual and sensory cues of discharge can help identify potential issues early. The following table outlines key characteristics associated with different conditions:
| Type of Discharge | Possible Cause | Associated Symptoms | Action Needed? |
|---|---|---|---|
| Clear, stretchy (like egg whites) | Ovulation | Mild abdominal twinge, increased libido | No – normal |
| Thick, white, clumpy | Yeast infection | Itching, redness, burning | Yes – antifungal treatment |
| Thin, milky-white with fishy odor | Bacterial vaginosis | Odor worsens after sex, mild irritation | Yes – antibiotics |
| White or yellow, frothy | Trichomoniasis | Genital soreness, painful urination | Yes – prescription medication |
| Increased milky discharge, no odor | Pregnancy | Missed period, breast tenderness | No – unless other symptoms appear |
When to Worry: Red Flags Requiring Medical Attention
While occasional changes in discharge are expected, certain signs warrant prompt evaluation by a healthcare provider. Delaying care can lead to complications such as pelvic inflammatory disease (PID), infertility, or systemic infection.
Seek medical advice immediately if you experience:
- Discharge with a strong, unpleasant odor
- Persistent itching or burning that interferes with sleep
- Pain in the lower abdomen or pelvis
- Bleeding between periods or after sex
- Fever accompanied by unusual discharge
- Recurrent infections (four or more yeast infections per year)
“If you’ve tried over-the-counter treatments without relief, don’t keep guessing. A proper diagnosis prevents mismanagement and protects your reproductive health.” — Dr. Amara Singh, Women’s Health Consultant
Mini Case Study: Recognizing Recurrent Yeast Infections
Sarah, a 29-year-old teacher, noticed recurring episodes of thick white discharge every few weeks. She initially treated herself with antifungal creams, assuming it was simple yeast overgrowth. However, symptoms returned shortly after each treatment. After missing work due to discomfort, she visited her gynecologist.
Testing revealed recurrent vulvovaginal candidiasis linked to undiagnosed prediabetes. High glucose levels were feeding yeast growth. With dietary adjustments, blood sugar monitoring, and a prescribed antifungal regimen, Sarah’s symptoms resolved. Her case underscores the importance of identifying root causes rather than treating surface symptoms alone.
Step-by-Step Guide to Managing and Preventing Abnormal Discharge
Whether addressing current concerns or aiming to prevent future issues, follow this practical timeline to support vaginal health:
- Day 1–3: Observe discharge patterns—note color, smell, texture, and timing in your cycle.
- Day 4: Avoid douching, scented soaps, or tight synthetic underwear that trap moisture.
- Day 5: Switch to breathable cotton underwear and change them daily.
- If symptoms persist beyond 7 days: Schedule a gynecological exam. Request testing for yeast, BV, and STIs.
- Upon diagnosis: Complete full course of prescribed medication—even if symptoms improve.
- Ongoing: Maintain balanced diet low in refined sugars, stay hydrated, and practice safe sex with barrier protection.
FAQ: Common Questions About White Discharge
Is white discharge during pregnancy normal?
Yes. Increased estrogen and blood flow to the pelvic area often cause more milky-white, odorless discharge called leukorrhea. However, any change in smell, color, or sensation should be evaluated to rule out infection.
Can stress affect vaginal discharge?
Indirectly, yes. Chronic stress weakens the immune system and alters hormone levels, potentially triggering yeast overgrowth or disrupting vaginal pH balance.
Should I douche if I have excess discharge?
No. Douching removes beneficial bacteria and increases infection risk. The vagina is self-cleaning. Use warm water only for external washing—never inside the vaginal canal.
Conclusion: Take Charge of Your Vaginal Health
Dripping white discharge isn’t always a problem—but knowing when to act can make all the difference. From hormonal shifts to infections, the causes vary widely in severity and treatment needs. Pay attention to your body’s signals, avoid self-diagnosis pitfalls, and seek professional guidance when something feels off.
Healthy discharge patterns reflect overall well-being. By adopting preventive habits, recognizing red flags early, and engaging with healthcare providers proactively, you empower yourself with knowledge and control over your reproductive health.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?