Womb cancer, also known as endometrial cancer, is one of the most common gynecological cancers affecting women, particularly those over 50. While survival rates are high when detected early, delays in diagnosis can significantly impact treatment effectiveness. Recognizing subtle symptoms and understanding reliable detection strategies are crucial for timely intervention. This article outlines the key warning signs, screening approaches, and practical steps women can take to catch womb cancer at its earliest, most treatable stage.
Understanding Womb Cancer: A Brief Overview
The womb, or uterus, consists of several layers, with the innermost lining—called the endometrium—being the most common site for cancer development. Most cases of womb cancer begin here and are classified as endometrial carcinomas. Unlike cervical cancer, which has a standardized screening program (Pap smears), there is no routine screening test for womb cancer. This makes symptom awareness especially vital.
Risk factors include hormonal imbalances (such as unopposed estrogen exposure), obesity, polycystic ovary syndrome (PCOS), late menopause, never having children, and certain genetic conditions like Lynch syndrome. However, even women without these risk factors can develop the disease, reinforcing the need for vigilance across all demographics.
Early Signs That Should Not Be Ignored
The initial symptoms of womb cancer are often mild and mistaken for normal age-related changes, especially during perimenopause or postmenopause. But consistent or unusual changes warrant medical evaluation. Key early signs include:
- Vaginal bleeding after menopause: Any bleeding more than 12 months after the last menstrual period is abnormal and requires prompt investigation.
- Irregular menstrual cycles: Heavier, longer, or more frequent periods in premenopausal women may signal an underlying issue.
- Abnormal vaginal discharge: Watery, bloody, or foul-smelling discharge not linked to infection.
- Pelvic pain or pressure: Persistent discomfort in the lower abdomen, sometimes accompanied by bloating or a feeling of fullness.
- Pain during intercourse: New-onset dyspareunia (pain with sex) that wasn't previously experienced.
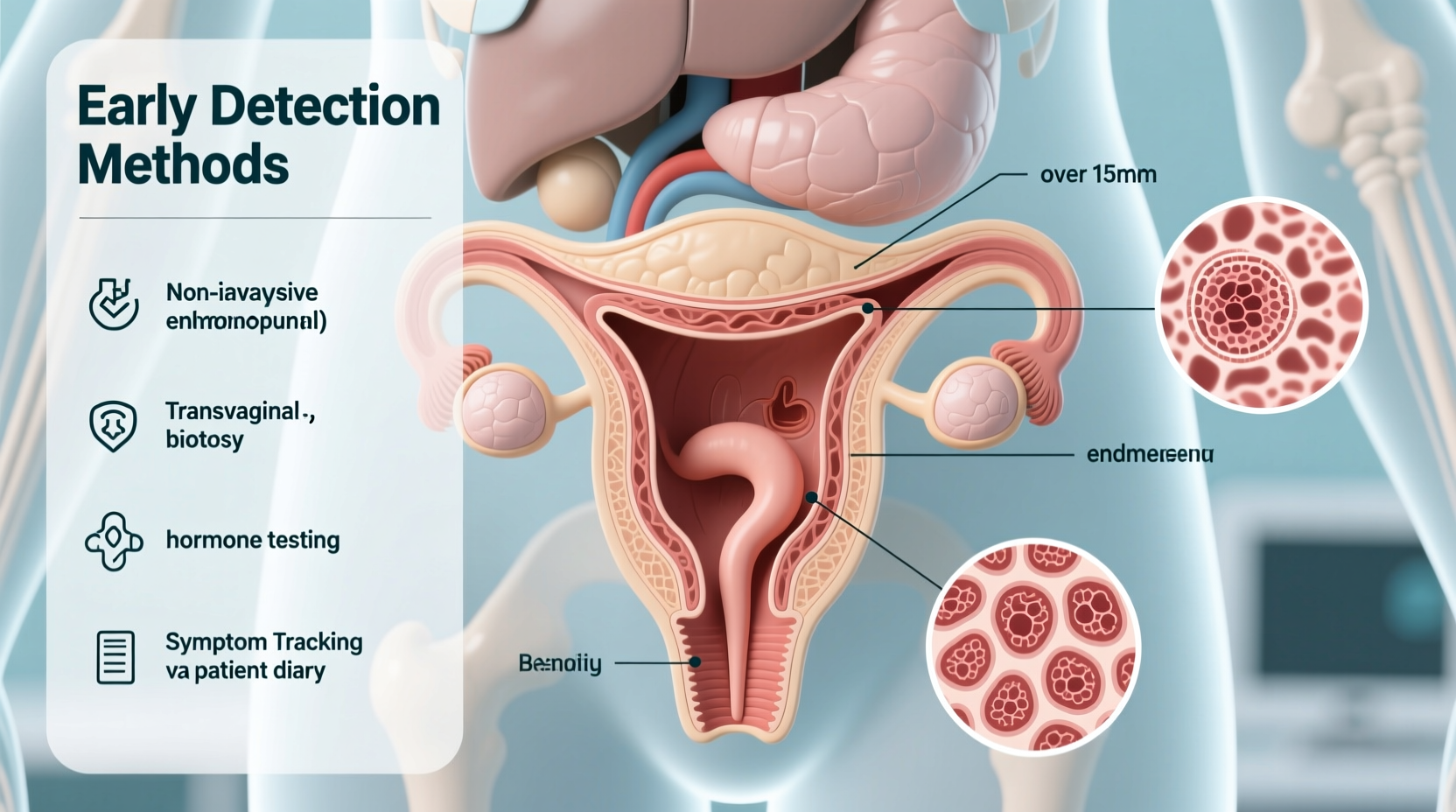
Effective Detection Methods and Diagnostic Pathways
Because there's no standard screening tool like a mammogram or Pap smear for womb cancer, diagnosis relies heavily on clinical evaluation and targeted testing when symptoms arise. The following methods are commonly used to detect abnormalities early:
- Transvaginal ultrasound (TVUS): This imaging technique uses sound waves to examine the thickness of the endometrial lining. An abnormally thickened lining (especially in postmenopausal women) raises suspicion and may prompt biopsy.
- Endometrial biopsy: A small sample of tissue is collected from the uterine lining using a thin tube inserted through the cervix. It’s minimally invasive and highly accurate for diagnosing cancer.
- Hysteroscopy: A narrow telescope is inserted into the uterus to visually inspect the endometrium. Often combined with biopsy for precise sampling.
- Dilation and curettage (D&C): If initial biopsy results are inconclusive, a D&C under anesthesia may be performed to scrape tissue from the uterus for analysis.
These procedures are typically initiated only after a woman reports symptoms. This underscores why patient advocacy—speaking up about changes—is essential.
| Method | Purpose | When Used |
|---|---|---|
| Transvaginal Ultrasound | Measures endometrial thickness | First-line imaging for abnormal bleeding |
| Endometrial Biopsy | Collects tissue for cancer diagnosis | After abnormal ultrasound or persistent symptoms |
| Hysteroscopy | Visual inspection of uterine cavity | To locate polyps, fibroids, or suspicious areas |
| Dilation & Curettage (D&C) | Comprehensive tissue sampling | If biopsy is inadequate or results unclear |
Expert Insight: Why Early Diagnosis Matters
“Over 90% of women diagnosed with early-stage endometrial cancer survive at least five years—but this drops dramatically if the cancer spreads. The key isn’t advanced technology; it’s listening to your body and seeking answers quickly.” — Dr. Rebecca Langston, Gynecologic Oncologist, Mayo Clinic
Dr. Langston emphasizes that the biggest barrier to early detection isn’t access to tools—it’s hesitation. Many women dismiss bleeding as “just part of aging” or fear what a diagnosis might mean. Yet, most cases caught early require less aggressive treatment, often limited to hysterectomy without chemotherapy or radiation.
Real-Life Example: A Case of Timely Action
Sarah, a 57-year-old teacher from Oregon, noticed light spotting six months after her final period. She initially brushed it off but decided to see her OB-GYN after reading a public health alert about postmenopausal bleeding. Her doctor ordered a transvaginal ultrasound, which revealed a thickened endometrium. A subsequent biopsy confirmed stage I endometrial cancer.
She underwent a laparoscopic hysterectomy and required no further treatment. Today, she’s cancer-free and actively shares her story to encourage other women to act fast. “I almost waited,” she says. “But catching it early meant I didn’t lose my ovaries, need chemo, or miss a single day of school.”
Step-by-Step Guide to Prompt Detection
If you notice any potential symptoms, follow this timeline to ensure swift evaluation:
- Day 1–3: Document symptoms—note frequency, duration, and characteristics of bleeding or discharge.
- Day 4: Schedule an appointment with your primary care physician or gynecologist. Be specific about changes since menopause or your usual cycle.
- Within 1 week: Undergo a pelvic exam and transvaginal ultrasound if indicated.
- Within 10–14 days: Complete endometrial biopsy if imaging shows abnormalities.
- By Day 21: Receive pathology results and discuss next steps with a specialist if cancer is detected.
Frequently Asked Questions
Can womb cancer occur before menopause?
Yes. While most cases occur after menopause, premenopausal women—especially those with PCOS, obesity, or a family history—can develop endometrial cancer. Irregular or heavy bleeding should always be evaluated, regardless of age.
Is a Pap smear enough to detect womb cancer?
No. Pap smears screen for cervical cancer, not endometrial cancer. They rarely detect womb cancer unless cells are incidentally shed into the cervix. Specific tests like biopsy or ultrasound are required for accurate diagnosis.
What if my ultrasound is normal but I’m still bleeding?
A normal endometrial thickness reduces the likelihood of cancer, but doesn’t rule it out entirely. Persistent symptoms may still require biopsy, especially in high-risk individuals. Always follow up until the cause is confirmed.
Action Plan: What You Can Do Now
Early detection begins with awareness and action. Use this checklist to stay proactive about your reproductive health:
- Track any vaginal bleeding or discharge after menopause—no amount is normal.
- Maintain a healthy weight through balanced diet and regular exercise.
- Discuss family history of cancer with your doctor; consider genetic counseling if Lynch syndrome is suspected.
- Report menstrual irregularities that persist beyond two cycles.
- Seek a second opinion if symptoms are dismissed without investigation.
Conclusion: Your Health Is Worth Advocating For
Womb cancer is highly treatable when caught early, but silent progression means waiting for severe symptoms can be dangerous. The power lies in recognizing subtle changes and insisting on answers. Medical advances mean most women diagnosed early return to full, active lives—often with minimal treatment. Don’t downplay your symptoms or delay care out of fear or inconvenience. Speak up, get tested, and take control of your long-term well-being.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?