Collagen type 2 is a critical structural protein primarily found in cartilage, the vitreous humor of the eye, and the intervertebral discs. Unlike types 1 and 3, which dominate skin, tendons, and bones, type 2 collagen plays a foundational role in maintaining joint integrity and flexibility. As natural collagen production declines with age—typically starting in the mid-20s—supporting this essential protein becomes vital for long-term joint function and overall musculoskeletal wellness. The most effective strategies go beyond generic supplements; they combine targeted nutrition, lifestyle adjustments, and evidence-based supplementation to deliver measurable results.
Understanding Collagen Type 2: Why It Matters
Type 2 collagen is the main component of articular cartilage—the smooth, white tissue that covers the ends of bones where they come together to form joints. Its primary function is to absorb shock and allow bones to glide over one another with minimal friction. When cartilage deteriorates due to aging, injury, or inflammatory conditions like osteoarthritis, joint pain, stiffness, and reduced mobility often follow.
Natural synthesis of type 2 collagen relies on specific amino acids—particularly proline, glycine, and hydroxyproline—as well as co-factors like vitamin C, zinc, and copper. However, dietary intake alone may not be sufficient to maintain optimal levels, especially under physical stress or chronic inflammation. This is where strategic intervention becomes necessary.
“Preserving cartilage health isn’t just about managing pain—it’s about sustaining mobility and quality of life.” — Dr. Alan Foster, Rheumatology Researcher, Mayo Clinic
Top Evidence-Based Solutions for Collagen Type 2 Support
Not all collagen supplements or lifestyle habits are equally effective. The following solutions are supported by clinical research and real-world outcomes:
1. Use Undenatured Type 2 Collagen (UC-II®)
Unlike hydrolyzed collagen peptides, undenatured type 2 collagen retains its triple-helix structure, which allows it to modulate the immune system through oral tolerance. This means it helps reduce autoimmune attacks on joint cartilage—a key mechanism in conditions like rheumatoid arthritis.
A 2013 double-blind, randomized study published in the Journal of the International Society of Sports Nutrition showed that participants taking 40 mg of UC-II daily experienced significantly greater improvement in joint comfort and flexibility compared to those taking glucosamine and chondroitin or placebo.
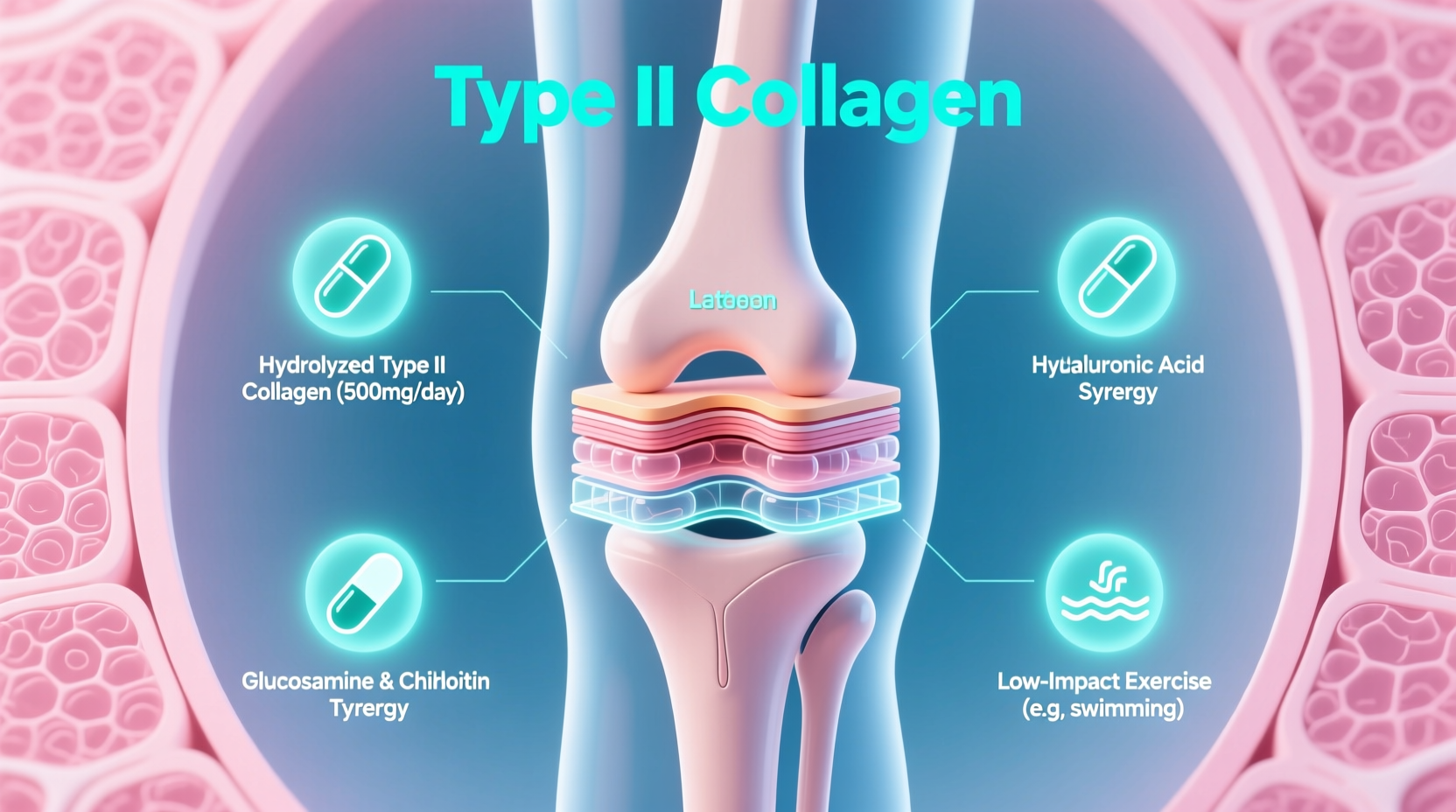
2. Combine With Synergistic Nutrients
Collagen doesn’t work in isolation. Pairing it with complementary compounds enhances absorption and biological activity:
- Vitamin C: Essential for collagen synthesis; acts as a cofactor for enzymes involved in stabilizing collagen fibers.
- Hyaluronic Acid: Supports synovial fluid viscosity, improving joint lubrication.
- MSM (Methylsulfonylmethane): Provides bioavailable sulfur, crucial for connective tissue repair.
- Curcumin: Reduces inflammation that accelerates cartilage breakdown.
3. Prioritize Anti-Inflammatory Nutrition
Diet profoundly influences joint health. Chronic low-grade inflammation can degrade cartilage over time. A Mediterranean-style diet rich in omega-3 fatty acids (from fatty fish, flaxseeds, and walnuts), colorful vegetables, and polyphenol-rich foods (like berries and green tea) creates an internal environment conducive to collagen preservation.
Avoid processed sugars, trans fats, and refined carbohydrates, which promote systemic inflammation and may inhibit collagen regeneration.
Step-by-Step Guide to Optimizing Collagen Type 2 Support
Implementing these solutions systematically increases the likelihood of success. Follow this timeline to build sustainable joint support:
- Week 1–2: Assess Current Joint Health
Track morning stiffness, joint discomfort during movement, and range of motion. Note baseline symptoms. - Week 3: Introduce Undenatured Type 2 Collagen
Begin with 40 mg daily on an empty stomach to maximize immune modulation. - Week 4: Optimize Diet
Eliminate processed foods and incorporate two servings of fatty fish per week. Add leafy greens and antioxidant-rich fruits daily. - Month 2: Add Supporting Supplements
Incorporate vitamin C (500 mg/day), MSM (1,000–2,000 mg/day), and curcumin (500 mg/day). - Month 3+: Monitor Progress & Adjust
Reassess joint comfort and mobility. Consider blood markers like CRP (C-reactive protein) if available.
Comparative Effectiveness of Collagen Types and Forms
| Form | Mechanism | Best For | Daily Dose | Evidence Level |
|---|---|---|---|---|
| Undenatured Type 2 (UC-II®) | Immune tolerance induction | Osteoarthritis, autoimmune joint issues | 40 mg | High (multiple RCTs) |
| Hydrolyzed Type 2 Collagen | Substrate provision for repair | Mild joint wear, preventive care | 5–10 g | Moderate |
| Glucosamine + Chondroitin | Glycosaminoglycan synthesis support | Symptomatic relief only | 1,500 mg + 800 mg | Low to Moderate |
| Collagen Peptides (Type 1 & 3) | General connective tissue support | Skin, tendons, bones—not ideal for cartilage | 10 g | High (for skin/tendon), Low (for joints) |
Real-World Example: Recovery in an Active Adult
Mark, a 48-year-old recreational runner, began experiencing knee pain after increasing his weekly mileage. An MRI revealed early-stage cartilage thinning in his right patellofemoral joint. His doctor advised against NSAIDs due to gastric sensitivity. Instead, Mark started a regimen of 40 mg UC-II® daily, 1,000 mg vitamin C, and 1,500 mg MSM, while switching to a whole-food, anti-inflammatory diet.
After 12 weeks, he reported a 70% reduction in morning stiffness and improved running endurance without pain. His orthopedist noted stabilized cartilage condition on follow-up imaging—suggesting halted degeneration. While not a cure, the combination effectively supported joint homeostasis and functional recovery.
Common Mistakes That Undermine Collagen Support
Even with the right supplements, certain habits can diminish results:
- Taking collagen with meals high in protein: This reduces absorption due to competitive amino acid uptake.
- Ignoring gut health: Poor digestion limits nutrient assimilation, including collagen precursors.
- Overlooking sleep and recovery: Collagen synthesis peaks during deep sleep; chronic sleep deprivation impairs tissue repair.
- Smoking or excessive alcohol use: Both accelerate collagen degradation and impair fibroblast function.
Frequently Asked Questions
Is type 2 collagen safe for long-term use?
Yes. Clinical studies have shown that undenatured type 2 collagen (UC-II®) is safe for continuous use up to 18 months with no serious adverse effects. Minor digestive discomfort has been reported in rare cases.
Can I get enough type 2 collagen from food?
Traditional diets rich in chicken sternum, trachea, and bone broth contain trace amounts of type 2 collagen, but not at therapeutic levels. Modern processing often denatures the protein, reducing efficacy. Supplementation remains the most reliable method for targeted support.
How soon will I notice improvements?
Responses vary, but many users report reduced joint stiffness within 60 days. Full benefits typically emerge after 90–120 days of consistent use, especially when combined with anti-inflammatory lifestyle practices.
Final Recommendations and Action Plan
Supporting collagen type 2 isn’t a one-size-fits-all endeavor. The most effective approach integrates high-quality supplementation with dietary discipline, inflammation control, and healthy lifestyle habits. Begin with a clinically validated form like UC-II®, pair it with synergistic nutrients, and align your daily routine with joint-friendly behaviors.
Joint health is cumulative. Small, consistent actions today lay the foundation for mobility and independence tomorrow. Whether you're an athlete, a weekend warrior, or simply aiming to age with grace, prioritizing collagen type 2 support is one of the smartest investments you can make in your long-term well-being.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?