Group B Streptococcus (GBS), also known as *Streptococcus agalactiae*, is a common bacterium that colonizes the gastrointestinal and genitourinary tracts of up to 25% of healthy adults. While typically harmless in adults, GBS poses significant risks during pregnancy and childbirth, particularly to newborns. Left untreated, it can lead to severe infections such as sepsis, pneumonia, and meningitis in infants. Understanding effective treatment and prevention strategies is essential for expectant parents, healthcare providers, and caregivers alike.
Understanding Group B Strep: Colonization vs. Infection
It's crucial to distinguish between GBS colonization and active infection. Many individuals carry GBS without symptoms—this is colonization. However, when the bacteria invade normally sterile sites like the bloodstream or cerebrospinal fluid, it becomes an infection. In newborns, there are two primary types:
- Early-onset disease: Occurs within the first 7 days of life, most commonly within 24 hours after birth. It is usually acquired during delivery from a colonized mother.
- Late-onset disease: Develops between 7 days and 3 months after birth. Transmission may occur during or after delivery, sometimes from community sources.
Risk factors for early-onset GBS in newborns include preterm labor, prolonged rupture of membranes (>18 hours), maternal fever during labor, and a history of prior infant with GBS disease.
“Routine screening and timely intrapartum antibiotic prophylaxis have reduced early-onset GBS disease by over 80% in the past two decades.” — Dr. Linda Harris, Maternal-Fetal Medicine Specialist
Screening and Diagnosis Protocols
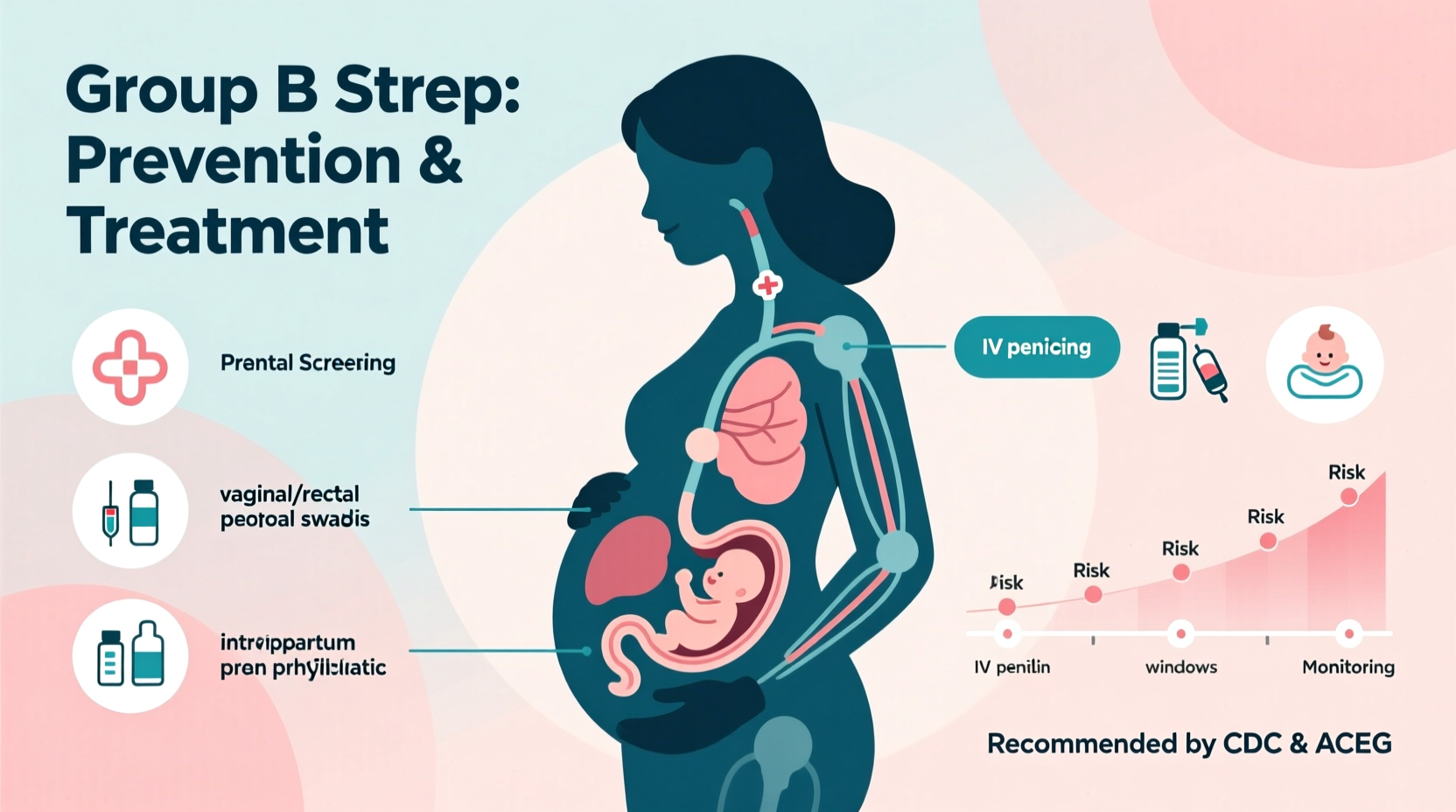
The cornerstone of GBS prevention is universal screening between 35 and 37 weeks of gestation. A vaginal and rectal swab is collected and sent for culture. Results typically return within 24–48 hours. Rapid molecular tests are emerging but not yet standard in most clinics.
If a woman tests positive, she is considered a GBS carrier and should receive antibiotics during labor to prevent transmission to the baby. Not all carriers develop symptoms, but their infants remain at risk without intervention.
Effective Treatment During Labor
Intrapartum antibiotic prophylaxis (IAP) is the gold standard for preventing vertical transmission of GBS from mother to infant. The preferred regimen is intravenous penicillin G, administered at least four hours before delivery. For those allergic to penicillin, alternatives depend on allergy severity:
| Allergy Type | Recommended Antibiotic | Notes |
|---|---|---|
| Mild penicillin allergy | Cefazolin | First-generation cephalosporin; effective against GBS |
| Severe (anaphylactic) allergy | Clindamycin or Vancomycin | Only if isolate is susceptible; resistance testing advised |
| Unknown susceptibility | Vancomycin | Broad-spectrum option when sensitivity is uncertain |
Antibiotics must be given intravenously during active labor—not before—to ensure adequate concentration in fetal tissues at birth. Oral antibiotics during pregnancy do not reliably eradicate GBS colonization and are not recommended for prevention.
Step-by-Step Guide to Managing GBS in Labor
- Confirm GBS status: Review prenatal records for recent screening results (collected at 35–37 weeks).
- Assess risk factors: Even without known colonization, proceed with IAP if there’s fever during labor, membrane rupture >18 hours, or preterm delivery. <3> Initiate IV antibiotics: Start penicillin G unless contraindicated. Dose: 5 million units initially, then 2.5 million units every 4 hours until delivery.
- Monitor fetal well-being: Continue standard labor monitoring alongside antibiotic administration.
- Inform pediatric team: Notify neonatal staff of maternal GBS status so they can assess the newborn appropriately after birth.
Postnatal Care and Newborn Monitoring
After delivery, babies born to GBS-positive mothers who received adequate IAP generally require only routine observation. However, infants whose mothers did not receive timely antibiotics—or had additional risk factors—may need closer evaluation.
Signs of early-onset GBS in newborns include:
- Lethargy or poor feeding
- Fever or unstable body temperature
- Respiratory distress (grunting, rapid breathing)
- Irritability or seizures (in severe cases)
In high-risk situations, clinicians may perform blood cultures and initiate empiric antibiotics while awaiting results. Lumbar puncture may be considered in symptomatic infants to rule out meningitis.
Mini Case Study: Preventing Early-Onset GBS Through Timely Intervention
Sarah, a 29-year-old first-time mother, tested positive for GBS at 36 weeks. She went into spontaneous labor at 39 weeks and arrived at the hospital with ruptured membranes lasting six hours. Her care team promptly started IV penicillin upon admission. She delivered vaginally 5 hours later. The pediatric team observed her newborn for 48 hours, noting no signs of infection. Blood work remained normal, and both mother and baby were discharged home on day two. This case highlights how adherence to screening and timely antibiotic use effectively prevents transmission.
Emerging Strategies and Future Directions
While current protocols are highly effective, researchers are exploring long-term solutions:
- Maternal vaccines: Several GBS vaccine candidates targeting capsular polysaccharides are in clinical trials. A successful vaccine could eliminate the need for antibiotics in labor and provide longer-term immunity.
- Rapid point-of-care testing: Devices capable of detecting GBS in minutes during labor could benefit women without prenatal screening.
- Microbiome modulation: Studies are examining whether probiotics or vaginal microbiota transplants might reduce GBS colonization rates naturally.
Until these innovations become widely available, consistent application of existing guidelines remains the best defense.
FAQ: Common Questions About Group B Strep
Can I pass GBS to my baby if I’m treated during labor?
The risk is significantly reduced—by more than 80%—when appropriate antibiotics are administered at least four hours before delivery. Complete elimination of risk is not guaranteed, but serious outcomes are rare with proper care.
Does having GBS mean I need a C-section?
No. Cesarean section does not eliminate the risk of GBS transmission and is not recommended solely for GBS colonization. Vaginal delivery with antibiotic coverage is safe and effective.
Can GBS come back after treatment?
Yes. A negative test earlier in pregnancy doesn't guarantee you won't test positive later. Similarly, successful treatment during one pregnancy doesn’t confer immunity in future pregnancies. Screening is required each time.
Checklist: Key Actions for Expectant Parents
- Get screened for GBS between 35 and 37 weeks of pregnancy
- Discuss antibiotic options with your provider if you have allergies
- Include GBS status in your birth plan and share it with your medical team
- Arrive at the hospital early enough to receive antibiotics if needed
- Observe your newborn closely for any signs of illness in the first week
- Follow up with your pediatrician regarding postnatal care recommendations
Conclusion: Protecting Mothers and Babies Starts with Knowledge
Group B Strep is a manageable condition when addressed proactively. With standardized screening, timely antibiotic use, and vigilant monitoring, the vast majority of GBS-related complications in newborns can be prevented. Awareness, communication with healthcare providers, and informed decision-making are the most powerful tools available. Stay informed, advocate for your care, and trust that modern medicine offers strong protection when protocols are followed.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?