Belching and flatulence are natural bodily functions—everyone experiences them. But when they become frequent, loud, or disruptive, they can signal underlying digestive issues or lifestyle habits that need attention. Excessive belching (burping) and farting (passing gas) often go hand in hand, stemming from swallowed air, certain foods, or gut imbalances. The good news: most cases can be managed with dietary changes, mindful eating, and simple behavioral adjustments.
What Causes Excessive Belching?
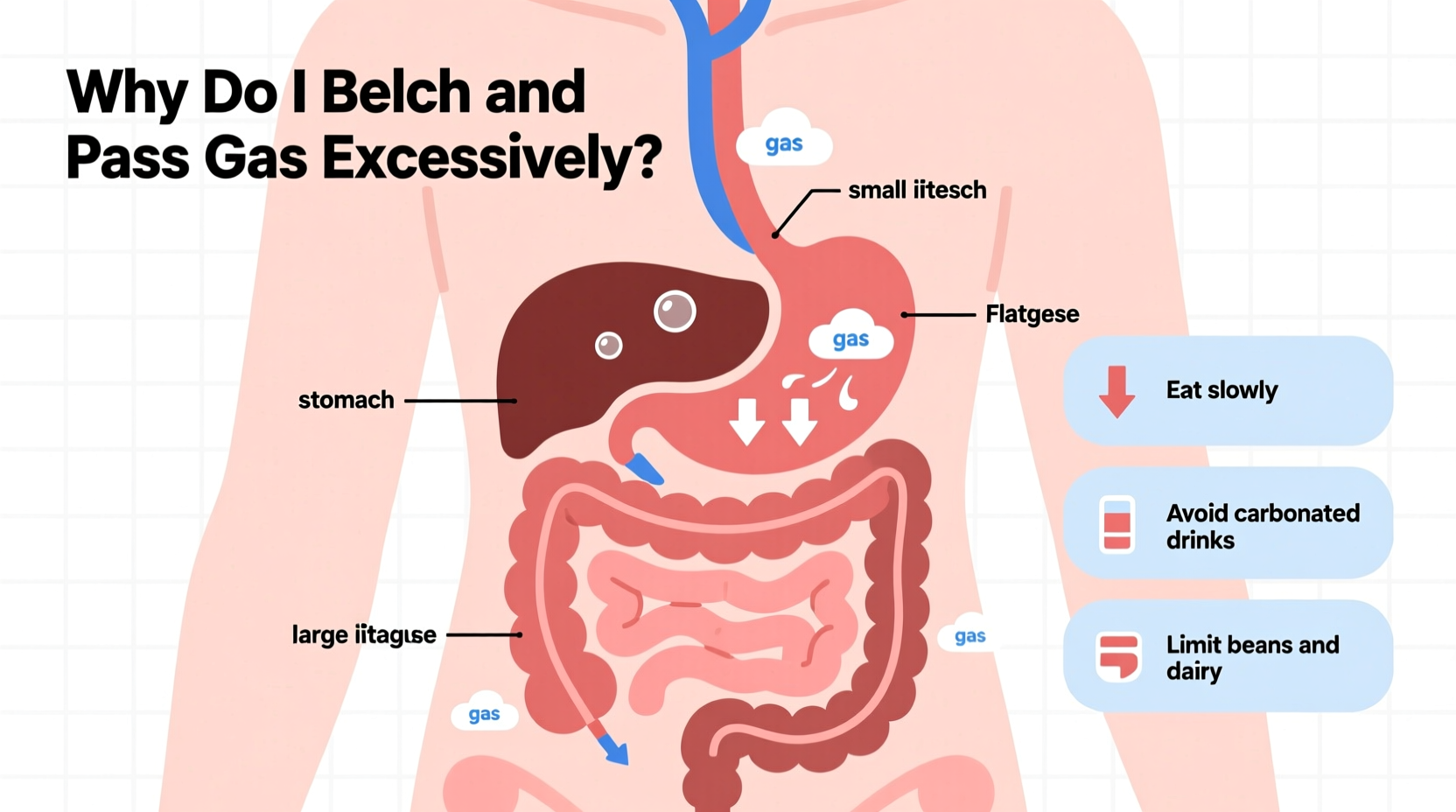
Belching is your body’s way of releasing excess air from the stomach through the mouth. While occasional burping after meals is normal, chronic or excessive belching may point to specific triggers.
- Aerophagia (swallowing air): Common during rapid eating, chewing gum, smoking, or drinking carbonated beverages.
- Gastroesophageal reflux disease (GERD): Stomach acid rising into the esophagus can cause irritation and repeated belching as a reflex to clear discomfort.
- Functional dyspepsia: A condition involving indigestion without an obvious structural cause, often accompanied by bloating and early satiety.
- Hiatal hernia: When part of the stomach pushes into the chest cavity, it can interfere with normal digestion and increase belching.
Why Are You Farting So Much?
Farting up to 20 times a day is considered within the normal range. However, excessive flatulence—especially if foul-smelling or socially uncomfortable—often results from what you eat and how your gut bacteria process it.
The primary source of intestinal gas is bacterial fermentation in the colon. When undigested carbohydrates reach the large intestine, gut microbes break them down, producing gases like hydrogen, methane, and sulfur compounds (which cause odor).
Foods high in fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAPs) are common culprits. These include:
- Beans and lentils
- Cruciferous vegetables (broccoli, cabbage, cauliflower)
- Dairy products (for lactose-intolerant individuals)
- Wheat and rye (due to fructans)
- Sugar alcohols like sorbitol and xylitol (found in sugar-free gum)
“Gas production varies widely between individuals based on diet, gut microbiome composition, and digestive efficiency.” — Dr. Lena Patel, Gastroenterology Specialist
Common Triggers and Lifestyle Factors
Beyond food choices, several daily habits contribute to increased gas production and release:
| Factor | How It Contributes | Easy Fix |
|---|---|---|
| Eating too fast | Increases swallowed air and reduces proper chewing | Chew each bite 20–30 times; pause between bites |
| Carbonated drinks | Introduce CO₂ directly into the digestive tract | Switch to still water or herbal teas |
| Chewing gum | Promotes constant swallowing of air and contains gas-producing sweeteners | Limit use or choose non-sugar alcohol varieties |
| Smoking | Involves repeated inhalation of air and irritates digestion | Quit or reduce frequency |
| Stress | Alters gut motility and microbiome balance | Practice mindfulness or breathing exercises |
Step-by-Step Guide to Reducing Gas
If belching and farting are interfering with your daily life, follow this structured approach to identify and resolve the root causes.
- Track Your Symptoms: Keep a 7-day food and symptom journal. Note meals, timing, gas episodes, and emotional state.
- Eliminate High-FODMAP Foods Temporarily: Remove onions, garlic, beans, apples, milk, and artificial sweeteners for two weeks. Monitor improvements.
- Slow Down at Meals: Aim to spend at least 20 minutes per meal. Put utensils down between bites.
- Reduce Carbonation and Gum: Cut out soda, sparkling water, and sugar-free gum for one week.
- Try Digestive Enzymes: Over-the-counter options like lactase (for dairy) or alpha-galactosidase (Beano) help break down complex carbs.
- Support Gut Health: Consider a probiotic supplement or fermented foods like kefir, sauerkraut, or kimchi to balance gut flora.
- Consult a Professional: If symptoms persist beyond four weeks, see a doctor to rule out SIBO (small intestinal bacterial overgrowth), IBS, or celiac disease.
Mini Case Study: Sarah’s Journey to Less Gas
Sarah, a 34-year-old teacher, came to a digestive health clinic complaining of near-constant belching and embarrassment from unpredictable flatulence during class. She consumed two diet sodas daily, chewed gum frequently, and ate quickly during short lunch breaks.
After keeping a food diary, she discovered her worst symptoms followed meals containing onions, wheat bread, and artificial sweeteners. With guidance, she eliminated carbonated drinks, switched to whole fruits instead of gum, and began eating lunch away from her desk.
Within three weeks, her belching decreased by 70%, and flatulence became predictable and less odorous. A trial of a low-FODMAP diet confirmed sensitivity to garlic and legumes, which she now limits. Sarah reports feeling more confident and comfortable throughout the day.
Checklist: Daily Habits to Reduce Excessive Gas
- ✅ Eat slowly and chew thoroughly
- ✅ Avoid carbonated beverages
- ✅ Limit gum and hard candies
- ✅ Identify and reduce trigger foods
- ✅ Stay hydrated with plain water
- ✅ Walk for 10 minutes after meals
- ✅ Manage stress with deep breathing or meditation
Frequently Asked Questions
Is excessive farting a sign of a serious illness?
Usually not. Most cases stem from diet or habits. However, if gas is accompanied by weight loss, diarrhea, blood in stool, or severe pain, consult a healthcare provider to rule out conditions like inflammatory bowel disease, celiac disease, or colon cancer.
Can probiotics make gas worse?
Yes, initially. Some people experience increased bloating and gas when starting probiotics as the gut adjusts. This typically resolves within a week. Start with a low dose and gradually increase.
Why do I only pass gas at night?
Gas builds up throughout the day but may be suppressed due to social settings. At home or during relaxation, the pelvic floor muscles loosen, allowing accumulated gas to release. This doesn’t indicate a problem unless associated with other symptoms.
When to Seek Medical Help
While most gas-related issues respond to lifestyle changes, certain red flags warrant professional evaluation:
- Persistent bloating lasting more than a few weeks
- Unexplained weight loss
- Changes in bowel habits (chronic diarrhea or constipation)
- Abdominal pain that interferes with daily activities
- Family history of gastrointestinal disorders
A gastroenterologist may recommend tests such as breath testing for lactose intolerance or SIBO, stool analysis, or endoscopy to determine if an underlying condition is contributing to your symptoms.
Conclusion: Take Control of Your Digestive Comfort
Excessive belching and farting don’t have to be a normal part of life. By understanding the causes—whether swallowed air, dietary triggers, or gut imbalance—you can take meaningful steps toward relief. Small changes in how and what you eat often yield significant improvements. Listen to your body, track patterns, and don’t hesitate to seek support when needed. Digestive comfort is achievable, and better days are ahead.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?