Falling is more than just an occasional stumble—it can signal underlying health issues, environmental hazards, or age-related changes that compromise stability. For many, especially adults over 65, frequent falls are a serious concern linked to injury, reduced mobility, and loss of independence. Understanding why falls happen and how to prevent them is essential for maintaining long-term health and confidence in daily movement.
Common Causes of Frequent Falls
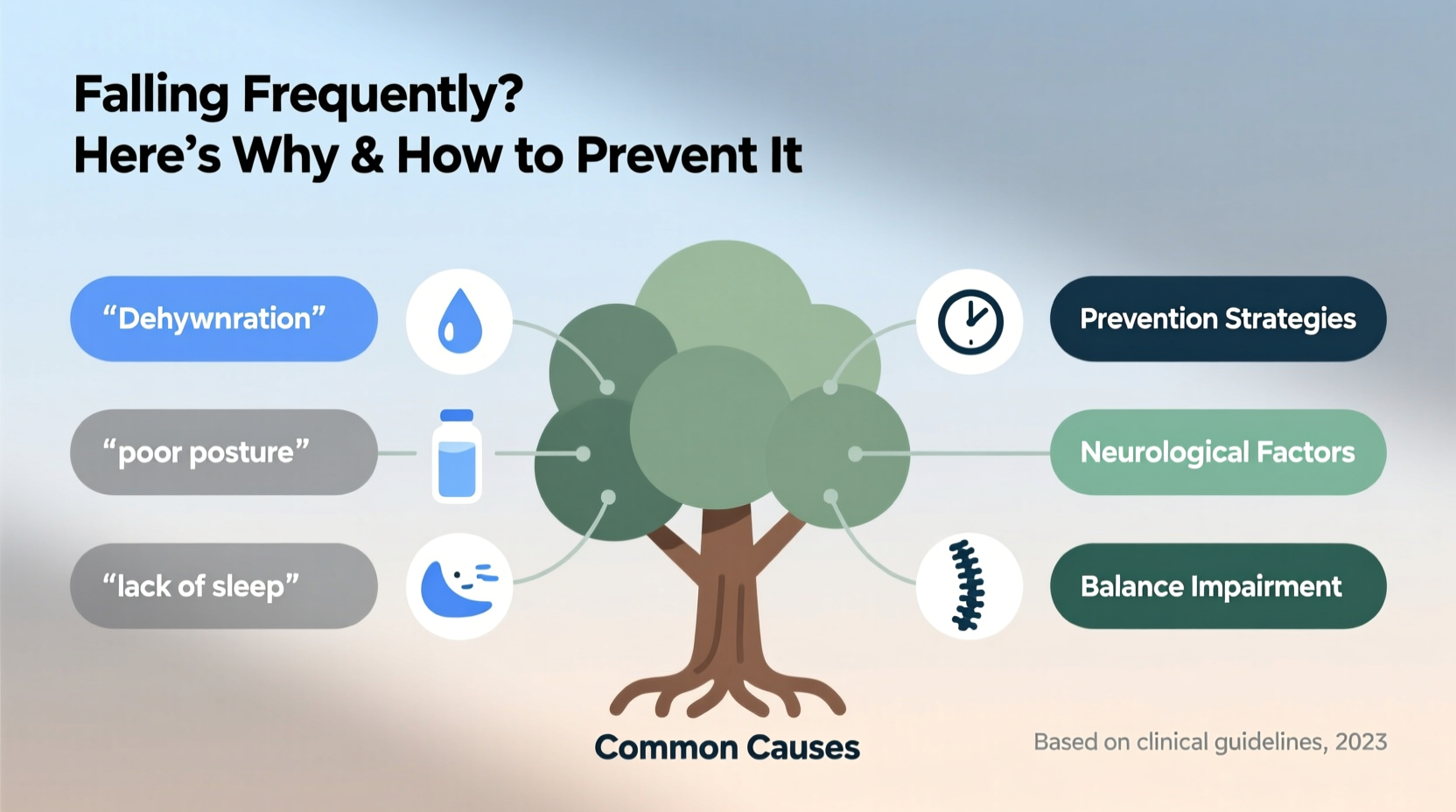
Falls rarely occur due to a single factor. Instead, they result from a combination of physiological, environmental, and behavioral influences. Identifying the root causes is the first step toward effective prevention.
- Muscle weakness: Age-related sarcopenia (loss of muscle mass) particularly affects the legs, reducing strength needed for balance and recovery during slips.
- Poor balance and coordination: Conditions like Parkinson’s disease, inner ear disorders, or neuropathy disrupt the body’s ability to maintain equilibrium.
- Medication side effects: Drugs such as sedatives, antihypertensives, or antidepressants may cause dizziness, drowsiness, or orthostatic hypotension (a sudden drop in blood pressure upon standing).
- Vision impairments: Cataracts, glaucoma, or uncorrected vision reduce depth perception and obstacle detection.
- Chronic health conditions: Diabetes, stroke, arthritis, and heart disease can all contribute to instability.
- Home hazards: Loose rugs, cluttered walkways, poor lighting, and lack of grab bars increase fall risk indoors.
- Foot problems and improper footwear: Painful feet, numbness, or wearing shoes with slick soles significantly affect gait stability.
Prevention Strategies to Reduce Fall Risk
Preventing falls involves both personal health management and environmental modifications. A proactive approach can dramatically lower the likelihood of injury.
1. Strengthen Muscles and Improve Balance
Regular physical activity is one of the most effective ways to prevent falls. Exercises that build leg strength and enhance balance should be prioritized.
- Tai Chi: This low-impact martial art improves coordination, posture, and reaction time.
- Strength training: Focus on quadriceps, hamstrings, and calf muscles using resistance bands or light weights.
- Balance drills: Practice standing on one foot, heel-to-toe walking, or using a balance board.
“Exercise isn’t just about fitness—it’s a critical tool for fall prevention. Even moderate activity three times a week reduces fall risk by up to 40%.” — Dr. Lena Patel, Geriatric Physiotherapist
2. Optimize Vision and Hearing
Impaired senses limit awareness of surroundings. Regular checkups are crucial.
- Update eyeglass prescriptions every 1–2 years.
- Wear bifocals or progressive lenses cautiously—they can distort floor-level vision when walking.
- Address hearing loss; it impairs spatial awareness and increases cognitive load during movement.
3. Conduct a Home Safety Assessment
Most falls occur at home. Simple adjustments can make a significant difference.
| Area | Do | Avoid |
|---|---|---|
| Bathroom | Install grab bars, use non-slip mats | Using towels as bathmats, skipping handrails |
| Stairs | Add sturdy railings, ensure even lighting | Leaving objects on steps, dim lighting |
| Floors | Secure rugs, remove clutter | Loose cords, slippery surfaces |
| Bedroom | Keep a flashlight and phone nearby | Reaching for items at night without lights |
Step-by-Step Fall Prevention Plan
Implementing a structured plan ensures consistent progress. Follow this six-week timeline to reduce fall risk:
- Week 1: Schedule a medical review with your doctor. Discuss medications, chronic conditions, and previous falls.
- Week 2: Visit an optometrist and audiologist. Update glasses or hearing aids if needed.
- Week 3: Perform a room-by-room home safety audit using a checklist (see below).
- Week 4: Begin a balance-focused exercise program—start with 10 minutes daily and gradually increase.
- Week 5: Replace unsafe footwear with supportive, non-slip shoes. Discard worn-out slippers.
- Week 6: Install recommended safety features (grab bars, stair rails, motion-sensor lights).
Essential Fall Prevention Checklist
Use this checklist to evaluate your current risk level and track improvements:
- ✅ Have I reviewed my medications with a doctor in the past year?
- ✅ Are my vision and hearing checked recently?
- ✅ Do I wear supportive, non-slip shoes indoors and outdoors?
- ✅ Are hallways and stairs well-lit, especially at night?
- ✅ Are throw rugs secured or removed?
- ✅ Is there a grab bar near the toilet and in the shower?
- ✅ Can I get out of chairs and beds easily without losing balance?
- ✅ Do I use a cane or walker if recommended by a therapist?
- ✅ Is a charged phone accessible in every room?
- ✅ Am I participating in regular strength and balance exercises?
Real-Life Example: Maria’s Turnaround
Maria, a 72-year-old retired teacher, fell twice within three months—one in her kitchen and another while descending her porch steps. After the second fall resulted in a wrist fracture, she consulted her primary care physician. A full assessment revealed that her blood pressure medication was causing dizziness upon standing, her prescription glasses were outdated, and her bathroom had no grab bars.
Over the next two months, Maria adjusted her medication timing, updated her lenses, installed safety rails, and joined a local Tai Chi class. She also replaced her fluffy bathroom rug with a rubber-backed mat. Six months later, she reported feeling more stable and confident—and has not fallen since.
Maria’s case illustrates how multiple small risks can combine into a dangerous pattern, but targeted interventions can restore safety and independence.
Frequently Asked Questions
Can vitamin D deficiency cause falls?
Yes. Low vitamin D levels are linked to muscle weakness and poor bone health, increasing both the risk of falling and the severity of injuries when falls occur. Adults over 50 should have their levels tested and consider supplementation if deficient.
Are walking aids always necessary for fall prevention?
Not for everyone, but they are highly beneficial when balance or strength is compromised. Using a cane or walker incorrectly can increase risk, so consult a physical therapist to ensure proper fit and technique.
Is fear of falling itself a problem?
Yes. Fear can lead to reduced activity, which causes further weakening of muscles and balance systems—a cycle that increases actual fall risk. Addressing both physical and psychological aspects is key to breaking this pattern.
Conclusion: Take Action Before a Fall Happens
Frequent falling is not an inevitable part of aging. It is a warning sign that deserves attention and action. By understanding the contributing factors—whether medical, environmental, or lifestyle-related—you can implement meaningful changes that enhance stability and safety. The strategies outlined here, from exercise and medication reviews to home modifications, are proven to reduce fall incidents and promote greater independence.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?