Experiencing sudden shifts between feeling hot and cold—sometimes simultaneously—is more common than many realize. These sensations often manifest as chills followed by waves of heat, or a persistent internal sense of fluctuation despite stable room temperatures. While occasionally benign, such symptoms can signal underlying health conditions that warrant attention. Understanding what drives these temperature shifts helps distinguish everyday triggers from warning signs requiring medical evaluation.
How the Body Regulates Temperature
The human body maintains a core temperature of approximately 98.6°F (37°C) through a delicate balance controlled by the hypothalamus, a region in the brain. This internal thermostat responds to external conditions, activity levels, and immune signals. When pathogens invade, for example, the hypothalamus raises the set point to create a fever—a defense mechanism that makes the environment less hospitable to viruses and bacteria.
This recalibration often begins with shivering (to generate heat), leading to chills even in warm environments. As the body reaches the new target temperature, shivering stops and sweating may begin, creating a sensation of intense heat. Once the threat subsides, the hypothalamus resets, prompting sweating and flushing to cool down—resulting in alternating feelings of being too hot and too cold.
Common Causes of Feeling Hot and Cold
Many factors contribute to the sensation of alternating hot and cold. Some are temporary and self-limiting; others require monitoring or intervention.
Infections and Fever
One of the most frequent causes is infection. Bacterial or viral illnesses—from the common cold to urinary tract infections or pneumonia—trigger immune responses that elevate body temperature. The onset of fever typically starts with chills as the body heats up, followed by sweating and warmth as it cools.
Hormonal Changes
Hormonal fluctuations play a significant role, particularly in women. Menopause, perimenopause, and menstrual cycles can all lead to hot flashes and night sweats. These episodes involve sudden vasodilation (widening of blood vessels), causing a rush of heat, redness, and sweating, often followed by chills as the body overcorrects.
“Hot flashes affect up to 80% of women during perimenopause. They’re not just uncomfortable—they can disrupt sleep and daily functioning.” — Dr. Linda Chen, Endocrinologist
Medication Side Effects
Certain medications alter temperature regulation. Antidepressants (especially SSRIs), hormone therapies, antihypertensives, and some diabetes drugs list chills or sweating as side effects. If symptoms began shortly after starting a new medication, consult your healthcare provider before making changes.
Low Blood Sugar (Hypoglycemia)
People with diabetes—or those who skip meals—may experience hypoglycemia. Symptoms include shakiness, confusion, rapid heartbeat, sweating, and a clammy sensation often paired with chills. This paradoxical mix can feel like alternating hot and cold, though it's primarily a response to adrenaline release.
Anxiety and Panic Attacks
Anxiety activates the sympathetic nervous system, triggering fight-or-flight responses. During panic attacks, people often report feeling flushed, dizzy, and sweaty—followed by chills as the episode subsides. Hyperventilation can also distort temperature perception.
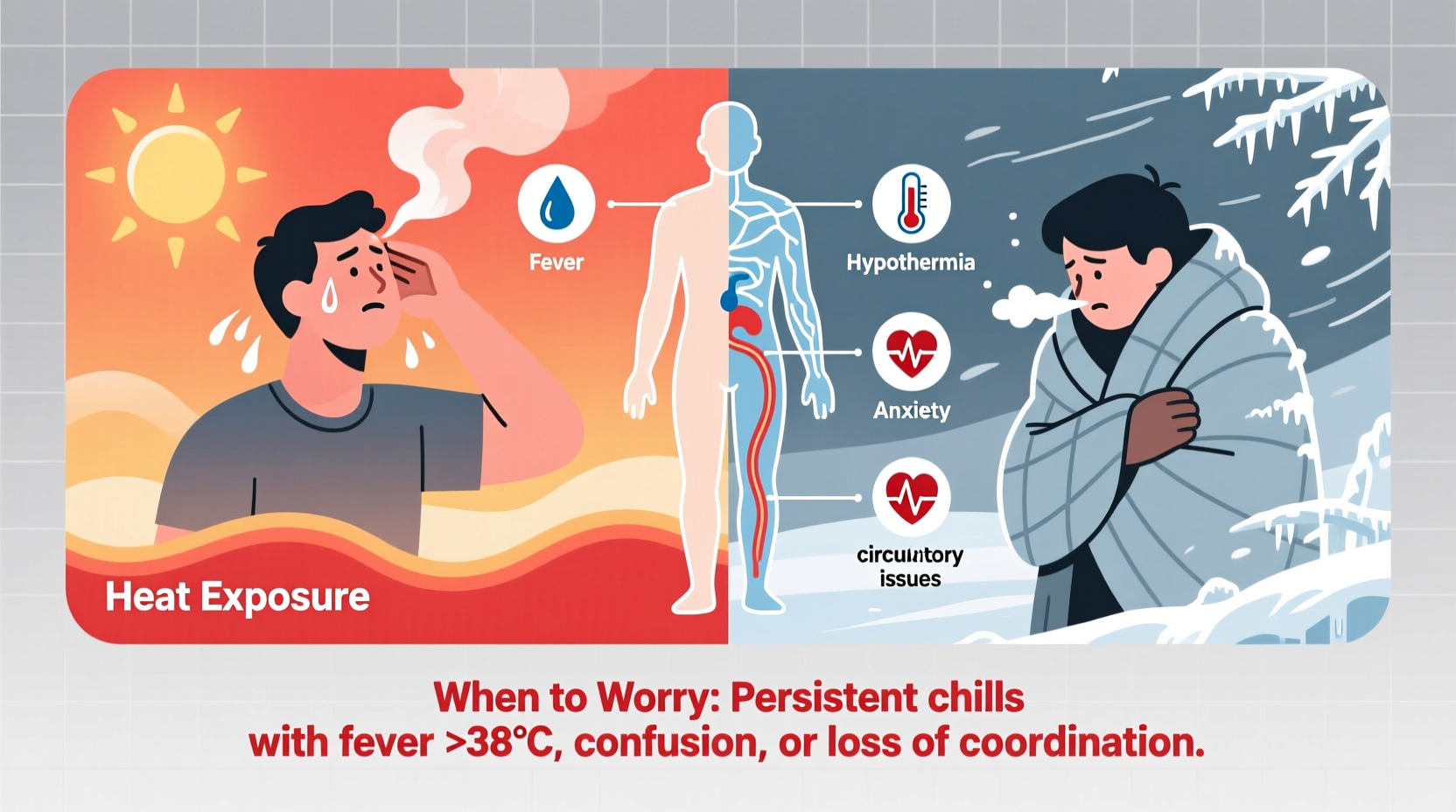
When to Worry: Red Flags and Warning Signs
While occasional temperature fluctuations are normal, certain patterns suggest the need for prompt medical assessment. Persistent or severe symptoms, especially when combined with other systemic issues, should not be ignored.
| Symptom Pattern | Possible Cause | Action Recommended |
|---|---|---|
| Fever above 103°F (39.4°C) lasting more than 48 hours | Bacterial infection, sepsis, serious viral illness | Seek immediate medical care |
| Night sweats with weight loss and fatigue | Tuberculosis, lymphoma, endocrine disorders | Consult doctor for diagnostic tests |
| Chills and rigors without obvious infection | Urinary tract infection, endocarditis, cancer | Urgent evaluation needed |
| Sudden hot flashes in men or premenopausal women | Hormonal imbalance, tumors, medication reaction | Endocrine workup recommended |
| Temperature swings with confusion or dizziness | Severe infection, dehydration, neurological issue | Emergency evaluation advised |
Case Example: Recognizing Early Sepsis
Mark, a 58-year-old man with type 2 diabetes, noticed he felt unusually cold one evening despite wearing a sweater indoors. Over the next few hours, he developed shaking chills, then suddenly felt overheated and began sweating profusely. He dismissed it as the flu until he became confused and nauseous. His wife called an ambulance. At the hospital, doctors diagnosed a kidney infection that had progressed to sepsis. Mark’s alternating chills and fever were early signs of a systemic inflammatory response. Prompt treatment saved his life.
This case underscores that temperature dysregulation isn’t always mild. In vulnerable individuals—such as the elderly, immunocompromised, or those with chronic diseases—these symptoms can escalate quickly.
What You Can Do: Practical Steps and Monitoring
If you're experiencing unexplained hot and cold sensations, taking structured steps can help clarify the cause and determine whether professional care is needed.
- Track your symptoms: Note when the sensations occur, their duration, and any associated factors (e.g., time of day, food intake, stress).
- Take your temperature regularly: Use a digital thermometer to log readings, especially if fever is suspected.
- Assess for additional symptoms: Look for cough, sore throat, abdominal pain, urinary changes, rashes, or unexplained fatigue.
- Review medications: Check side effects of current prescriptions or supplements.
- Stay hydrated: Dehydration impairs thermoregulation and worsens symptoms.
- Manage stress: Practice deep breathing, mindfulness, or gentle exercise to reduce anxiety-related episodes.
Checklist: When to Seek Medical Help
- ✅ Fever above 103°F (39.4°C) that doesn’t respond to medication
- ✅ Chills accompanied by vomiting, stiff neck, or rash
- ✅ Unintentional weight loss with night sweats
- ✅ Confusion, slurred speech, or difficulty staying awake
- ✅ Symptoms lasting more than 7 days without improvement
- ✅ History of cancer, heart disease, or weakened immune system
Frequently Asked Questions
Can feeling hot and cold be a sign of thyroid problems?
Yes. Hyperthyroidism (overactive thyroid) often causes heat intolerance, sweating, and palpitations, while hypothyroidism (underactive thyroid) leads to cold sensitivity and fatigue. Both can disrupt normal temperature perception and regulation. A simple blood test can assess thyroid function.
Why do I feel hot and cold after eating?
Some people experience flushing and sweating after meals, known as gustatory sweating. It’s common after spicy foods or alcohol. In rare cases, it may indicate autonomic dysfunction or a condition called carcinoid syndrome. If recurrent and disruptive, discuss with a physician.
Are night sweats always serious?
No. Occasional night sweats due to a warm room or heavy bedding are normal. However, drenching sweats that require changing clothes or waking multiple times per night—especially without heat exposure—should be evaluated. They may point to infections, hormonal imbalances, or other medical conditions.
Conclusion: Listen to Your Body
Feeling hot and cold intermittently is often part of the body’s natural response to stress, illness, or hormonal change. But when these sensations become frequent, severe, or accompanied by other concerning symptoms, they serve as important signals. Ignoring them can delay diagnosis of treatable—and sometimes serious—conditions.
Pay attention to patterns. Document what you experience. And don’t hesitate to reach out to a healthcare provider if something feels off. Your awareness today could prevent complications tomorrow.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?