Suddenly noticing a rhythmic thumping or pulsing sensation along your spine or lower back can be unsettling. While occasional awareness of internal movement isn’t always alarming, persistent or painful pulsations warrant attention. This sensation—often described as feeling a heartbeat in the back—can stem from normal anatomical variations or signal underlying vascular, neurological, or spinal conditions. Understanding what causes it, how to differentiate benign from serious cases, and knowing when to act is essential for long-term health.
Anatomy Behind the Sensation
The human body houses several major blood vessels that run close to the spine, particularly the abdominal aorta—the largest artery in the abdomen. It travels just in front of the lumbar vertebrae, making its pulsations occasionally perceptible under certain conditions. In slender individuals or during moments of heightened focus on bodily sensations (such as lying down quietly), it's not uncommon to feel this natural rhythm.
Additionally, cerebrospinal fluid circulation within the spinal canal and nerve activity along the dorsal column may contribute to subtle perceptions of movement. However, these are typically imperceptible without instrumentation. When a person becomes aware of a pulse-like sensation, especially if accompanied by pain or other symptoms, it’s crucial to determine whether the cause lies in vascular dynamics, musculoskeletal strain, or more concerning pathology.
Common Causes of Feeling a Pulse in the Back
- Normal aortic pulsation: The abdominal aorta can transmit rhythmic beats felt in the mid-to-lower back, especially when lying supine.
- Low body fat: Reduced adipose tissue increases the likelihood of perceiving deep vascular pulses.
- Pregnancy: Increased blood volume and cardiac output can amplify vessel pulsations near the spine.
- Muscle twitching or spasms: Sometimes mistaken for pulsing; often due to fatigue, dehydration, or nerve irritation.
- Spinal stenosis or disc herniation: Nerve compression may alter sensory perception, creating unusual sensations including rhythmic throbbing.
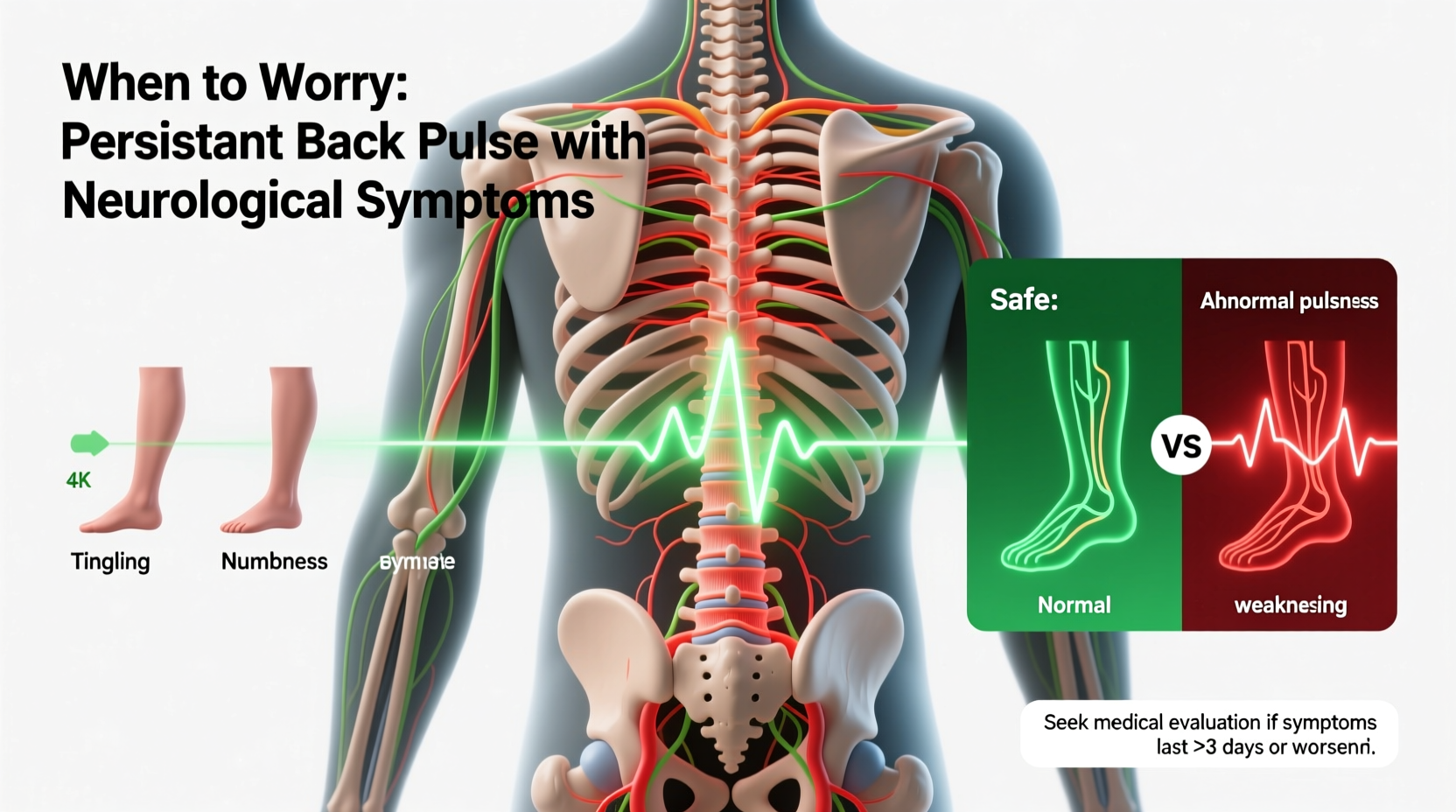
When Should You Be Concerned?
Not every instance of back pulsation requires immediate action. But specific red flags indicate potential pathology needing prompt evaluation. These include:
- Localized, severe pain in the upper or mid-back
- A pulsating mass felt through the skin
- Sudden onset with dizziness, sweating, or chest pain
- History of hypertension, smoking, or connective tissue disorders
- Symptoms worsening at rest or radiating to the chest or legs
“Persistent pulsatile sensations in the back, especially with pain, should never be ignored. They could indicate an abdominal aortic aneurysm—a condition where early detection saves lives.” — Dr. Alan Reyes, Vascular Surgeon, Cleveland Clinic
Danger Signs Requiring Immediate Medical Attention
| Symptom | Possible Cause | Action Required |
|---|---|---|
| Severe tearing pain in back or flank | Aortic dissection | Call emergency services immediately |
| Pulsating bulge in abdomen or back | Abdominal aortic aneurysm (AAA) | Urgent imaging (ultrasound/CT) |
| Loss of consciousness, low blood pressure | Ruptured aneurysm | Emergency surgery required |
| Numbness, weakness in legs | Spinal cord compression | Neurological assessment within hours |
Diagnostic Process and Medical Evaluation
If you experience unexplained pulsations in your back alongside any warning signs, your healthcare provider will likely initiate a systematic workup. This begins with a detailed history and physical exam, focusing on cardiovascular risk factors, trauma, and neurological function.
During the exam, the doctor may palpate the abdomen and lower back to detect abnormal masses or bruits (abnormal sounds indicating turbulent blood flow). Blood pressure readings in both arms and legs may reveal discrepancies suggestive of aortic involvement.
Imaging studies are central to diagnosis:
- Abdominal ultrasound: First-line test for evaluating aortic diameter and detecting aneurysms.
- CT angiography: Provides high-resolution images of blood vessels and surrounding structures.
- MRI of the spine: Used if nerve root or spinal cord issues are suspected.
Depending on results, referrals to specialists such as vascular surgeons, neurologists, or interventional radiologists may follow.
Mini Case Study: Recognizing a Silent Threat
John, a 62-year-old former smoker with controlled hypertension, began noticing a faint pulsing sensation in his lower back while lying down. Initially dismissing it, he returned to his doctor two weeks later after developing dull, persistent mid-back pain. An abdominal ultrasound revealed a 5.2 cm abdominal aortic aneurysm. Thanks to early detection, John underwent elective endovascular repair before rupture occurred. His case underscores how seemingly mild symptoms can mask life-threatening conditions—and why timely investigation matters.
Prevention and Monitoring Strategies
While not all causes of back pulsation are preventable, managing key health risks significantly reduces the likelihood of dangerous vascular events. A proactive approach includes:
- Maintaining healthy blood pressure through diet, exercise, and medication if needed.
- Avoiding tobacco use, which damages arterial walls and accelerates aneurysm formation.
- Regular cardiovascular screening for men over 65, especially those with smoking history.
- Monitoring changes in bodily sensations and reporting new or worsening symptoms promptly.
Do’s and Don’ts: Managing Back Pulsation Awareness
| Do’s | Don’ts |
|---|---|
| Monitor symptoms over time and note changes | Ignore sudden, severe back pain |
| Check blood pressure regularly | Delay seeking care due to fear or uncertainty |
| Stay physically active with low-impact exercises | Engage in heavy lifting if an aneurysm is diagnosed |
| Attend recommended follow-up scans | Assume all pulsations are harmless without evaluation |
Frequently Asked Questions
Can anxiety cause me to feel a pulse in my back?
Yes. Heightened awareness during anxiety or panic attacks can make normal bodily sensations—like aortic pulsations—feel more pronounced. However, anxiety doesn't create actual vascular abnormalities, so ruling out physical causes first is important.
Is it normal to feel a pulse in the lower back when lying down?
In some people, especially those with lean builds, yes. The abdominal aorta lies anterior to the spine, and its pulsations may be transmitted through tissues when reclining. As long as there’s no pain, swelling, or other symptoms, it’s usually benign.
How fast do aortic aneurysms grow?
Most grow slowly—at about 0.1 to 0.4 cm per year. Larger aneurysms (>5 cm) tend to expand faster and carry higher rupture risk, necessitating closer monitoring or intervention.
Conclusion: Listen to Your Body, Act with Purpose
Feeling a pulse in your back isn't automatically dangerous, but it shouldn't be automatically dismissed either. Your body communicates through sensations, and understanding the difference between routine physiology and warning signals is vital. Whether it's adjusting lifestyle habits, scheduling a screening, or seeking urgent care, taking informed steps protects your long-term well-being.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?