A gray spot in your vision can be unsettling, especially if it appears suddenly or grows over time. While some visual disturbances are harmless, a persistent or expanding gray spot may signal an underlying eye condition that requires prompt attention. Understanding the potential causes, associated symptoms, and appropriate actions can help protect your long-term eye health.
Common Causes of a Gray Spot in the Eye
A gray spot isn't always located on the surface of the eye—it often refers to a blind spot or shadow in your field of vision. These spots may appear as dark areas, smudges, or translucent shadows that move with your gaze. Several eye and neurological conditions can cause such visual disruptions.
- Posterior Vitreous Detachment (PVD): As we age, the vitreous gel inside the eye shrinks and pulls away from the retina. This common condition can create floaters and gray shadows, especially noticeable against bright backgrounds.
- Retinal Tear or Detachment: A serious condition where the retina pulls away from its normal position. A new or enlarging gray spot, often accompanied by flashes of light or a curtain-like shadow, is a medical emergency.
- Migraine with Aura: Some people experience temporary visual disturbances—including shimmering spots, zigzag lines, or gray patches—before or during a migraine headache. These usually resolve within 20–60 minutes.
- Macular Degeneration: Age-related macular degeneration (AMD) affects the central part of the retina, leading to blurred or grayed-out areas in the center of your vision.
- Optic Neuritis: Inflammation of the optic nerve, often linked to multiple sclerosis, can cause vision loss, color desaturation, and gray spots.
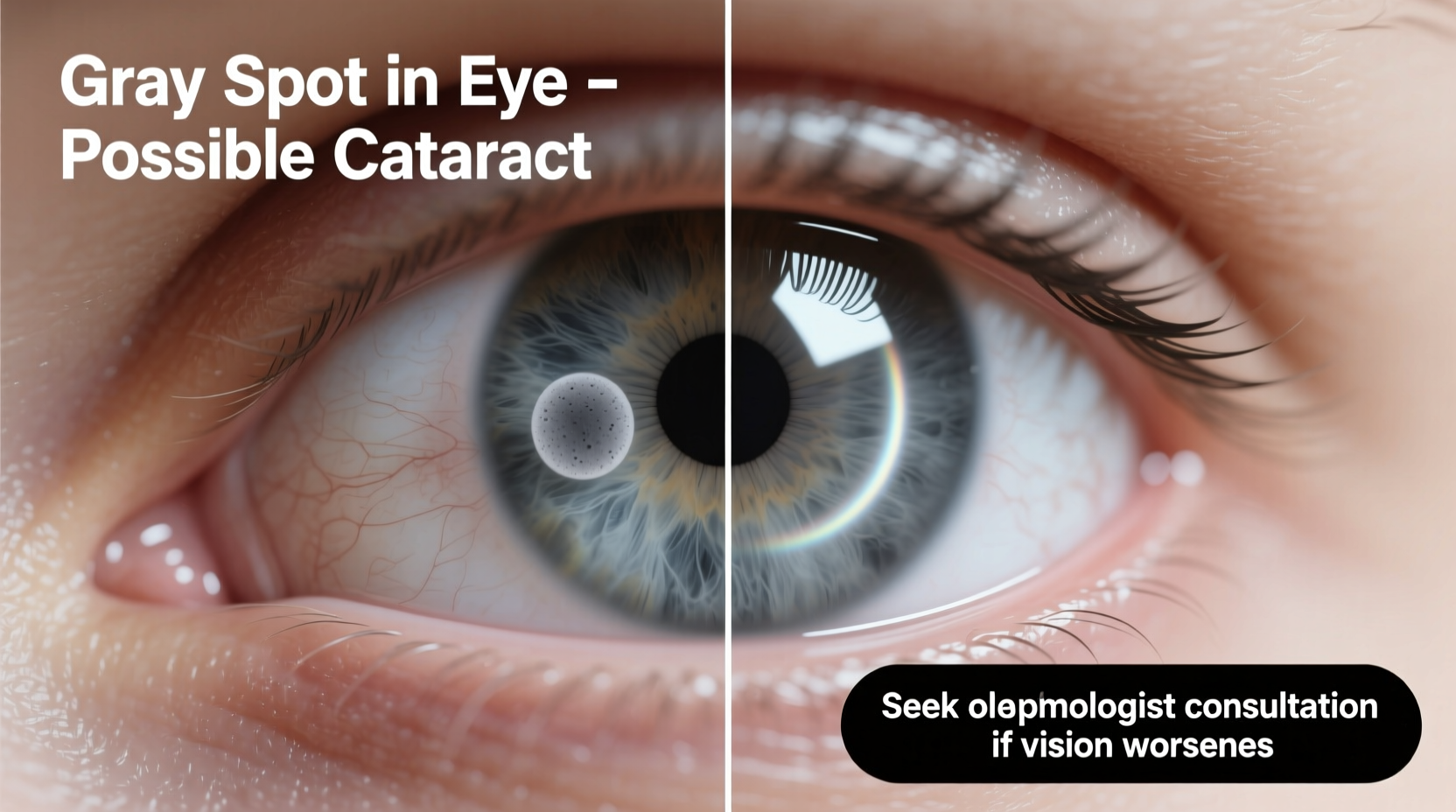
- Eye Trauma or Previous Surgery: Scarring from injury or complications after cataract or retinal surgery may result in permanent blind spots.
Symptoms That Accompany Gray Spots
The presence of additional symptoms helps determine whether a gray spot is benign or a sign of a more serious issue. Pay close attention to:
- New or increasing floaters (small specks or cobwebs drifting across vision)
- Flashes of light, especially in peripheral vision
- Distorted vision (straight lines appearing wavy)
- Loss of peripheral (side) vision
- Pain or discomfort in the eye
- Sudden blurring or dimming of vision
- Color perception changes (colors seem duller)
“Any new onset of visual field defects—especially if unilateral—should be evaluated promptly. Early intervention can prevent irreversible vision loss.” — Dr. Lena Patel, Neuro-Ophthalmologist, Massachusetts Eye and Ear
When to See a Doctor: A Step-by-Step Guide
Not every gray spot demands emergency care, but knowing how to respond based on symptom severity is crucial.
- Assess Onset and Progression: Was the spot sudden or gradual? Is it growing or staying the same?
- Note Associated Symptoms: Record any flashes, floaters, pain, or vision changes.
- Check Both Eyes: Cover one eye at a time to determine if the spot affects one or both eyes.
- Contact an Eye Care Professional: Schedule an appointment with an optometrist or ophthalmologist within 24–48 hours if symptoms persist.
- Seek Emergency Care: Go to an urgent eye clinic or ER immediately if you experience a curtain-like shadow, sudden vision loss, or severe flashes.
Diagnostic Process and What to Expect
When you visit an eye specialist, expect a comprehensive evaluation designed to pinpoint the source of the gray spot.
| Test | Purpose | What It Involves |
|---|---|---|
| Dilated Eye Exam | Inspect retina and vitreous | Eyedrops widen pupils; doctor uses a special lens to examine the back of the eye |
| Visual Field Test | Map peripheral and central vision | You press a button when you see lights appear in your side vision |
| OCT (Optical Coherence Tomography) | Detailed imaging of retinal layers | Non-invasive scan using light waves to detect swelling or thinning |
| Ultrasound (if needed) | View structures when media is cloudy | Sound waves create images of the eye interior, useful if bleeding blocks view |
Based on findings, your doctor may diagnose conditions like vitreous syneresis, macular hole, epiretinal membrane, or even early glaucoma. Treatment varies widely—from monitoring to laser therapy or surgery.
Real-Life Example: Recognizing Retinal Warning Signs
Mark, a 52-year-old teacher, noticed a small gray dot in his right eye while reading. At first, he dismissed it as fatigue. Over three days, the spot grew into a haze resembling a cracked windshield, and he began seeing flashes at night. He visited an ophthalmologist who performed a dilated exam and diagnosed a retinal tear. Laser photocoagulation was performed the same week, sealing the tear before full detachment occurred. Mark credits his quick action with saving his vision.
This case underscores the importance of not ignoring subtle changes—even if painless. Early detection transformed a potentially blinding condition into a manageable one.
Do’s and Don’ts When Experiencing a Gray Spot
| Do’s | Don’ts |
|---|---|
| Monitor changes daily using an Amsler grid | Ignore sudden or worsening symptoms |
| Wear UV-protective sunglasses outdoors | Rub your eyes aggressively |
| Attend all follow-up appointments | Delay seeking care due to fear or cost concerns |
| Control systemic conditions like diabetes and hypertension | Use over-the-counter eye drops without diagnosis |
Frequently Asked Questions
Can a gray spot in my eye go away on its own?
Sometimes, minor floaters or shadows caused by PVD may become less noticeable over weeks or months as the brain adapts. However, structural damage like a retinal tear or macular issue will not resolve without treatment. Never assume a spot will disappear—get it checked.
Is a gray spot always a sign of something serious?
Not always. Some people naturally have minor blind spots due to optic disc anatomy, and migraines cause temporary gray zones. But any new, changing, or symptomatic spot should be evaluated to rule out dangerous conditions.
Can high blood pressure or diabetes cause gray spots?
Yes. Both conditions can lead to retinopathy—damage to the blood vessels in the retina—which may manifest as blind spots, blurred vision, or floating shadows. Regular eye exams are essential for those with chronic diseases.
Action Plan: Protecting Your Vision Moving Forward
If you’ve experienced a gray spot in your vision, take these proactive steps:
- Schedule a comprehensive eye exam with an ophthalmologist, even if symptoms have improved.
- Learn your family history of eye diseases like glaucoma, AMD, or retinal disorders.
- Adopt protective habits: wear sunglasses, avoid smoking, manage blood sugar and blood pressure.
- Use the Amsler grid monthly to self-monitor central vision changes.
- Keep emergency contacts handy for eye specialists who offer after-hours care.
“The eye is the only place in the body where blood vessels and nerves can be seen directly. A gray spot might be your body’s way of signaling a deeper issue—listen to it.” — Dr. Alan Zhou, Retina Specialist, Johns Hopkins Medicine
Conclusion
A gray spot in your eye shouldn’t be ignored, even if it seems minor or painless. From benign floaters to sight-threatening retinal tears, the range of possible causes is broad—and timely diagnosis makes all the difference. By understanding symptoms, acting quickly, and partnering with eye care professionals, you can preserve your vision and prevent long-term complications. Your eyes give you the gift of sight—protect them with informed vigilance.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?