Stomach aches are among the most common discomforts people experience, yet they vary widely in cause, severity, and appropriate response. From mild indigestion to food poisoning or chronic conditions like irritable bowel syndrome (IBS), understanding how to respond wisely can mean the difference between quick recovery and prolonged distress. This guide explores evidence-based remedies, smart dietary decisions, and practical strategies that support both immediate relief and long-term gut health.
Understanding Common Causes of Stomach Aches
Before treating a stomach ache, it's essential to identify its likely origin. While severe or persistent pain requires medical evaluation, many cases stem from manageable causes:
- Digestive overload: Overeating, especially fatty or spicy foods, slows digestion and increases pressure in the stomach.
- Gas and bloating: Swallowed air or fermentation of undigested carbohydrates in the colon leads to trapped gas.
- Food intolerance: Lactose, fructose, or gluten sensitivity can trigger cramping and diarrhea.
- Infections: Viral gastroenteritis (\"stomach flu\") or bacterial contamination often comes with nausea, vomiting, and fever.
- Stress and anxiety: The gut-brain axis means emotional stress can manifest as abdominal pain or altered motility.
- Medication side effects: NSAIDs like ibuprofen may irritate the stomach lining, increasing acid production.
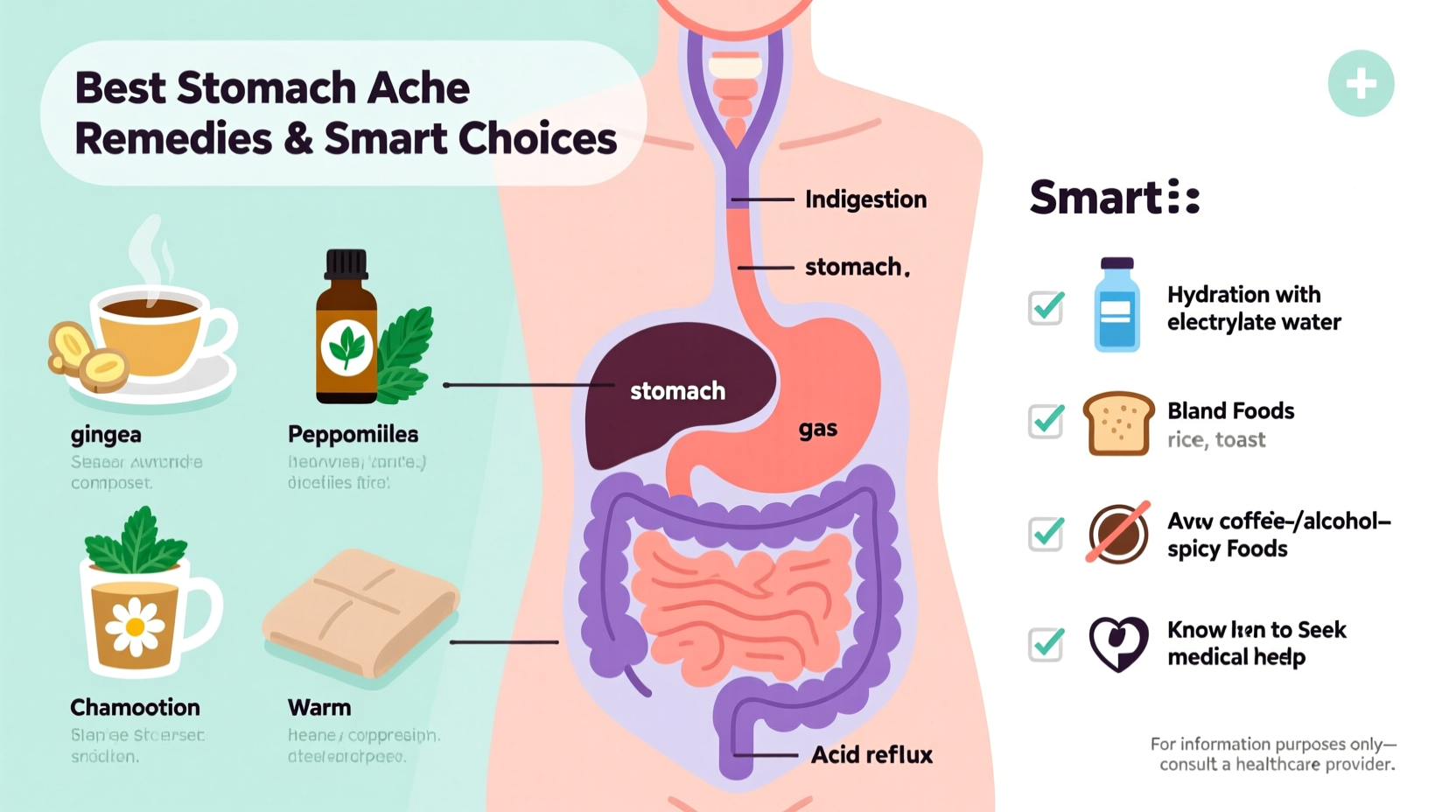
Effective Home Remedies Backed by Science
Many natural remedies offer gentle, effective relief without the risks of overmedication. When used appropriately, these can soothe discomfort and support healing.
Ginger Tea for Nausea and Motility
Ginger contains compounds like gingerol that reduce inflammation and enhance gastric emptying. Studies show it helps relieve nausea from various causes, including motion sickness and post-surgery recovery.
Peppermint Oil for Irritable Bowel Symptoms
Enteric-coated peppermint oil capsules have been clinically shown to reduce bloating, cramping, and pain in IBS patients by relaxing intestinal smooth muscle.
“Peppermint oil is one of the few complementary therapies with strong evidence for managing functional bowel disorders.” — Dr. Sarah Lin, Gastroenterology Specialist
Heat Therapy for Cramping
Applying a heating pad to the abdomen improves blood flow and relaxes contracted muscles, offering rapid relief from menstrual or gas-related cramps.
BRAT Diet During Recovery
The BRAT diet—bananas, rice, applesauce, and toast—is bland and low-fiber, making it ideal after vomiting or diarrhea. It helps firm stools and replenish energy gently.
Smart Dietary Choices to Prevent Recurrence
Prevention starts with what you eat—and when. Strategic food choices reduce irritation, support healthy digestion, and minimize triggers.
| Do | Avoid |
|---|---|
| Eat small, frequent meals to avoid overwhelming digestion | Large portions, especially late at night |
| Choose cooked vegetables over raw when sensitive | Raw cruciferous veggies (broccoli, cabbage) that produce gas |
| Drink herbal teas like chamomile or fennel | Carbonated drinks and alcohol |
| Stay hydrated with water or oral rehydration solutions | Sugary sodas or energy drinks |
| Chew food thoroughly to aid mechanical digestion | Eating quickly or on the go |
Probiotics and Gut Health
Regular intake of probiotics—found in yogurt, kefir, sauerkraut, or supplements—can stabilize gut flora and reduce episodes of bloating and irregularity. Strains like *Lactobacillus* and *Bifidobacterium* are particularly well-studied for digestive balance.
When to Seek Medical Help: A Step-by-Step Guide
Most stomach aches resolve within hours or a day. However, knowing when to escalate care is crucial. Follow this timeline if symptoms persist:
- Hour 0–6: Mild pain after eating? Try rest, hydration, and a warm compress. Sip clear fluids. Monitor progression.
- Hour 6–24: If pain continues but remains manageable, avoid solid foods temporarily. Introduce BRAT items if nausea subsides.
- After 24 hours: No improvement? Consider possible infection or food intolerance. Note fever, bloody stool, or inability to keep liquids down.
- After 48 hours: Persistent or worsening pain warrants medical consultation. Rule out appendicitis, gallstones, ulcers, or inflammatory bowel disease.
- Immediate red flags: Seek emergency care for severe localized pain (especially lower right abdomen), high fever, vomiting blood, or signs of dehydration (dizziness, dry mouth, reduced urination).
“Abdominal pain is a signal, not just a symptom. Listening to its pattern—timing, location, triggers—gives doctors vital clues.” — Dr. Rajiv Mehta, Internal Medicine Physician
Mini Case Study: Managing Chronic Bloating
Lena, a 34-year-old office worker, experienced recurring bloating and cramps after lunch. She assumed it was stress-related until she tracked her meals and noticed symptoms consistently followed salads with raw vegetables and beans. After eliminating high-FODMAP foods (fermentable carbs) and switching to steamed vegetables and lean proteins, her discomfort dropped by 80%. A follow-up with a dietitian confirmed mild IBS, and she began a structured reintroduction plan. Within six weeks, Lena identified specific triggers and regained confidence in her daily routine.
This case illustrates how self-monitoring and informed adjustments—not drastic diets—are often the key to sustainable relief.
Checklist: Smart Actions for Immediate Relief
- ✅ Stop eating and give your digestive system a break
- ✅ Sip room-temperature water or electrolyte solution slowly
- ✅ Apply a heating pad to the abdomen for cramps
- ✅ Try ginger tea or peppermint infusion (avoid peppermint if you have GERD)
- ✅ Lie on your left side to ease gas movement through the colon
- ✅ Avoid NSAIDs, caffeine, and carbonation
- ✅ Rest and practice slow, deep breathing to calm the nervous system
Frequently Asked Questions
Can I take antacids for every stomach ache?
Antacids work best for heartburn or excess stomach acid, not all types of abdominal pain. Using them unnecessarily may mask underlying issues or disrupt natural digestion. Reserve them for confirmed acid-related discomfort.
Is fasting good when I have a stomach ache?
Short-term fasting (12–24 hours) during acute illness like vomiting or diarrhea allows the gut to rest. However, prolonged fasting can weaken the intestinal lining and delay recovery. Reintroduce food gradually with easily digestible options.
Are there long-term risks to ignoring frequent stomach aches?
Yes. Recurrent pain may indicate conditions like gastritis, ulcers, celiac disease, or IBD. Untreated, these can lead to malnutrition, anemia, or increased risk of complications. Early assessment improves outcomes significantly.
Make Smarter Choices Starting Today
Relief from stomach aches doesn’t require extreme measures. Often, the wisest actions are the simplest: listen to your body, hydrate, choose gentle foods, and respond early. By combining time-tested home remedies with mindful habits, you empower yourself to manage discomfort effectively and reduce future occurrences. Don’t wait for pain to become chronic—start tracking your triggers, adjusting your diet, and prioritizing digestive wellness now.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?