For many patients and healthcare professionals alike, drawing blood should be a routine procedure. Yet, in some cases, it becomes unexpectedly challenging—requiring multiple attempts, causing discomfort, or even leading to failed collections. When veins are difficult to access, the experience can be frustrating and stressful for everyone involved. Understanding the underlying reasons behind hard-to-draw blood and learning practical strategies can make a significant difference in outcomes.
Whether you're a patient with a history of difficult draws or a phlebotomist seeking better techniques, this guide explores the physiological, environmental, and technical factors that contribute to problematic venipuncture—and what can be done to improve success rates.
Why Drawing Blood Can Be Difficult: Common Causes
Several factors—some within control, others not—can make veins elusive during blood collection. These range from anatomical variations to temporary conditions influenced by hydration, temperature, or medication.
- Small or collapsed veins: Naturally small vessels or those that collapse under pressure (common in elderly or chronically ill patients) resist needle insertion.
- Poor hydration: Dehydration reduces blood volume and makes veins less prominent and more likely to roll.
- Cold temperatures: Cold environments cause vasoconstriction, shrinking veins and making them harder to locate.
- Obesity: Excess subcutaneous fat can obscure vein visibility and increase depth, requiring greater precision.
- History of IV drug use: Repeated trauma to veins can lead to scarring, sclerosis, or complete closure of accessible sites.
- Chronic illness: Conditions like diabetes, kidney disease, or heart failure affect circulation and vessel integrity.
- Fear or anxiety: Stress-induced vasoconstriction tightens blood vessels, reducing their accessibility.
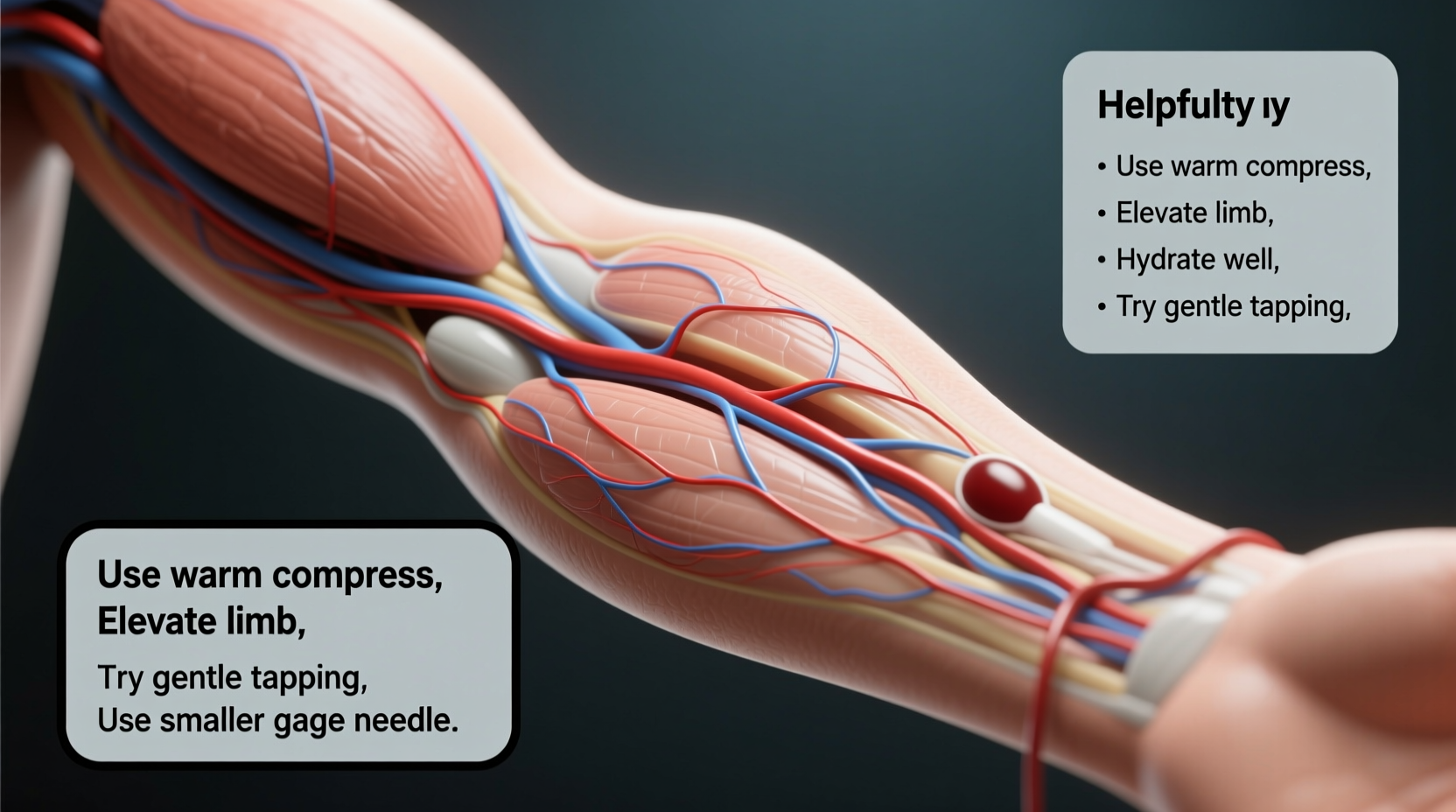
Techniques That Improve Venipuncture Success
Even when veins are difficult, skilled technique and proper preparation can significantly increase the chances of a successful first stick. The right approach combines patient cooperation, environmental adjustments, and clinical expertise.
Warming the Site
Applying a warm compress to the antecubital area for 3–5 minutes promotes vasodilation. This simple step can bring hidden veins to the surface, especially in cold-sensitive individuals.
Tourniquet Application
A properly placed tourniquet about 3–4 inches above the intended puncture site helps distend veins. However, leaving it on too long (>1 minute) can cause hemoconcentration or discomfort. Release immediately after blood flow is established.
Hydration and Timing
Scheduling blood draws earlier in the day often yields better results, as patients are typically more hydrated after overnight fasting (unless dehydrated). Encourage oral fluid intake before non-fasting tests whenever possible.
“Some patients come in with ‘rolling veins’ due to thin tissue or nervousness. A gentle touch, proper anchoring, and using the smallest effective needle can make all the difference.” — Sarah Lin, Certified Phlebotomy Technician, 12 years experience
Checklist: Preparing for a Successful Blood Draw
Use this actionable checklist to optimize conditions before venipuncture:
- Drink plenty of water 1–2 hours before the appointment (avoid caffeine).
- Wear short sleeves or clothing that allows easy arm access.
- Arrive relaxed—practice deep breathing if anxious.
- Inform the technician of past difficulties with blood draws.
- Request a warm towel or heating pad if arms feel cold.
- Keep the arm still and muscles relaxed during the procedure.
- Allow time between attempts; don’t rush repeat draws.
Do’s and Don’ts During Difficult Draws
| Do’s | Don’ts |
|---|---|
| Anchor the vein firmly by pulling skin taut below the site | Probe excessively once the needle is in—this increases pain and bruising |
| Use smaller gauge needles (23G) for fragile or small veins | Use excessive tourniquet pressure or leave it on too long |
| Try alternate sites: dorsal hand veins, forearm, or foot (if permitted) | Attempt multiple sticks in the same area without reassessing |
| Communicate openly—patients should report pain or burning | Ignore signs of nerve proximity (sharp pain radiating down arm) |
| Have backup equipment ready (pediatric tubes, syringes) | Rush the process; take time to reassess after a failed attempt |
Real-World Scenario: Managing a Challenging Case
Martha, a 72-year-old woman with type 2 diabetes and hypertension, had been referred for routine lab work prior to surgery. She mentioned previous issues with blood draws at her local clinic, often requiring two or more attempts.
Upon arrival, the phlebotomist noted her hands were cool and her veins appeared flat. Instead of proceeding immediately, the technician offered a warm towel and asked Martha to dangle her arm gently while sipping water. After five minutes, the cephalic vein became visible on her forearm.
The technician used a 23-gauge butterfly needle, anchored the vein securely, and successfully collected all required samples on the first try. Martha reported minimal discomfort and expressed relief at the improved experience.
This case illustrates how combining patient-centered care with technical adjustments can overcome common barriers—even in high-risk individuals.
Step-by-Step Guide for Patients Facing Difficult Veins
If you know you have tough veins, follow this timeline to prepare effectively:
- 24 Hours Before: Maintain normal fluid intake. Avoid alcohol, which contributes to dehydration.
- 1–2 Hours Before: Drink 16–20 oz of water. Eat a light meal unless fasting is required.
- En Route to Appointment: Dress warmly, especially in colder months. Bring a sweater to keep arms warm.
- At the Facility: Inform staff of past challenges. Request a warm compress or heating pad.
- During the Procedure: Breathe deeply, keep your arm relaxed, and avoid clenching your fist excessively.
- After the Draw: Apply firm pressure for at least 2 minutes to prevent bruising, especially if on blood thinners.
Frequently Asked Questions
Why do my veins “roll” when someone tries to draw blood?
Rolling occurs when the vein moves away from the needle upon insertion. This is common in people with loose skin, low body fat, or narrow veins. Anchoring the vein by stretching the skin tightly below the puncture site helps stabilize it.
Can medications affect how easy it is to draw blood?
Yes. Long-term steroid use can thin the skin and damage veins. Blood thinners increase bruising risk but don’t directly impact vein accessibility. Chemotherapy patients often develop scarred or fibrotic veins due to repeated IV treatments.
What should I do if the phlebotomist can’t get my blood after two tries?
Most facilities recommend stopping after two unsuccessful attempts and assigning a more experienced technician. It's reasonable to request a different provider or reschedule when better preparation (like hydration) can be achieved.
Conclusion: Turning Challenges into Confidence
Difficulty drawing blood doesn’t mean it’s impossible—just that extra care, patience, and strategy are needed. Whether you're a patient navigating chronic health conditions or a clinician striving for higher first-stick success rates, understanding the root causes and applying proven solutions leads to better outcomes.
Simple actions like staying hydrated, warming the site, and communicating openly can transform an anxious experience into a smooth one. For healthcare providers, refining technique and embracing adaptive tools ensures dignity and comfort for every patient, regardless of vein visibility.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?