Experiencing a heavier-than-normal menstrual flow can be more than just inconvenient—it can disrupt daily life, cause fatigue, and raise concerns about underlying health. While some variation in flow is normal, consistently soaking through pads or tampons every hour, passing large clots, or needing to double up on protection may signal something more serious. Understanding the reasons behind a heavy period—medically known as menorrhagia—is the first step toward effective management and improved well-being.
What Counts as a Heavy Period?
A typical menstrual cycle lasts 3 to 7 days, with blood loss averaging 30 to 40 milliliters (about 2 to 3 tablespoons) per cycle. A period is considered heavy if:
- You soak through a pad or tampon every hour for several consecutive hours.
- You pass blood clots larger than a quarter (about 2.5 cm).
- You need to use double protection (pad and tampon together) to control flow.
- You wake up at night to change sanitary products.
- Your period lasts longer than seven days.
- You feel fatigued or short of breath, which could indicate anemia.
If any of these apply regularly, it’s worth discussing with a healthcare provider. Heavy flow isn’t something you should simply “live with.”
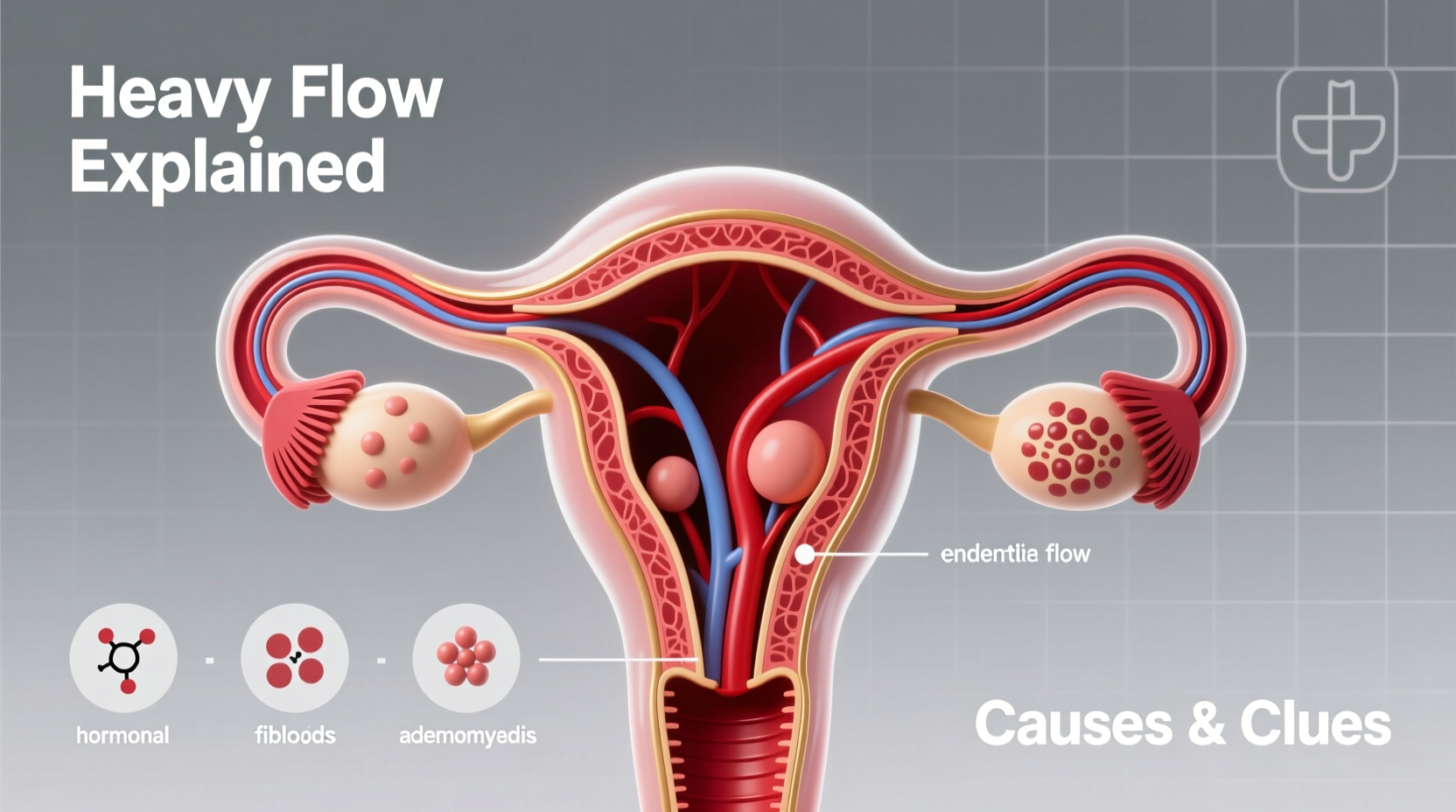
Common Causes of Heavy Menstrual Flow
Heavy periods can stem from a variety of factors, ranging from hormonal imbalances to structural issues in the reproductive system. Identifying the root cause is essential for proper treatment.
Hormonal Imbalance
The balance between estrogen and progesterone regulates your menstrual cycle. When ovulation doesn’t occur regularly—common during adolescence, perimenopause, or in conditions like polycystic ovary syndrome (PCOS)—the uterine lining may grow excessively, leading to heavier bleeding when it sheds.
Uterine Fibroids
Fibroids are noncancerous growths in the muscular wall of the uterus. They’re extremely common, affecting up to 70% of women by age 50. While many fibroids cause no symptoms, larger or multiple fibroids can increase menstrual flow and cause pelvic pressure or pain.
Adenomyosis
This condition occurs when endometrial tissue grows into the muscular wall of the uterus. The result is a swollen, tender uterus and often very heavy, painful periods. Adenomyosis is frequently underdiagnosed because its symptoms overlap with fibroids and endometriosis.
Endometrial Polyps
Polyps are small, benign growths on the inner lining of the uterus. They can cause irregular bleeding and heavy periods, especially in women over 40. Unlike fibroids, polyps originate from the endometrium and may require removal via hysteroscopy.
Use of Certain Intrauterine Devices (IUDs)
Copper IUDs, such as Paragard, are associated with heavier periods and increased cramping, particularly in the first few months after insertion. Hormonal IUDs, on the other hand, often reduce flow and are sometimes used to treat heavy bleeding.
Bleeding Disorders
Conditions like von Willebrand disease impair the blood’s ability to clot, leading to prolonged or excessive bleeding—not only during menstruation but also after injuries or surgeries. These disorders often go undiagnosed until heavy periods become unmanageable.
“Many women assume their heavy periods are normal because they’ve always been that way. But consistent flooding, fatigue, or missing work due to flow is not typical and deserves evaluation.” — Dr. Lena Patel, OB-GYN Specialist
When to See a Doctor
While occasional fluctuations in flow are normal, persistent heavy bleeding warrants medical attention. Left untreated, it can lead to iron-deficiency anemia, chronic fatigue, and reduced quality of life.
Seek care if you experience:
- Soaking through sanitary products hourly for two or more hours.
- Bleeding that lasts longer than eight days.
- Symptoms of anemia: dizziness, pale skin, weakness, or rapid heartbeat.
- Pain severe enough to interfere with daily activities.
- Postmenopausal bleeding.
Diagnostic Steps Your Doctor May Take
- Medical History Review: Including cycle patterns, family history, medications, and symptoms.
- Physical and Pelvic Exam: To check for uterine enlargement or tenderness.
- Blood Tests: To assess for anemia and thyroid function.
- Ultrasound: Transvaginal imaging to visualize the uterus, ovaries, and detect fibroids or polyps.
- Endometrial Biopsy: Sampling uterine lining tissue, especially in women over 45 or with risk factors for cancer.
- Hysteroscopy: Direct visualization of the uterine cavity, often combined with biopsy or polyp removal.
Treatment Options Based on Cause
Treatment depends on the underlying cause, severity, age, and whether you plan to have children. Options range from medication to minimally invasive procedures.
| Condition | Treatment Options | Effectiveness for Reducing Flow |
|---|---|---|
| Hormonal imbalance / PCOS | Combined oral contraceptives, progestin therapy, metformin | High – often reduces flow by 40–60% |
| Uterine fibroids | Hormonal IUD, GnRH agonists, myomectomy, uterine artery embolization | Moderate to high – depends on size and location |
| Adenomyosis | Hormonal IUD, NSAIDs, endometrial ablation, hysterectomy | Moderate – ablation or removal offers long-term relief |
| Bleeding disorders | Tranexamic acid, desmopressin, hormone therapy | High – especially with targeted clotting support |
| IUD-related | Switch to hormonal IUD or alternative contraception | Very high – hormonal IUDs reduce flow significantly |
Real-Life Example: Sarah’s Journey to Diagnosis
Sarah, a 34-year-old teacher, had endured heavy periods since her early twenties. She routinely changed super tampons every hour and missed work twice a year due to fatigue. She assumed it was normal until she fainted during a school event. Blood tests revealed severe iron-deficiency anemia. An ultrasound showed multiple fibroids, one measuring 6 cm. After consulting a gynecologist, she opted for a minimally invasive myomectomy. Within three months, her flow normalized, energy returned, and she no longer needed iron supplements. Her story underscores how normalization of symptoms delays care—and how timely intervention transforms lives.
Self-Care and Lifestyle Strategies
While medical treatment addresses the root cause, daily habits can ease symptoms and support recovery.
- Eat iron-rich foods (spinach, lentils, red meat) to combat anemia.
- Stay hydrated and rest during peak flow days.
- Use high-absorbency period products designed for heavy flow.
- Apply heat to relieve cramping and improve circulation.
- Consider supplements like vitamin C (enhances iron absorption) or omega-3s (may reduce inflammation).
Frequently Asked Questions
Can stress make my period heavier?
Indirectly, yes. Chronic stress disrupts hormone balance, potentially leading to irregular cycles and heavier bleeding. Managing stress through sleep, exercise, and mindfulness may help regulate flow over time.
Is a heavy period a sign of cancer?
Not usually, but abnormal bleeding—especially after menopause or in women over 45—requires evaluation to rule out endometrial cancer. Risk factors include obesity, unopposed estrogen exposure, and certain genetic syndromes.
Will a hysterectomy stop heavy periods?
Yes, removing the uterus ends menstrual bleeding entirely. It’s typically reserved for cases where other treatments fail or aren’t suitable. Less invasive options like endometrial ablation can also provide lasting relief without removing the uterus.
Take Control of Your Cycle
Heavy menstrual flow is more than a monthly inconvenience—it’s a signal from your body that something may be off balance. Whether due to fibroids, hormonal shifts, or an undiagnosed condition, effective solutions exist. You don’t have to endure fatigue, anxiety about leaks, or missed moments. By tracking symptoms, seeking timely care, and exploring treatment options, you can regain comfort and confidence in your daily life.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?