Elevated intraocular pressure (IOP), commonly referred to as high eye pressure, is a key factor in the development of glaucoma—one of the leading causes of irreversible blindness worldwide. While high eye pressure doesn’t always lead to vision loss, it significantly increases the risk. Understanding what causes it, recognizing the dangers, and knowing how to manage it are essential steps in preserving long-term eye health. This article explores the underlying mechanisms, associated risks, and practical strategies to lower and control eye pressure effectively.
What Causes High Eye Pressure?
Intraocular pressure is determined by the balance between the production and drainage of aqueous humor—a clear fluid that nourishes the front part of the eye. When this fluid doesn’t drain properly, pressure builds up inside the eye. Several factors can disrupt this balance:
- Blocked or inefficient drainage system: The trabecular meshwork, responsible for draining fluid, may become clogged or less efficient with age.
- Excessive fluid production: In rare cases, the ciliary body produces too much aqueous humor.
- Anatomical variations: Narrow drainage angles, common in people of Asian descent, increase the risk of acute angle-closure glaucoma.
- Medications: Long-term use of corticosteroids—especially eye drops, inhalers, or oral forms—can elevate IOP.
- Systemic conditions: Diabetes, hypertension, and sleep apnea have been linked to altered ocular perfusion and pressure regulation.
Risks Associated with Elevated Eye Pressure
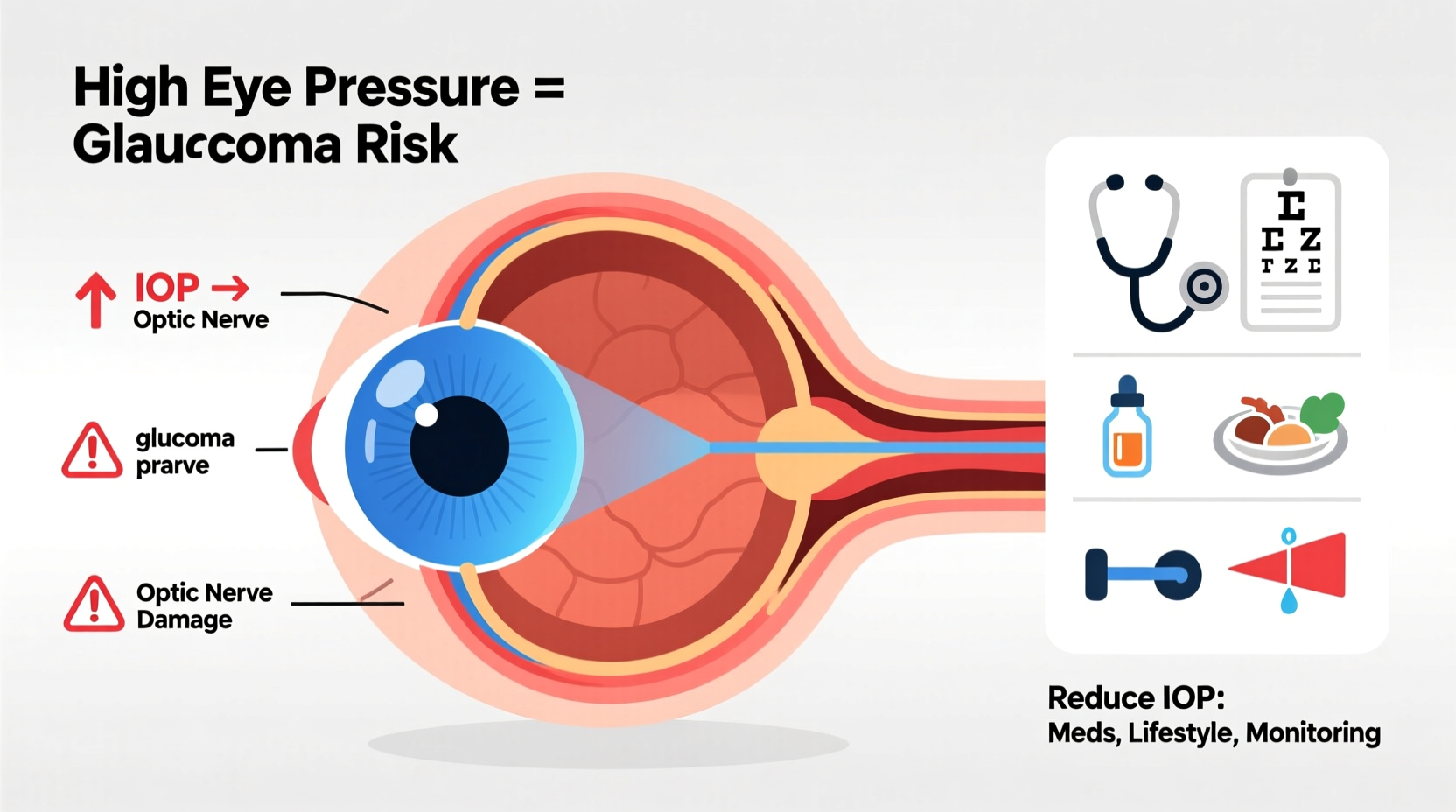
Persistent high IOP damages the optic nerve, which transmits visual information from the retina to the brain. Unlike other tissues, optic nerve fibers do not regenerate. Once damaged, the resulting vision loss is permanent.
The primary condition linked to high eye pressure is glaucoma. There are two main types:
- Open-angle glaucoma: The most common form, progressing slowly with no early symptoms. Peripheral vision deteriorates first, often unnoticed until significant damage has occurred.
- Angle-closure glaucoma: Less common but more urgent. It occurs when the iris blocks the drainage angle suddenly, causing rapid pressure spikes. Symptoms include severe eye pain, headache, nausea, blurred vision, and halos around lights.
Beyond glaucoma, chronically high eye pressure may contribute to reduced blood flow to the optic nerve and retinal ganglion cell death. Individuals with thin corneas, a family history of glaucoma, or African or Hispanic ancestry are at higher risk.
“Even without glaucoma, consistently elevated IOP should be taken seriously—it’s one of the few modifiable risk factors we have for preventing optic nerve damage.” — Dr. Alan Kim, Ophthalmologist and Glaucoma Specialist
How to Reduce High Eye Pressure: Proven Strategies
The goal of managing high eye pressure is to preserve vision by lowering IOP to a safe range, typically between 12–22 mmHg, though target levels vary per individual. A combination of medical treatment, lifestyle adjustments, and regular monitoring offers the best outcomes.
1. Use Prescribed Medications
Eye drops are the first-line treatment for reducing IOP. They work by either decreasing fluid production or improving drainage. Common classes include:
- Prostaglandin analogs (e.g., latanoprost)
- Beta-blockers (e.g., timolol)
- Alpha agonists (e.g., brimonidine)
- Carbonic anhydrase inhibitors (e.g., dorzolamide)
Consistency is critical—missing doses can cause pressure fluctuations that harm the optic nerve over time.
2. Adopt Beneficial Lifestyle Habits
Diet, exercise, and daily routines play a surprisingly strong role in eye pressure regulation.
| Practice | Benefit | Evidence Level |
|---|---|---|
| Aerobic exercise (30 min, 4x/week) | Lowers IOP by 15–20% | Strong clinical support |
| Reduced caffeine intake | Prevents temporary spikes | Moderate evidence |
| Dark green leafy vegetables | Rich in nitrates; improve blood flow | Emerging research |
| Sleeping with head elevated | Reduces nocturnal pressure rise | Clinical observation |
3. Avoid Pressure-Increasing Behaviors
Certain everyday actions can inadvertently raise eye pressure:
- Straining during bowel movements (Valsalva maneuver)
- Wearing tight neckwear that restricts blood flow
- Long periods of inverted yoga poses (e.g., headstands)
- Excessive fluid consumption in short intervals
Real-Life Example: Managing Pressure Through Lifestyle Change
James, a 58-year-old teacher, was diagnosed with ocular hypertension during a routine eye exam. His IOP readings were consistently above 24 mmHg, though he had no vision loss. His ophthalmologist recommended starting eye drops, but James wanted to explore natural methods first.
Over six months, he incorporated 30 minutes of brisk walking five times a week, eliminated energy drinks, increased his intake of spinach and kale, and began using a wedge pillow to elevate his head at night. At his follow-up, his average IOP dropped to 19 mmHg. While he still required occasional medication during seasonal allergies, his improved habits significantly reduced his reliance on drops.
This case illustrates how proactive lifestyle changes can complement medical treatment and sometimes delay or reduce the need for pharmaceutical intervention.
Step-by-Step Guide to Monitoring and Reducing Eye Pressure
Follow this timeline to take control of your eye health:
- Week 1: Schedule a comprehensive eye exam including tonometry, visual field testing, and optic nerve imaging.
- Week 2: Begin tracking habits—note caffeine, fluid intake, exercise, and sleep patterns.
- Month 1: Start moderate aerobic activity (e.g., walking, cycling) 4–5 times weekly.
- Month 2: Adjust diet to include potassium-rich fruits, leafy greens, and omega-3 sources like fatty fish or flaxseed.
- Ongoing: Take prescribed medications as directed. Attend follow-ups every 3–6 months, or as advised.
Frequently Asked Questions
Can high eye pressure go back to normal on its own?
Occasionally, temporary spikes caused by stress, caffeine, or posture may resolve quickly. However, chronic elevation rarely corrects itself without intervention. Regular monitoring and treatment are necessary to prevent damage.
Is high eye pressure the same as glaucoma?
No. High eye pressure (ocular hypertension) means elevated IOP without optic nerve damage. Glaucoma involves both high pressure and structural or functional damage to the optic nerve. Not everyone with high pressure develops glaucoma, but they are at increased risk.
Are there natural supplements that help lower eye pressure?
Some studies suggest Ginkgo biloba, magnesium, and vitamin B12 may support optic nerve health, but they don’t directly lower IOP. Always consult your doctor before starting supplements, especially if you’re on medication.
Conclusion: Protect Your Vision Before Damage Occurs
High eye pressure is a silent threat—one that gives no warning until vision begins to fade. But unlike many health issues, it can be detected early and managed effectively. Whether through medication, lifestyle changes, or a combination of both, reducing intraocular pressure is one of the most powerful tools available to prevent glaucoma-related blindness.
Your eyes don’t come with a backup pair. Start taking action today: get regular eye checkups, adopt eye-friendly habits, and stay informed. Small changes now can preserve your sight for decades to come.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?